Abstract
Background
Current evidence on associations between circulating bilirubin and colorectal cancer (CRC) risk is inconsistent.
Methods
In this prospective study, we investigated associations of pre-diagnostic circulating levels of total and indirect bilirubin with CRC risk in 78,467 Korean adults aged 40–78 years at recruitment, considering potential non-linearity and sex differences. Hazard ratios (HR) and 95% confidence intervals (CI) for associations with CRC risk were estimated with Cox proportional hazard regression.
Results
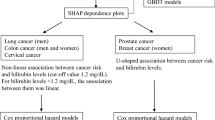
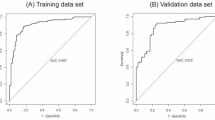
During a median 7.9-year follow-up, 539 incident CRC cases were recorded. In multivariable-adjusted models, higher levels of total bilirubin were associated with a 26% (CI: 42% to 7%) lower risk of CRC among men and women combined, comparing the highest with the lowest tertile (P-linear trend = 0.003). A U-shaped association was observed in men, with the lowest risk at approximately 0.8 mg/dL (=13.7 μmol/L) of total bilirubin (P for non-linearity = 0.01). Although the association was largely null in women, there was no evidence for effect modification by sex (P-interaction = 0.73). Associations between indirect bilirubin and CRC risk were similar.
Conclusions
Higher circulating levels of total and indirect bilirubin were inversely associated with the risk of CRC among Korean adults. The associations were strongly inverse and U-shaped among men.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets analysed during the current study are available after the approval of the review committee of the Korea National Institute of Health. The authors are not authorized to share the data other than the approved research group.
References
IARC/WHO. The Global Cancer Observatory - Cancer Fact Sheets: Colorectal Cancer. Lyon: International Agency for Research on Cancer (IARC); 2020.
Kang MJ, Jung KW, Bang SH, Choi SH, Park EH, Yun EH, et al. Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2020. Cancer Res Treat. 2023;55:385–99.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–74.
Lasry A, Zinger A, Ben-Neriah Y. Inflammatory networks underlying colorectal cancer. Nat Immunol. 2016;17:230–40.
Wagner KH, Wallner M, Mölzer C, Gazzin S, Bulmer AC, Tiribelli C, et al. Looking to the horizon: the role of bilirubin in the development and prevention of age-related chronic diseases. Clin Sci. 2015;129:1–25.
Sedlak TW, Saleh M, Higginson DS, Paul BD, Juluri KR, Snyder SH. Bilirubin and glutathione have complementary antioxidant and cytoprotective roles. Proc Natl Acad Sci USA. 2009;106:5171–6.
Rodrigues CMP, Solá S, Brito MA, Brites D, Moura JJG. Bilirubin directly disrupts membrane lipid polarity and fluidity, protein order, and redox status in rat mitochondria. J Hepatol. 2002;36:335–41.
Hansen TW, Mathiesen SB, Walaas SI. Bilirubin has widespread inhibitory effects on protein phosphorylation. Pediatr Res. 1996;39:1072–7.
Fevery J. Bilirubin in clinical practice: a review. Liver Int J Int Assoc Study Liver. 2008;28:592–605.
Buckley DB, Klaassen CD. Mechanism of gender-divergent UDP-glucuronosyltransferase mRNA expression in mouse liver and kidney. Drug Metab Dispos Biol Fate Chem. 2009;37:834–40.
Vítek L, Tiribelli C. Bilirubin: The yellow hormone? J Hepatol. 2021;75:1485–90.
Zucker SD, Horn PS, Sherman KE. Serum bilirubin levels in the U.S. population: gender effect and inverse correlation with colorectal cancer. Hepatol Balt Md. 2004;40:827–35.
Ioannou GN, Liou IW, Weiss NS. Serum bilirubin and colorectal cancer risk: a population-based cohort study. Aliment Pharm Ther. 2006;23:1637–42.
Jirásková A, Novotný J, Novotný L, Vodicka P, Pardini B, Naccarati A, et al. Association of serum bilirubin and promoter variations in HMOX1 and UGT1A1 genes with sporadic colorectal cancer. Int J Cancer. 2012;131:1549–55.
Kühn T, Sookthai D, Graf ME, Schübel R, Freisling H, Johnson T, et al. Albumin, bilirubin, uric acid and cancer risk: results from a prospective population-based study. Br J Cancer. 2017;117:1572–9.
Seyed Khoei N, Jenab M, Murphy N, Banbury BL, Carreras-Torres R, Viallon V, et al. Circulating bilirubin levels and risk of colorectal cancer: serological and Mendelian randomization analyses. BMC Med. 2020;18:229.
Seyed Khoei N, Anton G, Peters A, Freisling H, Wagner KH. The Association between Serum Bilirubin Levels and Colorectal Cancer Risk: Results from the Prospective Cooperative Health Research in the Region of Augsburg (KORA) Study in Germany. Antioxidants. 2020;9:908.
Seyed Khoei N, Wagner KH, Carreras-Torres R, Gunter MJ, Murphy N, Freisling H. Associations between Prediagnostic Circulating Bilirubin Levels and Risk of Gastrointestinal Cancers in the UK Biobank. Cancers. 2021;13:2749.
Inoguchi T, Nohara Y, Nojiri C, Nakashima N. Association of serum bilirubin levels with risk of cancer development and total death. Sci Rep. 2021;11:13224.
Kang TW, Kim HJ, Ju H, Kim JH, Jeon YJ, Lee HC, et al. Genome-wide association of serum bilirubin levels in Korean population. Hum Mol Genet. 2010;19:3672–8.
Kim YR, Choi CK, Lee YH, Choi SW, Kim HY, Shin MH, et al. Association between Albumin, Total Bilirubin, and Uric Acid Serum Levels and the Risk of Cancer: A Prospective Study in a Korean Population. Yonsei Med J. 2021;62:792–8.
Kim Y, Han BG, Group the K. Cohort Profile: The Korean Genome and Epidemiology Study (KoGES) Consortium. Int J Epidemiol. 2017;46:e20.
Health Examinees Study Group. The Health Examinees (HEXA) study: rationale, study design and baseline characteristics. Asian Pac J Cancer Prev APJCP. 2015;16:1591–7.
Ahn Y, Kwon E, Shim JE, Park MK, Joo Y, Kimm K, et al. Validation and reproducibility of food frequency questionnaire for Korean genome epidemiologic study. Eur J Clin Nutr. 2007;61:1435–41.
Kim J, Kim Y, Ahn YO, Paik HY, Ahn Y, Tokudome Y, et al. Development of a food frequency questionnaire in Koreans. Asia Pac J Clin Nutr. 2003;12:243–50.
Kityo A, Lee SA. Longitudinal changes in high sensitivity C-reactive protein associated with serum uric acid in the Korean Genome and Epidemiology Study. Sci Rep. 2024;14:374.
Zucker SD, Goessling W, Hoppin AG. Unconjugated bilirubin exhibits spontaneous diffusion through model lipid bilayers and native hepatocyte membranes. J Biol Chem. 1999;274:10852–62.
Niknam M, Maleki MH, Khakshournia S, Rasouli M, Vakili O, Shafiee SM. Bilirubin, an endogenous antioxidant that affects p53 protein and its downstream apoptosis/autophagy-related genes in LS180 and SW480 cell culture models of colorectal cancer. Biochem Biophys Res Commun. 2023;672:161–7.
Kander MC, Cui Y, Liu Z. Gender difference in oxidative stress: a new look at the mechanisms for cardiovascular diseases. J Cell Mol Med. 2017;21:1024–32.
Cheng Z, Rios GR, King CD, Coffman BL, Green MD, Mojarrabi B, et al. Glucuronidation of catechol estrogens by expressed human UDP-glucuronosyltransferases (UGTs) 1A1, 1A3, and 2B7. Toxicol Sci J Soc Toxicol. 1998;45:52–7.
Bosma PJ, Chowdhury JR, Bakker C, Gantla S, de Boer A, Oostra BA, et al. The genetic basis of the reduced expression of bilirubin UDP-glucuronosyltransferase 1 in Gilbert’s syndrome. N Engl J Med. 1995;333:1171–5.
Keshavan P, Schwemberger SJ, Smith DLH, Babcock GF, Zucker SD. Unconjugated bilirubin induces apoptosis in colon cancer cells by triggering mitochondrial depolarization. Int J Cancer. 2004;112:433–45.
Corich L, Aranda A, Carrassa L, Bellarosa C, Ostrow JD, Tiribelli C. The cytotoxic effect of unconjugated bilirubin in human neuroblastoma SH-SY5Y cells is modulated by the expression level of MRP1 but not MDR1. Biochem J. 2009;417:305–12.
Guerra Ruiz AR, Crespo J, López Martínez RM, Iruzubieta P, Casals Mercadal G, Lalana Garcés M, et al. Measurement and clinical usefulness of bilirubin in liver disease. Adv Lab Med. 2021;2:352–72.
Park B, Her EY, Lee K, Nari F, Jun JK, Choi KS, et al. Overview of the National Cancer Screening Program for Colorectal Cancer in Korea over 14 Years (2004-2017). Cancer Res Treat. 2023;55:910–7.
Vítek L, Tiribelli C. Gilbert’s syndrome revisited. J Hepatol. 2023;79:1049–55.
Acknowledgements
The authors appreciate all participants in the KoGES-HEXA Cohort Study.
Funding
This work was supported by the Austrian Science Fund (FWF, grant nr. P 32303) and the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. 2022R1A2C1004608).
Author information
Authors and Affiliations
Contributions
All authors have contributed to the publication according to the ICMJE guidelines for authorship. The specific contributions of each author are as follows. Study conceptualization and funding acquisition: K-HW, AS, and HF; Study concept and design: AS and HF; Data acquisition: JL, DK, and AS; data analysis: JL; supervision and interpretation of data analysis: HN, AS, and HF; Drafting of the manuscript: HN and HF; Reviewing of the manuscript: JL, NSK, LP-N, BF, AS, and HF; All authors approved the final version for submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This research was conducted according to the principles expressed in the Declaration of Helsinki. All study participants provided informed consent. Ethical approval was obtained from the IRBs of Seoul National University and collaborating centres of the KoGES groups, and an additional ethical approval specifically for this project was obtained from the IRB of Seoul National University College of Medicine/Hospital (Reference no.: E1810-006-974).
Consent for publication
The manuscript does not contain any individual person’s data. All reasonable measures have been taken to ensure the anonymity of study participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Noh, H., Lee, J., Seyed Khoei, N. et al. Serum bilirubin levels and risk of colorectal cancer in Korean adults: results from the Korean Genome and Epidemiology Study-Health Examinee (KoGES-HEXA) Cohort Study. Br J Cancer 131, 1635–1643 (2024). https://doi.org/10.1038/s41416-024-02847-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41416-024-02847-9