Abstract
Background
The incidence and predictors of brain metastases (BrM) from sarcoma remain poorly characterized. We aimed to determine the cumulative incidence (CuI) and risk factors for BrM.
Methods
We retrospectively analyzed data from all sarcoma patients who presented to our center (2006–2023). CuI was calculated from initial presentation to BrM, stratified by key variables. Univariable (UVA) and multivariable competing risk regression analyses (MVA) were conducted to identify risk factors.
Results
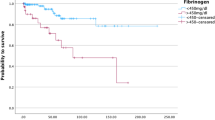
Among 5110 sarcoma patients, 117 developed BrM. CuI rates were 1.8%, 2.4%, and 2.9% at 24, 48, and 72 months, respectively, within a median onset of 17 months. On UVA, intrathoracic primary site, alveolar soft part (ASPS), epithelioid, intimal and Rhabdomyosarcoma histologies, and stage IV at diagnosis were associated with increased CuI, while age ≥59, retroperitoneal origin and liposarcoma were associated with decreased CuI. On MVA the following remained correlated to BrM incidence: intrathoracic primary (HR 5.13), ASPS (HR 4.2), age ≥59 years (HR 0.45) and liposarcoma (HR 0.11); 44.3% presented with solitary BrM. Median survival post-BrM diagnosis was 6 months.
Conclusion
BrM risk in sarcoma varies by age, histology, and tumor location. Solitary metastases were common in our BrM cohort, and OS post-BrM was poor.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The data are available from the corresponding author upon reasonable request.
Change history
02 September 2025
“The original online version of this article was revised: The article “Cumulative incidence and survival outcomes of brain metastases in sarcoma: a large single center retrospective analysis”, written by Ayah Erjan, Kurl Jamora, Enrique Gutierrez et al, was originally published open access under a “Creative Commons Attribution (CC BY) license 4.0”. As a result of the author’s/authors’ subsequent decision not to publish this article under the open access model, the copyright notice of the article was changed on 12 August 202] to © The Author(s), under exclusive licence to Springer Nature Limited, 2025 with all rights reserved.
16 October 2025
A Correction to this paper has been published: https://doi.org/10.1038/s41416-025-03176-1
References
Jędrys W, Leśniak A, Borkowska A, Rutkowski P, Sobczuk P. Brain metastases of sarcoma: a rare phenomenon in rare tumours. J Cancer Res Clin Oncol. 2023;149:18271–81. https://doi.org/10.1007/s00432-023-05451-1.
Salvati M, D’Elia A, Frati A, Santoro A. Sarcoma metastatic to the brain: a series of 35 cases and considerations from 27 years of experience. J Neurooncol. 2010;98:373–7. https://doi.org/10.1007/s11060-009-0085-0.
Gusho CA, Blank AT, Batus M. Outcomes of brain metastasis in high-grade bone and soft tissue sarcoma: an analysis of clinicopathological characteristics and survival data. Rare Tumors. 2021;13:203636132110261. https://doi.org/10.1177/20363613211026151.
Toda Y, Kobayashi E, Kubota D, Miyakita Y, Narita Y, Kawai A. A retrospective analysis of the prognosis of Japanese patients with sarcoma brain metastasis. Cancer Med. 2023;12:9471–81. https://doi.org/10.1002/cam4.5710.
Sbaraglia M, Bellan E, Dei Tos AP. The 2020 WHO classification of soft tissue tumours: news and perspectives. Pathologica. 2020;113:70–84. https://doi.org/10.32074/1591-951X-213.
Itoga R, Matsuoka M, Onodera T, Yokota I, Iwasaki K, Matsubara S, et al. Brain metastasis in soft tissue sarcoma at initial presentation. Anticancer Res. 2021;41:5611–6. https://doi.org/10.21873/anticanres.15376.
Espat NJ, Bilsky M, Lewis JJ, Leung D, Brennan MF. Soft tissue sarcoma brain metastases: prevalence in a cohort of 3829 patients. Cancer. 2002;94:2706–11. https://doi.org/10.1002/cncr.10554.
Chou Y, Liu C, Chen W, Chen T, Chen P, Wu H, et al. Brain, the last fortress of sarcoma: similar dismal outcome but discrepancy of timing of brain metastasis in bone and soft tissue sarcoma. J Surg Oncol. 2011;104:765–70. https://doi.org/10.1002/jso.22011.
Al Sannaa G, Watson KL, Olar A, Wang W, Fuller G, McCutcheon I, et al. Sarcoma brain metastases: 28 years of experience at a single institution. Ann Surg Oncol. 2016;23:962–7. https://doi.org/10.1245/s10434-016-5559-7.
Ababneh HS, Muhsen B, Fares AS, Hirbawi H, Awabdeh TA, Hussaini MA, et al. Sarcoma brain metastases: tertiary cancer center experience. J Cancer Res Ther. 2023;19:S758–63. https://doi.org/10.4103/jcrt.jcrt_654_22.
Lim JX, Karlsson B, Pang A, Vellayappan BA, Nga V. Stereotactic radiosurgery in alveolar soft part sarcoma brain metastases: case series and literature review. J Clin Neurosci. 2021;93:227–30. https://doi.org/10.1016/j.jocn.2021.09.002.
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®). Soft Tissue Sarcoma. Version 5.2024. https://www.nccn.org.
Thway K, Jones RL, Noujaim J, Fisher C. Epithelioid sarcoma: diagnostic features and genetics. Adv Anat Pathol. 2016;23:41–49. https://doi.org/10.1097/PAP.0000000000000102.
Ogose A, Morita T, Hotta T, Kobayashi H, Otsuka H, Hirata Y, et al. Brain metastases in musculoskeletal sarcomas. Jpn J Clin Oncol. 1999;29:245–7. https://doi.org/10.1093/jjco/29.5.245.
Myall NJ, Yu H, Soltys SG, Wakelee HA, Pollom E. Management of brain metastases in lung cancer: evolving roles for radiation and systemic treatment in the era of targeted and immune therapies. Neuro Oncol Adv. 2021;3:v52–v62. https://doi.org/10.1093/noajnl/vdab106.
Raghavendra AS, Ibrahim NK. Breast cancer brain metastasis: a comprehensive review. JCO Oncol Pr. 2024;20:1348–59. https://doi.org/10.1200/OP.23.00794.
Nguyen A, Nguyen A, Fleeting C, Patel A, Bazett N, Hey G, et al. An evaluation of risk factors for intracranial metastases of sarcomas: a systematic review and meta-analysis. World Neurosurg. 2024;187(Jul):e683–99. https://doi.org/10.1016/j.wneu.2024.04.146.
Author information
Authors and Affiliations
Contributions
Study design: AE, DBS, Data Collection: AE, KJ, AVN, EG, Data Analysis: AS; Data Interpretation: AE, KJ, EG, AS, AVN, B-AM, NL, TC, DK, PW, PC, CC, DK, DBS; Writing first draft: AE; Reviewing, editing and approving final manuscript: AE, KJ, EG, AS, AVN, B-AM, NL, TC, DK, PW, PC, CC, DK, DBS; Supervision: DBS.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This retrospective study utilized previously collected data. Ethical approval was obtained from the University Health Network Research Ethics Board (UHN REB number 23-5735). All methods were performed in accordance with relevant guidelines and regulations. All data were anonymized to ensure participant confidentiality. Informed consent was waived as the study used de-identified data.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
“The original online version of this article was revised: The article “Cumulative incidence and survival outcomes of brain metastases in sarcoma: a large single center retrospective analysis”, written by Ayah Erjan, Kurl Jamora, Enrique Gutierrez et al, was originally published open access under a “Creative Commons Attribution (CC BY) license 4.0”. As a result of the author’s/authors’ subsequent decision not to publish this article under the open access model, the copyright notice of the article was changed on 12 August 202] to © The Author(s), under exclusive licence to Springer Nature Limited, 2025 with all rights reserved.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Erjan, A., Jamora, K., Gutierrez, E. et al. Cumulative incidence and survival outcomes of brain metastases in sarcoma: a large single center retrospective analysis. Br J Cancer 133, 1508–1517 (2025). https://doi.org/10.1038/s41416-025-03111-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41416-025-03111-4