Abstract
Objective To study the accuracy of BruxChecker in assessing sleep bruxism.
Methods In total, 35 subjects were categorised into two groups: 16 subjects with sleep bruxism (SB) and 19 with no sleep bruxism (NSB). Each participant wore a BruxChecker for 14 consecutive nights. Wear patterns were evaluated on nights one, seven and fourteen, focusing on abrasion (wear without perforation) and perforation areas. Clinical assessment was the reference standard, with BruxChecker perforation indicating a positive result for SB.
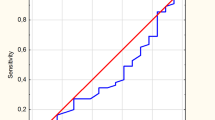
Results The mean age was 28.0 ± 9.3 years (SB) and 21.6 ± 1.7 years (NSB). The SB group exhibited significantly larger abraded areas on the BruxChecker compared to the NSB group on all three nights. Additionally, the SB group had significantly greater perforation on the fourteenth night. The diagnostic performance of the BruxChecker varied over time. On the first night, sensitivity and specificity were 31% and 84%, respectively. By the seventh night, these values were 63% and 42%, respectively. On the fourteenth night, sensitivity increased to 94%, with specificity decreased to 32%.
Conclusions BruxChecker may offer a practical and relatively cost-effective tool for assessing sleep bruxism in individuals with probable sleep bruxism. Its diagnostic performance appeared to improve when used over 14 consecutive nights, though its accuracy remains limited compared to standard methods.
Key points
-
The BruxChecker offers a comfortable, non-invasive way to assess sleep bruxism. It presents a more affordable option compared to gold-standard assessments like polysomnography, which can be expensive and resource-intensive.
-
The device can help detect signs of bruxism early, potentially preventing long-term damage to teeth, jaw muscles, and joints.
-
Dentists and clinicians can use the data from BruxChecker to better decide whether further investigation or treatment is necessary.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The data that supports the findings of this study are available from the corresponding author upon reasonable request.
References
Verhoeff M C, Lobbezoo F, Ahlberg J et al. Updating the bruxism definitions: report of an international consensus meeting. J Oral Rehabil 2025; 52: 1335–1342.
Thomas D C, Manfredini D, Patel J et al. Sleep bruxism: the past, the present, and the future-evolution of a concept. J Am Dent Assoc 2024; 155: 329–343.
Manfredini D, Colonna A, Bracci A, Lobbezoo F. Bruxism: a summary of current knowledge on aetiology, assessment and management. Oral Surg 2020; 13: 358–370.
Svensson P, Lavigne G. Clinical bruxism semantics beyond academic debates: Normo- and patho-bruxism as a new proposal. J Oral Rehabil 2020; 47: 547–548.
Manfredini D, Ahlberg J, Wetselaar P, Svensson P, Lobbezoo F. The bruxism construct: from cut-off points to a continuum spectrum. J Oral Rehabil 2019; 46: 991–997.
Carra M C, Huynh N, Lavigne G. Sleep bruxism: a comprehensive overview for the dental clinician interested in sleep medicine. Dent Clin North Am 2012; 56: 387–413.
Nashed A, Lanfranchi P, Rompré P et al. Sleep bruxism is associated with a rise in arterial blood pressure. Sleep 2012; 35: 529–536.
Lavigne G J, Khoury S, Abe S, Yamaguchi T, Raphael K. Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil 2008; 35: 476–494.
Khoury S, Carra M C, Huynh N, Montplaisir J, Lavigne G J. Sleep bruxism – tooth grinding prevalence, characteristics and familial aggregation: a large cross-sectional survey and polysomnographic validation. Sleep 2016; 39: 2049–2056.
Oporto G H 5th, Bornhardt T, Iturriaga V, Salazar L A. Genetic polymorphisms in the serotonergic system are associated with circadian manifestations of bruxism. J Oral Rehabil 2016; 43: 805–812.
Bertazzo-Silveira E, Kruger C M, Porto De Toledo I et al. Association between sleep bruxism and alcohol, caffeine, tobacco, and drug abuse. J Am Dent Assoc 2016; 147: 859–866.
Carra M C, Huynh N, Morton P et al. Prevalence and risk factors of sleep bruxism and wake-time tooth clenching in a 7- to 17-yr-old population. Eur J Oral Sci 2011; 119: 386–394.
Yap A U, Tan M W Y, Tan S H X, Chua A P. Sleep bruxism events: an epiphenomenon of severe obstructive sleep apnea? Clin Oral Investig 2023; 27: 4633–4642.
Rees J S, Somi S. A guide to the clinical management of attrition. Br Dent J 2018; 224: 319–323.
Ommerborn M A, Schneider C, Giraki M et al. In vivo evaluation of noncarious cervical lesions in sleep bruxism subjects. J Prosthet Dent 2007; 98: 150–158.
Ohlmann B, Waldecker M, Leckel M et al. Correlations between sleep bruxism and temporomandibular disorders. J Clin Med 2020; 9: 611.
Van Selms M K A, Visscher C M, Naeije M, Lobbezoo F. Bruxism and associated factors among Dutch adolescents. Community Dent Oral Epidemiol 2013; 41: 353–363.
Koyano K, Tsukiyama Y, Ichiki R, Kuwata T. Assessment of bruxism in the clinic. J Oral Rehabil 2008; 35: 495–508.
Manfredini D, Ahlberg J, Aarab G et al. Towards a Standardized Tool for the Assessment of Bruxism (STAB) – overview and general remarks of a multidimensional bruxism evaluation system. J Oral Rehabil 2020; 47: 549–556.
Lobbezoo F, Ahlberg J, Verhoeff M C et al. The bruxism screener (BruxScreen): development, pilot testing and face validity. J Oral Rehabil 2024; 51: 59–66.
Lavigne G, Manzini C, Huynh N. Sleep bruxism. In Kryger M H, Roth T, Dement W C (eds) Principles and Practice of Sleep Medicine. 5th ed. Missouri: Elsevier, 2011.
Ommerborn M A, Giraki M, Schneider C et al. A new analyzing method for quantification of abrasion on the Bruxcore device for sleep bruxism diagnosis. J Orofac Pain 2005; 19: 232–238.
Pierce C J, Gale E N. Methodological considerations concerning the use of Bruxcore Plates to evaluate nocturnal bruxism. J Dent Res 1989; 68: 1110–1114.
Shochat T, Gavish A, Arons E et al. Validation of the BiteStrip screener for sleep bruxism. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 2007; DOI: 10.1016/j.tripleo.2007.03.009..
Tokiwa O, Park B-K, Takezawa Y, Takahashi Y, Sasaguri K, Sato S. Relationship of tooth grinding pattern during sleep bruxism and dental status. Cranio 2008; 26: 287–293.
Onodera K, Kawagoe T, Sasaguri K, Protacio-Quismundo C, Sato S. The use of a bruxchecker in the evaluation of different grinding patterns during sleep bruxism. Cranio 2006; 24: 292–299.
Sugimoto K, Yoshimi H, Sasaguri K, Sato S. Occlusion factors influencing the magnitude of sleep bruxism activity. Cranio 2011; 29: 127–137.
Huynh N, Lavigne G J, Lanfranchi P A, Montplaisir J Y, de Champlain J. The effect of 2 sympatholytic medications – propranolol and clonidine – on sleep bruxism: experimental randomized controlled studies. Sleep 2006; 29: 307–316.
Saletu A, Parapatics S, Anderer P, Matejka M, Saletu B. Controlled clinical, polysomnographic and psychometric studies on differences between sleep bruxers and controls and acute effects of clonazepam as compared with placebo. Eur Arch Psychiatry Clin Neurosci 2010; 260: 163–174.
Ahlberg J, Piirtola M, Lobbezoo F et al. Correlates and genetics of self-reported sleep and awake bruxism in a nationwide twin cohort. J Oral Rehabil 2020; 47: 1110–1119.
Lavigne G J, Montplaisir J Y. Restless legs syndrome and sleep bruxism: prevalence and association among Canadians. Sleep 1994; 17: 739–743.
Wetselaar P, Vermaire E J H, Lobbezoo F, Schuller A A. The prevalence of awake bruxism and sleep bruxism in the Dutch adult population. J Oral Rehabil 2019; 46: 617–623.
Brandão de Almeida A, Rodrigues R S, Simão C, de Araújo R P, Figueiredo J. Prevalence of sleep bruxism reported by parents/caregivers in a portuguese pediatric dentistry service: a retrospective study. Int J Environ Res Public Health 2022; 19: 7823.
Strausz T, Strausz S, Jones S E et al. A two-sample mendelian randomization study of neuroticism and sleep bruxism. J Dent Res 2024; 103: 980–987.
Huynh N, Fabbro C D. Sleep bruxism in children and adolescents – a scoping review. J Oral Rehabil 2024; 51: 103–109.
Martynowicz H, Lavigne G, Kato T et al. A case-control study on the effect of rhythmic masticatory muscle activity (RMMA) clusters on sleep fragmentation and severity of orofacial muscle pain in sleep bruxism. J Sleep Res 2024; DOI: 10.1111/jsr.14072.
Lavigne G J, Kato T, Kolta A, Sessle B J. Neurobiological mechanisms involved in sleep bruxism. Crit Rev Oral Biol Med 2003; 14: 30–46.
Clark G T, Beemsterboer P L, Solberg W K, Rugh J D. Nocturnal electromyographic evaluation of myofascial pain dysfunction in patients undergoing occlusal splint therapy. J Am Dent Assoc 1979; 99: 607–611.
Parodi S, Verda D, Bagnasco F, Muselli M. The clinical meaning of the area under a receiver operating characteristic curve for the evaluation of the performance of disease markers. Epidemiol Health 2022; DOI: 10.4178/epih.e2022088.
Lobbezoo F, Ahlberg J, Raphael K G et al. International consensus on the assessment of bruxism: report of a work in progress. J Oral Rehabil 2018; 45: 837–844.
Martynowicz H, Michalek-Zrabkowska M, Gac P et al. Performance evaluation of portable respiratory polygraphy for assessing sleep bruxism in adults. J Oral Rehabil 2024; 51: 1862–1871.
Acknowledgements
We are grateful for the support provided by the Faculty of Dentistry, Prince of Songkla University, including the provision of facilities, personnel, and research funding. Finally, we would like to thank all research participants for their valuable contributions to this study.
Funding
This research was funded by the Faculty of Dentistry, Prince of Songkla University, Thailand, with no external funding. The BruxChecker® foils used in this study were provided by Scheu-Dental GmbH (Iserlohn, Germany). The source of funding had no influence on the design, data collection, analysis, interpretation, or the decision to submit the manuscript for publication of this study.
Author information
Authors and Affiliations
Contributions
The authors confirm contribution to the paper as follows: study conception and design: PY, ST, WS, SK, WN, PL and PC; data collection: PY, ST, WS, SK, WN, PL and PC; analysis and interpretation of results: PY, ST, WS, SK, WN, PL and PC; draft manuscript: PY and ST; reviewed and intellectual contribution: ST and PC. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
The authors have no conflict of interest related to this publication. Ethical approval for the study was granted by the Faculty of Dentistry, Prince of Songkla University (EC5701-02-J-LR). Participants in this study signed an informed consent form before taking part.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yakkaphan, P., Tangpothitham, S., Srisomphot, W. et al. Accuracy of the BruxChecker oral device for the assessment of sleep bruxism. Br Dent J (2026). https://doi.org/10.1038/s41415-025-9203-4
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41415-025-9203-4