Abstract
Background
The amount and activity of breast stem cell population may play an important role in breast carcinogenesis. However, little is known about whether early-life and adult anthropometric measures, including body mass index (BMI), birthweight, and height, are associated with stem cell marker expressions in non-cancerous breast tissue.
Methods
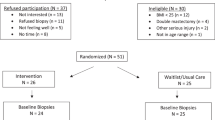
Among 730 women with biopsy-confirmed benign breast disease (BBD) in the Nurses’ Health Study II, we quantified immunohistochemical staining of stem cell markers (CD44, CD24, ALDH1A1) in histopathologically normal epithelial and stromal breast tissue. Linear regression was conducted to estimate the associations of anthropometric measures with stem cell marker expression, adjusting for potential confounders.
Results
BMI at age 18 (≥23.0 vs. <19.0 kg/m2), BMI at benign breast biopsy (≥30.0 vs. <21.0 kg/m2), and change in BMI since age 18 (>7.0 vs. ≤0 kg/m2) were inversely associated with CD44 expression levels in epithelium and stroma combined (β [95% CI]= -0.30 [-0.55, -0.04]; -0.34 [−0.59, −0.08]; −0.38 [−0.65, −0.10]; respectively). Change in BMI since age 18 (>7.0 vs. ≤0 kg/m2) was also inversely associated with ALDH1A1 expression in epithelium (−0.31 [−0.62, −0.001]) and stroma (−0.63 [−1.18, −0.08]). Birthweight and height were not associated.
Conclusion
Adiposity measures may be associated with stem cell marker expression among cancer-free women.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets generated and/or analysed during the current study are available in the Nurses’ Health Study repository after reasonable request.
References
Wicha MS, Liu S, Dontu G. Cancer stem cells: an old idea-a paradigm shift. Cancer Res. 2006;66:1883–90. https://doi.org/10.1158/0008-5472.CAN-05-3153
Ginestier C, Wicha MS. Mammary stem cell number as a determinate of breast cancer risk. Breast Cancer Res. 2007;9:109. https://doi.org/10.1186/bcr1741
Cobaleda C, Cruz JJ, Gonzalez-Sarmiento R, Sanchez-Garcia I, Perez-Losada J. The emerging picture of human breast cancer as a stem cell-based disease. Stem Cell Rev. 2008;4:67–79. https://doi.org/10.1007/s12015-008-9012-6
Smalley M, Ashworth A. Stem cells and breast cancer: a field in transit. Nat Rev Cancer. 2003;3:832–44. https://doi.org/10.1038/nrc1212
Yaghjyan L, Heng YJ, Baker GM, Murthy D, Mahoney MB, Rosner B, et al. Associations of stem cell markers CD44, CD24 and ALDH1A1 with mammographic breast density in women with benign breast biopsies. Br J Cancer. 2024;131:325–33. https://doi.org/10.1038/s41416-024-02743-2
Yaghjyan L, Stoll E, Ghosh K, Scott CG, Jensen MR, Brandt KR, et al. Tissue-based associations of mammographic breast density with breast stem cell markers. Breast Cancer Res. 2017;19:100. https://doi.org/10.1186/s13058-017-0889-3
Green J, Cairns BJ, Casabonne D, Wright FL, Reeves G, Beral V, et al. Height and cancer incidence in the Million Women Study: prospective cohort, and meta-analysis of prospective studies of height and total cancer risk. Lancet Oncol. 2011;12:785–94. https://doi.org/10.1016/S1470-2045(11)70154-1
Michels KB, Xue F, Terry KL, Willett WC. Longitudinal study of birthweight and the incidence of breast cancer in adulthood. Carcinogenesis. 2006;27:2464–8. https://doi.org/10.1093/carcin/bgl105
Zhou W, Chen X, Huang H, Liu S, Xie A, Lan L. Birth weight and incidence of breast cancer: dose-response meta-analysis of prospective studies. Clin Breast Cancer. 2020;20:e555–68. https://doi.org/10.1016/j.clbc.2020.04.011
Byun D, Hong S, Ryu S, Nam Y, Jang H, Cho Y, et al. Early-life body mass index and risks of breast, endometrial, and ovarian cancers: a dose-response meta-analysis of prospective studies. Br J Cancer. 2022;126:664–72. https://doi.org/10.1038/s41416-021-01625-1
Oh H, Boeke CE, Tamimi RM, Smith-Warner SA, Wang M, Willett WC, et al. The interaction between early-life body size and physical activity on risk of breast cancer. Int J Cancer. 2015;137:571–81. https://doi.org/10.1002/ijc.29272
Premenopausal Breast Cancer Collaborative Group, Schoemaker MJ, Nichols HB, Wright LB, Brook MN, Jones ME, et al. Association of body mass index and age with subsequent breast cancer risk in premenopausal women. JAMA Oncol. 2018;4:e181771. https://doi.org/10.1001/jamaoncol.2018.1771
Munsell MF, Sprague BL, Berry DA, Chisholm G, Trentham-Dietz A. Body mass index and breast cancer risk according to postmenopausal estrogen-progestin use and hormone receptor status. Epidemiol Rev. 2014;36:114–36. https://doi.org/10.1093/epirev/mxt010
Oh H, Wild RA, Manson JE, Bea JW, Shadyab AH, Pfeiffer RM, et al. Obesity, height, and serum androgen metabolism among postmenopausal women in the Women’s Health Initiative Observational Study. Cancer Epidemiol Biomarkers Prev. 2021;30:2018–29. https://doi.org/10.1158/1055-9965.EPI-21-0604
Oh H, Coburn SB, Matthews CE, Falk RT, LeBlanc ES, Wactawski-Wende J, et al. Anthropometric measures and serum estrogen metabolism in postmenopausal women: the Women’s Health Initiative Observational Study. Breast Cancer Res. 2017;19:28. https://doi.org/10.1186/s13058-017-0810-0
Poole EM, Tworoger SS, Hankinson SE, Schernhammer ES, Pollak MN, Baer HJ. Body size in early life and adult levels of insulin-like growth factor 1 and insulin-like growth factor binding protein 3. Am J Epidemiol. 2011;174:642–51. https://doi.org/10.1093/aje/kwr123
Tamimi RM, Eriksson L, Lagiou P, Czene K, Ekbom A, Hsieh CC, et al. Birth weight and mammographic density among postmenopausal women in Sweden. Int J Cancer. 2010;126:985–91. https://doi.org/10.1002/ijc.24786
Oh H, Rice MS, Warner ET, Bertrand KA, Fowler EE, Eliassen AH, et al. Early-life and adult anthropometrics in relation to mammographic image intensity variation in the Nurses’ Health Studies. Cancer Epidemiol Biomarkers Prev. 2020;29:343–51. https://doi.org/10.1158/1055-9965.EPI-19-0832
Masala G, Bendinelli B, Caini S, Duroni G, Ermini I, Pastore E, et al. Lifetime changes in body fatness and breast density in postmenopausal women: the FEDRA study. Breast Cancer Res. 2023;25:35. https://doi.org/10.1186/s13058-023-01624-5
Oh H, Yaghjyan L, Austin-Datta RJ, Heng YJ, Baker GM, Sirinukunwattana K, et al. Early-life and adult adiposity, adult height, and benign breast tissue composition. Cancer Epidemiol Biomarkers Prev. 2021;30:608–15. https://doi.org/10.1158/1055-9965.EPI-20-1348
Oh H, Eliassen AH, Beck AH, Rosner B, Schnitt SJ, Collins LC, et al. Breast cancer risk factors in relation to estrogen receptor, progesterone receptor, insulin-like growth factor-1 receptor, and Ki67 expression in normal breast tissue. npj Breast Cancer. 2017;3:39. https://doi.org/10.1038/s41523-017-0041-7
Oh H, Yaghjyan L, Heng YJ, Rosner B, Mahoney MB, Murthy D, et al. Associations of early-life and adult anthropometric measures with the expression of stem cell markers CD44, CD24, and ALDH1A1 in women with benign breast biopsies. Cancer Epidemiol Biomarkers Prev. 2024;33:933–43. https://doi.org/10.1158/1055-9965.EPI-23-1567
Yaghjyan L, Heng YJ, Baker GM, Bret-Mounet V, Murthy D, Mahoney MB, et al. Reliability of CD44, CD24, and ALDH1A1 immunohistochemical staining: pathologist assessment compared to quantitative image analysis. Front Med. 2022;9:1040061. https://doi.org/10.3389/fmed.2022.1040061
Li W, Ma H, Zhang J, Zhu L, Wang C, Yang Y. Unraveling the roles of CD44/CD24 and ALDH1 as cancer stem cell markers in tumorigenesis and metastasis. Sci Rep. 2017;7:13856. https://doi.org/10.1038/s41598-017-14364-2
Beca FF, Caetano P, Gerhard R, Alvarenga CA, Gomes M, Paredes J, et al. Cancer stem cells markers CD44, CD24 and ALDH1 in breast cancer special histological types. J Clin Pathol. 2013;66:187–91. https://doi.org/10.1136/jclinpath-2012-201169
Zhao K, Wu C, Li X, Niu M, Wu D, Cui X, et al. From mechanism to therapy: the journey of CD24 in cancer. Front Immunol. 2024;15:1401528. https://doi.org/10.3389/fimmu.2024.1401528
Ponta H, Sherman L, Herrlich PA. CD44: from adhesion molecules to signalling regulators. Nat Rev Mol Cell Biol. 2003;4:33–45. https://doi.org/10.1038/nrm1004
Yue H, Hu Z, Hu R, Guo Z, Zheng Y, Wang Y, et al. ALDH1A1 in cancers: bidirectional function, drug resistance, and regulatory mechanism. Front Oncol. 2022;12:918778. https://doi.org/10.3389/fonc.2022.918778
Liu G, Liu GX, Fang Y, Cao ZY, Du HH, Fu J, et al. Clinicopathological and prognostic value of CD24 expression in breast cancer: a meta-analysis. Int J Biol Markers. 2017;32:e182–9. https://doi.org/10.5301/jbm.5000254
McFarlane S, Coulter JA, Tibbits P, O’Grady A, McFarlane C, Montgomery N, et al. CD44 increases the efficiency of distant metastasis of breast cancer. Oncotarget. 2015;6:11465–76. https://doi.org/10.18632/oncotarget.3410
Lee JH, Kim SH, Lee ES, Kim YS. CD24 overexpression in cancer development and progression: a meta-analysis. Oncol Rep. 2009;22:1149–56. https://doi.org/10.3892/or_00000548
Khoury T, Ademuyiwa FO, Chandrasekhar R, Jabbour M, Deleo A, Ferrone S, et al. Aldehyde dehydrogenase 1A1 expression in breast cancer is associated with stage, triple negativity, and outcome to neoadjuvant chemotherapy. Mod Pathol. 2012;25:388–97. https://doi.org/10.1038/modpathol.2011.172
Liu Y, Lv DL, Duan JJ, Xu SL, Zhang JF, Yang XJ, et al. ALDH1A1 expression correlates with clinicopathologic features and poor prognosis of breast cancer patients: a systematic review and meta-analysis. BMC Cancer. 2014;14:444. https://doi.org/10.1186/1471-2407-14-444
Jacobs TW, Byrne C, Colditz G, Connolly JL, Schnitt SJ. Pathologic features of breast cancers in women with previous benign breast disease. Am J Clin Pathol. 2001;115:362–9. https://doi.org/10.1309/up07-k3kd-25nl-d3m8
Tamimi RM, Byrne C, Baer HJ, Rosner B, Schnitt SJ, Connolly JL, et al. Benign breast disease, recent alcohol consumption, and risk of breast cancer: a nested case–control study. Breast Cancer Research. 2005;7:R555. https://doi.org/10.1186/bcr1039
Tamimi RM, Colditz GA, Wang Y, Collins LC, Hu R, Rosner B, et al. Expression of IGF1R in normal breast tissue and subsequent risk of breast cancer. Breast Cancer Res Treat. 2011;128:243–50. https://doi.org/10.1007/s10549-010-1313-1
Page DL, Dupont WD, Rogers LW, Rados MS. Atypical hyperplastic lesions of the female breast. a long-term follow-up study. Cancer. 1985;55:2698–708. 10.1002/1097-0142(19850601)55:11<2698::aid-cncr2820551127>3.0.co;2-a
Stunkard AJ, Sorensen T, Schulsinger F. Use of the Danish Adoption Register for the study of obesity and thinness. Res Publ Assoc Res Nerv Ment Dis. 1983;60:115–20.
Must A, Willett WC, Dietz WH. Remote recall of childhood height, weight, and body build by elderly subjects. Am J Epidemiol. 1993;138:56–64. https://doi.org/10.1093/oxfordjournals.aje.a116777
Troy LM, Michels KB, Hunter DJ, Spiegelman D, Manson JE, Colditz GA, et al. Self-reported birthweight and history of having been breastfed among younger women: an assessment of validity. Int J Epidemiol. 1996;25:122–7. https://doi.org/10.1093/ije/25.1.122
Baker GM, Bret-Mounet VC, Wang T, Veta M, Zheng H, Collins LC, et al. Immunohistochemistry scoring of breast tumor tissue microarrays: a comparison study across three software applications. J Pathol Inform. 2022;13:100118. https://doi.org/10.1016/j.jpi.2022.100118
Collins LC, Wang Y, Connolly JL, Baer HJ, Hu R, Schnitt SJ, et al. Potential role of tissue microarrays for the study of biomarker expression in benign breast disease and normal breast tissue. Appl Immunohistochem Mol Morphol. 2009;17:438–41. https://doi.org/10.1097/PAI.0b013e3181993d86
Bankhead P, Loughrey MB, Fernández JA, Dombrowski Y, McArt DG, Dunne PD, et al. QuPath: open source software for digital pathology image analysis. Sci Rep. 2017;7:16878. https://doi.org/10.1038/s41598-017-17204-5
Dorgan JF, Klifa C, Shepherd JA, Egleston BL, Kwiterovich PO, Himes JH, et al. Height, adiposity and body fat distribution and breast density in young women. Breast Cancer Res. 2012;14:R107. https://doi.org/10.1186/bcr3228
Potischman N, Swanson CA, Siiteri P, Hoover RN. Reversal of relation between body mass and endogenous estrogen concentrations with menopausal status. J Natl Cancer Inst. 1996;88:756–8. https://doi.org/10.1093/jnci/88.11.756
Tworoger SS, Eliassen AH, Missmer SA, Baer H, Rich-Edwards J, Michels KB, et al. Birthweight and body size throughout life in relation to sex hormones and prolactin concentrations in premenopausal women. Cancer Epidemiol Biomarkers Prev. 2006;15:2494–501. https://doi.org/10.1158/1055-9965.EPI-06-0671
Siiteri PK. Adipose tissue as a source of hormones. Am J Clin Nutr. 1987;45:277–82. https://doi.org/10.1093/ajcn/45.1.277
Giatromanolaki A, Sivridis E, Fiska A, Koukourakis MI. The CD44+/CD24- phenotype relates to ‘triple-negative’ state and unfavorable prognosis in breast cancer patients. Med Oncol. 2011;28:745–52. https://doi.org/10.1007/s12032-010-9530-3
Acknowledgements
The authors would like to acknowledge the contribution to this study from central cancer registries supported through the Centers for Disease Control and Prevention’s National Program of Cancer Registries (NPCR) and/or the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program. Central registries may also be supported by state agencies, universities, and cancer centres. Participating central cancer registries include the following: Alabama, Alaska, Arizona, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Hawaii, Idaho, Indiana, Iowa, Kentucky, Louisiana, Massachusetts, Maine, Maryland, Michigan, Mississippi, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Puerto Rico, Rhode Island, Seattle SEER Registry, South Carolina, Tennessee, Texas, Utah, Virginia, West Virginia, Wyoming.
Funding
This work was supported by the National Cancer Institute at the National Institutes of Health [CA240341 to LY, CA131332, CA175080 to RMT, P01 CA87969, UM1 CA186107, U01 CA176726], Avon Foundation for Women, Susan G. Komen for the Cure®, and Breast Cancer Research Foundation. HO was supported by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (NRF) grant (NRF-2023S1A5C2A03095169).
Author information
Authors and Affiliations
Contributions
HO performed statistical analyses, drafted the manuscript, and interpreted results. LY conceived of and designed the study, made substantial contributions to interpretation of data and critical revision of the manuscript, provided final review and approval, and supervised the overall study progress. YJH assessed laboratory (immunohistochemistry) results and made substantial contributions to interpretation of data and critical revision of the manuscript. GMB made substantial contributions to interpretation of data and critical revision of the manuscript. BRS made substantial contributions to interpretation of data and critical revision of the manuscript. MBM made substantial contributions to interpretation of data and critical revision of the manuscript. DM made substantial contributions to curation of data and critical revision of the manuscript. BR made substantial contributions to interpretation of data and critical revision of the manuscript. RMT conceived of and designed the study, made substantial contributions to interpretation of data and critical revision of the manuscript, and provided final review and approval. LY and RMT shared senior authorship on this manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
Consent for publication was obtained from the study participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Oh, H., Yaghjyan, L., Heng, Y.J. et al. Birthweight, height, and body mass index in relation to the expression of stem cell markers among women with benign breast biopsies in the Nurses’ Health Study II. Br J Cancer 133, 1695–1707 (2025). https://doi.org/10.1038/s41416-025-03194-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41416-025-03194-z