Abstract
Background
This study aims to develop a stacking model for accurately predicting axillary lymph node (ALN) response to neoadjuvant chemotherapy (NAC) using longitudinal MRI in breast cancer.
Methods
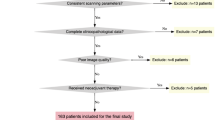
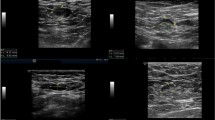
We included patients with node-positive breast cancer who received NAC following surgery from January 2012 to June 2022. We collected MRIs before and after NAC, and extracted radiomics features from the tumour, peritumour, and ALN regions. The Mann–Whitney U test, least absolute shrinkage and selection operator, and Boruta algorithm were used to select features. We utilised machine learning techniques to develop three single-modality models and a stacking model for predicting ALN response to NAC.
Results
This study consisted of a training cohort (n = 277), three external validation cohorts (n = 313, 164, and 318), and a prospective cohort (n = 81). Among the 1153 patients, 60.62% achieved ypN0. The stacking model achieved excellent AUCs of 0.926, 0.874, and 0.862 in the training, external validation, and prospective cohort, respectively. It also showed lower false-negative rates (FNRs) compared to radiologists, with rates of 14.40%, 20.85%, and 18.18% (radiologists: 40.80%, 50.49%, and 63.64%) in three cohorts. Additionally, there was a significant difference in disease-free survival between high-risk and low-risk groups (p < 0.05).
Conclusions
The stacking model can accurately predict ALN status after NAC in breast cancer, showing a lower false-negative rate than radiologists.
Trial registration number
The clinical trial numbers were NCT03154749 and NCT04858529.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated and analysed during the current study are available from the corresponding author Kun Wang, upon reasonable request.
References
Wolmark N, Wang J, Mamounas E, Bryant J, Fisher B. Preoperative chemotherapy in patients with operable breast cancer: nine-year results from National Surgical Adjuvant Breast and Bowel Project B-18. J Natl Cancer Inst Monogr. 2001;30:96–102.
Bear HD, Anderson S, Brown A, Smith R, Mamounas EP, Fisher B, et al. The effect on tumor response of adding sequential preoperative docetaxel to preoperative doxorubicin and cyclophosphamide: preliminary results from National Surgical Adjuvant Breast and Bowel Project Protocol B-27. J Clin Oncol. 2003;21:4165–74.
Pilewskie M, Morrow M. Axillary nodal management following neoadjuvant chemotherapy: a review. JAMA Oncol. 2017;3:549–55.
Boughey JC, Suman VJ, Mittendorf EA, Ahrendt GM, Wilke LG, Taback B, et al. Factors affecting sentinel lymph node identification rate after neoadjuvant chemotherapy for breast cancer patients enrolled in ACOSOG Z1071 (Alliance). Ann Surg. 2015;261:547–52.
Kuehn T, Bauerfeind I, Fehm T, Fleige B, Hausschild M, Helms G, et al. Sentinel-lymph-node biopsy in patients with breast cancer before and after neoadjuvant chemotherapy (SENTINA): a prospective, multicentre cohort study. Lancet Oncol. 2013;14:609–18.
Boileau JF, Poirier B, Basik M, Holloway CM, Gaboury L, Sideris L, et al. Sentinel node biopsy after neoadjuvant chemotherapy in biopsy-proven node-positive breast cancer: the SN FNAC study. J Clin Oncol. 2015;33:258–64.
Caudle AS, Yang WT, Krishnamurthy S, Mittendorf EA, Black DM, Gilcrease MZ, et al. Improved Axillary Evaluation Following Neoadjuvant Therapy for Patients With Node-Positive Breast Cancer Using Selective Evaluation of Clipped Nodes: Implementation of Targeted Axillary Dissection. J Clin Oncol. 2016;34:1072–8.
Kuemmel S, Heil J, Rueland A, Seiberling C, Harrach H, Schindowski D, et al. A Prospective, Multicenter Registry Study to Evaluate the Clinical Feasibility of Targeted Axillary Dissection (TAD) in Node-positive Breast Cancer Patients. Ann Surg. 2022;276:e553–e62.
Swarnkar PK, Tayeh S, Michell MJ, Mokbel K. The evolving role of marked lymph node biopsy (MLNB) and targeted axillary dissection (TAD) after neoadjuvant chemotherapy (NACT) for node-positive breast cancer: systematic review and pooled analysis. Cancers. 2021;13:1539.
Vila J, Mittendorf EA, Farante G, Bassett RL, Veronesi P, Galimberti V, et al. Nomograms for Predicting Axillary Response to Neoadjuvant Chemotherapy in Clinically Node-Positive Patients with Breast Cancer. Ann Surg Oncol. 2016;23:3501–9.
Murphy BL, Hoskin TL, Heins CDN, Habermann EB, Boughey JC. Preoperative Prediction of Node-Negative Disease After Neoadjuvant Chemotherapy in Patients Presenting with Node-Negative or Node-Positive Breast Cancer. Ann Surg Oncol. 2017;24:2518–25.
Schipper RJ, Moossdorff M, Nelemans PJ, Nieuwenhuijzen GA, de Vries B, Strobbe LJ, et al. A model to predict pathologic complete response of axillary lymph nodes to neoadjuvant chemo(immuno)therapy in patients with clinically node-positive breast cancer. Clin Breast Cancer. 2014;14:315–22.
Skarping I, Förnvik D, Zackrisson S, Borgquist S, Rydén L. Predicting pathological axillary lymph node status with ultrasound following neoadjuvant therapy for breast cancer. Breast Cancer Res Treat. 2021;189:131–44.
Al-Hattali S, Vinnicombe SJ, Gowdh NM, Evans A, Armstrong S, Adamson D, et al. Breast MRI and tumour biology predict axillary lymph node response to neoadjuvant chemotherapy for breast cancer. Cancer Imaging. 2019;19:91.
Kim R, Chang JM, Lee HB, Lee SH, Kim SY, Kim ES, et al. Predicting Axillary Response to Neoadjuvant Chemotherapy: Breast MRI and US in Patients with Node-Positive Breast Cancer. Radiology. 2019;293:49–57.
Huang X, Shi Z, Mai J, Liu C, Liu C, Chen S. An MRI-based scoring system for preoperative prediction of axillary response to neoadjuvant chemotherapy in node-positive breast cancer: a multicenter retrospective study. Acad Radiol. 2022:1257–1269.
Zhu T, Lin X, Zhang T, Li W, Gao H, Yang C, et al. A model incorporating axillary tail position on mammography for preoperative prediction of non-sentinel lymph node metastasis in patients with initial cn+ breast cancer after neoadjuvant chemotherapy. Acad Radiol. 2022;29:e271–e8.
Slanetz PJ, Moy L, Baron P, diFlorio RM, Green ED, Heller SL, et al. ACR Appropriateness Criteria(®) monitoring response to neoadjuvant systemic therapy for breast cancer. J Am Coll Radiology: JACR. 2017;14:S462–s75.
You S, Kang DK, Jung YS, An YS, Jeon GS, Kim TH. Evaluation of lymph node status after neoadjuvant chemotherapy in breast cancer patients: comparison of diagnostic performance of ultrasound, MRI and 18F-FDG PET/CT. Br J Radiol. 2015;88:20150143.
Javid S, Segara D, Lotfi P, Raza S, Golshan M. Can breast MRI predict axillary lymph node metastasis in women undergoing neoadjuvant chemotherapy. Ann Surg Oncol. 2010;17:1841–6.
Hieken TJ, Boughey JC, Jones KN, Shah SS, Glazebrook KN. Imaging response and residual metastatic axillary lymph node disease after neoadjuvant chemotherapy for primary breast cancer. Ann Surg Oncol. 2013;20:3199–204.
Bitencourt AGV, Gibbs P, Rossi Saccarelli C, Daimiel I, Lo Gullo R, Fox MJ, et al. MRI-based machine learning radiomics can predict HER2 expression level and pathologic response after neoadjuvant therapy in HER2 overexpressing breast cancer. EBioMedicine. 2020;61:103042.
Yu Y, He Z, Ouyang J, Tan Y, Chen Y, Gu Y, et al. Magnetic resonance imaging radiomics predicts preoperative axillary lymph node metastasis to support surgical decisions and is associated with tumor microenvironment in invasive breast cancer: a machine learning, multicenter study. EBioMedicine. 2021;69:103460.
Drukker K, Edwards A, Doyle C, Papaioannou J, Kulkarni K, Giger ML. Breast MRI radiomics for the pretreatment prediction of response to neoadjuvant chemotherapy in node-positive breast cancer patients. J Med imaging. 2019;6:034502.
Minarikova L, Bogner W, Pinker K, Valkovič L, Zaric O, Bago-Horvath Z, et al. Investigating the prediction value of multiparametric magnetic resonance imaging at 3 T in response to neoadjuvant chemotherapy in breast cancer. Eur Radiol. 2017;27:1901–11.
Pereira NP, Curi C, Osório C, Marques EF, Makdissi FB, Pinker K, et al. Diffusion-weighted magnetic resonance imaging of patients with breast cancer following neoadjuvant chemotherapy provides early prediction of pathological response - a prospective study. Sci Rep. 2019;9:16372.
Eun NL, Kang D, Son EJ, Park JS, Youk JH, Kim JA, et al. Texture analysis with 3.0-T MRI for association of response to neoadjuvant chemotherapy in breast cancer. Radiology. 2020;294:31–41.
Nadrljanski MM, Milosevic ZC. Tumor texture parameters of invasive ductal breast carcinoma in neoadjuvant chemotherapy: early identification of non-responders on breast MRI. Clin imaging. 2020;65:119–23.
Tudorica A, Oh KY, Chui SY, Roy N, Troxell ML, Naik A, et al. Early prediction and evaluation of breast cancer response to neoadjuvant chemotherapy using quantitative DCE-MRI. Transl Oncol. 2016;9:8–17.
Dogan BE, Yuan Q, Bassett R, Guvenc I, Jackson EF, Cristofanilli M, et al. Comparing the performances of magnetic resonance imaging size vs pharmacokinetic parameters to predict response to neoadjuvant chemotherapy and survival in patients with breast cancer. Curr Probl Diagn Radiol. 2019;48:235–40.
Liu Z, Li Z, Qu J, Zhang R, Zhou X, Li L. et al. Radiomics of multiparametric MRI for pretreatment prediction of pathologic complete response to neoadjuvant chemotherapy in breast cancer: a multicenter study.Clin Cancer Res. 2019;25:3538–47.
Han L, Zhu Y, Liu Z, Yu T, He C, Jiang W, et al. Radiomic nomogram for prediction of axillary lymph node metastasis in breast cancer. Eur Radiol. 2019;29:3820–9.
Santucci D, Faiella E, Cordelli E, Sicilia R, de Felice C, Zobel BB. 3T MRI-Radiomic Approach to Predict for Lymph Node Status in Breast Cancer Patients. Cancers. 2021;13:2228.
Schipper RJ, Paiman ML, Beets-Tan RG, Nelemans PJ, de Vries B, Heuts EM, et al. Diagnostic Performance of Dedicated Axillary T2- and Diffusion-weighted MR Imaging for Nodal Staging in Breast Cancer. Radiology. 2015;275:345–55.
Schipper RJ, Smidt ML, van Roozendaal LM, Castro CJ, de Vries B, Heuts EM, et al. Noninvasive nodal staging in patients with breast cancer using gadofosveset-enhanced magnetic resonance imaging: a feasibility study. Invest Radiol. 2013;48:134–9.
Byon JH, Park YV, Yoon JH, Moon HJ, Kim EK, Kim MJ, et al. Added value of MRI for invasive breast cancer including the entire axilla for evaluation of high-level or advanced axillary lymph node metastasis in the Post-ACOSOG Z0011 trial era. Radiology. 2021;300:46–54.
Crombé A, Périer C, Kind M, De Senneville BD, Le Loarer F, Italiano A, et al. T(2) -based MRI delta-radiomics improve response prediction in soft-tissue sarcomas treated by neoadjuvant chemotherapy. J Magn Reson Imaging: JMRI. 2019;50:497–510.
Gan L, Ma M, Liu Y, Liu Q, Xin L, Cheng Y, et al. A clinical-radiomics model for predicting axillary pathologic complete response in breast cancer with axillary lymph node metastases. Front Oncol. 2021;11:786346.
Liu S, Du S, Gao S, Teng Y, Jin F, Zhang L. A delta-radiomic lymph node model using dynamic contrast enhanced MRI for the early prediction of axillary response after neoadjuvant chemotherapy in breast cancer patients. BMC cancer. 2023;23:15.
Gu J, Tong T, Xu D, Cheng F, Fang C, He C, et al. Deep learning radiomics of ultrasonography for comprehensively predicting tumor and axillary lymph node status after neoadjuvant chemotherapy in breast cancer patients: a multicenter study. Cancer. 2023;129:356–66.
Park H, Lim Y, Ko ES, Cho HH, Lee JE, Han BK, et al. Radiomics signature on magnetic resonance imaging: association with disease-free survival in patients with invasive breast cancer. Clin Cancer Res. 2018;24:4705–14.
Mamounas EP, Anderson SJ, Dignam JJ, Bear HD, Julian TB, Geyer CE Jr, et al. Predictors of locoregional recurrence after neoadjuvant chemotherapy: results from combined analysis of national surgical adjuvant breast and bowel project B-18 and B-27. J Clin Oncol. 2012;30:3960–6.
Funding
This study is supported by grants from the National Natural Science Foundation of China (82171898), Deng Feng Project of High-level Hospital Construction (DFJHBF202109), Guangdong Basic and Applied Basic Research Foundation (grant number 2022A1515012277, 2023A1515010222), Guangzhou Science and Technology Project (202002030236), Macao Science and Technology Development Fund (20210701181316106/AKP), Beijing Medical Award Foundation (YXJL-2020-0941-0758), Beijing Science and Technology Innovation Medical Development Foundation (KC2022-ZZ-0091-5), Development Cancer for Medical Science and Technology National Health Commission of the People’s Republic of China (WKZX2023CX110002), and Beijing Life Oasis Public Service Center (cphcf-2022-058). Funding sources were not involved in the study design, data collection, analysis and interpretation, writing of the report, or decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
Teng Zhu contributed to the conception design, collection and analysis of data, and manuscript writing. Yu-Hong Huang contributed to the data analysis, data interpretation and manuscript writing. Wei Li contributed to the collection and analysis of data, and manuscript writing. Can-Gui Wu contributed to the analysis of data, and manuscript writing. Yi-Min Zhang contributed to the conception design. Xing-Xing Zheng contributed to the analysis of pathology. Ting-Feng Zhang contributed to the provision of study materials of patients. Ying-Yi Lin and Zhi-Yong Wu contributed to the provision of study materials of patients and data proofreading. Zai-Yi Liu, Guo-Lin Ye and Ying Lin contributed to the administrative support, provision of study materials of patients and manuscript revision. Kun Wang contributed to the conception design, funding acquisition and manuscript revision. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This multicenter study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of Guangdong Provincial People’s Hospital and Institute (2019764H), and all patients in this study consented to the use of their past radiological and pathological data for research purposes.
Consent for publication
All authors have agreed on the contents of the manuscript and provided consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhu, T., Huang, YH., Li, W. et al. A non-invasive artificial intelligence model for identifying axillary pathological complete response to neoadjuvant chemotherapy in breast cancer: a secondary analysis to multicenter clinical trial. Br J Cancer 131, 692–701 (2024). https://doi.org/10.1038/s41416-024-02726-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41416-024-02726-3