Abstract
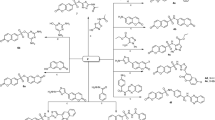
Twenty triphenylphosphonium (TPP) conjugates in which 1-alkynyl-substituted nucleic bases (uracil, thymine) and their analogues (6-methyluracil, quinazoline-2,4-dione) were connected to the TPP cation via an octyl or decyl linker were synthesized. In vitro evaluation of their antibacterial activity against five Gram-positive bacteria, two Gram-negative bacteria and fungus C. albicans revealed six lead compounds which exhibited high bacteriostatic activity (MIC 0.2–0.9 μM) against Gram-positive bacteria S. aureus, B. cereus, E. faecalis, as well as MRSA strains. These lead compounds are TPP-conjugates in which 1-alkynylquinazoline-2,4-dione moiety is bound to the TPP cation via the decyl (4 d, 4 f) or octyl (4e) linker and biscationic TPP-conjugates in which two TPP cations are attached to the N-1 and N-3 atoms of 5-alkynylquinazoline-2,4-dione moiety via the decyl (5 d, 5 f) or octyl (5e) linkers. Biscations 5 d and 5e showed high in vitro bacteriostatic and bactericidal activity (MIC/MBC 0.2–7.8 μM) against Gram-negative bacteria E. coli and P. aeruginosa. In addition, biscations 5 d and 5 f exhibited noticeable in vitro fungistatic and fungicidal activity against fungus C. albicans. Using colorimetric and fluorimetric methods, it was found that all lead compounds at concentrations corresponding to the MIC and MBC values caused cytoplasmic membrane damage and depolarization, without violating the integrity of the S. aureus cell wall. In addition, all lead compounds inhibited the formation of S. aureus biofilm by 80-100% at concentrations close to the MBC value (about 0.8 μM), and destroyed already formed S. aureus biofilm at concentrations in the range of 6.3–12.5 μM.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
D’Souza GGM, Wagle MA, Saxena V, Shah A. Approaches for targeting mitochondria in cancer therapy. Biochim Biophys Acta. 2011;1807:689–96. https://doi.org/10.1016/j.bbabio.2010.08.008.
Battogtokh G, Cho Y-Y, Lee JY, Lee HS, Kang HC. Mitochondrial-targeting anticancer agent conjugates and nanocarrier systems for cancer treatment. Front Pharm. 2018;9:922. https://doi.org/10.3389/fphar.2018.00922.
Bock FJ, Tait SWG. Mitochondria as multifaceted regulators of cell death. Nat Rev Mol Cell Biol. 2020;21:85–100. https://doi.org/10.1038/s41580-019-0173-8.
Lee H-C, Wei Y-H. Mitochondrial role in life and death of the cell. J Biomed Sci. 2000;7:2–15. https://doi.org/10.1007/BF02255913.
Guo X, Yang N, Ji W, Zhang H, Dong X, Zhou Z, Li L, Shen H-M, Yao SQ, Huang W. Mito-Bomb: Targeting mitochondria for cancer therapy. Adv Mater. 2021:e2007778. https://doi.org/10.1002/adma.202007778.
Ross MF, Kelso GF, Blaikie FH, James AM, Cochemé HM, Filipovska A, Da Ros T, Hurd TR, Smith RAJ, Murphy MP. Lipophilic triphenylphosphonium cations as tools in mitochondrial bioenergetics and free radical biology. Biochem (Mosc. 2005;70:222–30. https://doi.org/10.1007/s10541-005-0104-5.
Wang J, Li J, Xiao Y, Fu B, Qin Z. TPP-based mitocans: a potent strategy for anticancer drug design. RSC Med Chem. 2020;11:858–75. https://doi.org/10.1039/c9md00572b.
Jung K, Reszka R. Mitochondria as subcellular targets for clinically useful anthracyclines. Adv Drug Deliv Rev. 2001;49:87–105. https://doi.org/10.1016/S0169-409X(01)00128-4.
Esfandyari-Manesha M, Mohammadi A, Atyabi F, Ebrahimi SM, Shahmoradi E, Amini M, Mirzaie ZH, Ghahremani MH, Dinarvand R. Enhancement mitochondrial apoptosis in breast cancer cells by paclitaxeltriphenylphosphonium conjugate in DNA aptamer modified nanoparticles. J Drug Deliv Sci Technol. 2019;54:101228. https://doi.org/10.1016/j.jddst.2019.101228.
Zielonka J, Joseph J, Sikora A, Hardy M, Ouari O, Vasquez-Vivar J, Cheng G, Lopez M, Kalyanaraman B. Mitochondria-targeted triphenylphosphonium-based compounds: Syntheses, mechanisms of action, and therapeutic and diagnostic applications. Chem Rev. 2017;117:10043–120. https://doi.org/10.1021/acs.chemrev.7b00042.
Jeena MT, Kim S, Jin S, Ryu J-H. Recent progress in mitochondria-targeted drug and drug-free agents for cancer therapy. Cancers. 2020;12:4 https://doi.org/10.3390/cancers12010004.
Li Y, Zeng Q, Wang R, Wang B, Chen R, Wang N, Lu Y, Shi F, Dehaen W, Huai Q. Synthesis and discovery of mitochondria-targeting oleanolic acid derivatives for potential PI3K inhibition. Fitoterapia. 2022;162:105291. https://doi.org/10.1016/j.fitote.2022.105291.
Gray MW. Mitochondrial evolution. Cold Spring Harb Perspect Biol. 2012;4:a011403 https://doi.org/10.1101/cshperspect.a011403.
Boguszewska K, Szewczuk M, Kazmierczak-Baranska J, Karwowski BT. The similarities between human mitochondria and bacteria in the context of structure, genome, and base excision repair system. Molecules. 2020;25:2857. https://doi.org/10.3390/molecules25122857.
Epand RM, Walker C, Epand RF, Magarvey NA. Molecular mechanisms of membrane targeting antibiotics. Biochim Biophys Acta. 2016;1858:980–87. https://doi.org/10.1016/j.bbamem.2015.10.018.
Alborn WEJR, Allen NE, Preston DA. Daptomycin disrupts membrane potential in growing Staphylococcus aureus. Antimicrob Agents Chemother. 1991;35:2282–87. https://doi.org/10.1128/AAC.35.11.2282.
Ibrahim MK, Haria A, Mehta NV, Degani MS. Antimicrobial potential of quaternary phosphonium salt compounds: a review. Future Med Chem. 2023;15:2113–41. https://doi.org/10.4155/fmc-2023-0188.
Furst VH, Wetzke G, Berger W, Schubert W. Quarternare Triphenylphosphoniumverbindungen. J Prakt Chem. 1962;17:299–313. https://doi.org/10.1002/prac.19620170507.
Tumanov AA, Shevchuk MI, Postnov IE, Glukhova MN, Osipova NI, Tolochko AF, Subbotina GM. Antimicrobial activity of phosphonium salts and ylides and their chemical constitution. Pharm Chem J. 1978;12:1583–85. https://doi.org/10.1007/BF00770780.
Nunes B, Cagide F, Fernandes C, Borges A, Borges F, Simes M. Efficacy of novel quaternary ammonium and phosphonium salts differing in cation type and alkyl chain length against antibiotic-resistant Staphylococcus aureus. Int J Mol Sci. 2024;25:504. https://doi.org/10.3390/ijms25010504.
Khailova LS, Nazarov PA, Sumbatyan NV, Korshunova GA, Rokitskaya TI, Dedukhova VI, Antonenko YuN, Skulachev VP. Uncoupling and toxic action of alkyltriphenylphosphonium cations on mitochondria and the bacterium Bacillus subtilis as a function of alkyl chain length. Biochem (Mosc. 2015;80:1589–97. https://doi.org/10.1134/S000629791512007X.
Kanazawa A, Ikeda T, Endo T. Synthesis and antimicrobial activity of dimethyl- and trimethyl-substituted phosphonium salts with alkyl chains of various lengths. Antimicrob Agents Chemother. 1994;38:945–52. https://doi.org/10.1128/aac.38.5.945.
Terekhova NV, Khailova LS, Rokitskaya TI, Nazarov PA, Islamov DR, Usachev KS, Tatarinov DA, Mironov VF, Kotova EA, Antonenko. YuN. Trialkyl(vinyl)phosphonium chlorophenol derivatives as potent mitochondrial uncouplers and antibacterial agents. ACS Omega. 2021;6:20676–85. https://doi.org/10.1021/acsomega.1c02909.
O’Toole GA, Wathier M, Zegans ME, Shanks RMQ, Kowalski R, Grinstaff MW. Diphosphonium ionic liquids as broad spectrum antimicrobial agents. Cornea. 2012;31:810–16. https://doi.org/10.1097/ICO.0b013e31823f0a86.
Brunel F, Lautard C, Garzino F, Raimundo J-M, Bolla J-M, Camplo M. Phosphonium-ammonium-based di-cationic ionic liquids as antibacterial over the ESKAPE group. Bioorg Med Chem Lett. 2020;30:127389. https://doi.org/10.1016/j.bmcl.2020.127389.
Spahr AC, Michaud ME, Amoo LE, Sanchez CA, Hogue CE, Thierer LM, Gau MR, Wuest WM, Minbiole KPC. Rigidity-activity relationships of bisQPC scaffolds against pathogenic bacteria. ChemMedChem. 2022;17:e202200224. https://doi.org/10.1002/cmdc.202200224.
Sommers KJ, Michaud ME, Hogue CE, Scharnow AM, Amoo LE, Petersen AA, Carden RG, Minbiole KPC, Wuest WM. Quaternary phosphonium compounds: An examination of non-nitrogenous cationic amphiphiles that evade disinfectant resistance. ACS Infect Dis. 2022;8:387–97. https://doi.org/10.1021/acsinfecdis.1c00611.
Shi LW, Zhuang Q-Q, Wang T-Q, Jiang X-D, Liu Y, Deng J-W, Sun H-H, Li Y, Li H-H, Liu T-B, Liu J-Z. Synthetic antibacterial quaternary phosphorus salts promote methicillin-resistant Staphylococcus aureus-infected wound healing. Int J Nanomed. 2023;18:1145–58. https://doi.org/10.2147/IJN.S398748.
Chen CW, Pavlova JA, Lukianov DA, Tereshchenkov AG, Makarov GI, Khairullina ZZ, Tashlitsky VN, Paleskava A, Konevega AL, Bogdanov AA, Osterman IA, Sumbatyan NV, Polikanov. YuS. Binding and action of triphenylphosphonium analog of chloramphenicol upon the bacterial ribosome. Antibiotics. 2021;10:390. https://doi.org/10.3390/antibiotics10040390.
Pavlova JA, Khairullina ZZ, Tereshchenkov AG, Nazarov PA, Lukianov DA, Volynkina IA, Skvortsov DA, Makarov GI, Abad E, Murayama SY, Kajiwara S, Paleskava A, Konevega AL, Antonenko YuN, Lyakhovich A, Osterman IA, Bogdanov AA, Sumbatyan NV. Triphenilphosphonium analogs of chloramphenicol as dual-acting antimicrobial and antiproliferating agents. Antibiotics. 2021;10:489. https://doi.org/10.3390/antibiotics10050489.
Nam YS, Cho SY, Yang HY, Park KS, Jang J-H, Kim Y-T, Jeong J-w, Suh J-T, Lee H-J. Investigation of mutation distribution in DNA gyrase and topoisomerase IV genes in ciprofloxacin-non-susceptible Enterobacteriaceae isolated from blood cultures in a tertiary care university hospital in South Korea, 2005–2010. Int J Antimicrob Agents. 2013;41:126–29. https://doi.org/10.1016/j.ijantimicag.2012.10.004.
Kang S, Sunwoo K, Jung Y, Hur JK, Park K-H, Kim JS, Kim D. Membrane-targeting triphenylphosphonium functionalized Ciprofloxacin for methicillin-resistant Staphylococcus aureus (MRSA). Antibiotics. 2020;9:758. https://doi.org/10.3390/antibiotics9110758.
Tsepaeva OV, Nemtarev AV, Salikhova TI, Abdullin TI, Khozyainova GrigorevaLR, Mironov SA. VF. Synthesis, anticancer, and antibacterial activity of betulinic and betulonic acid C-28-triphenylphosphonium conjugates with variable alkyl linker length. Anticancer Agents Med Chem. 2020;20:286–300. https://doi.org/10.2174/1871520619666191014153554.
Gupta SC, Patchva S, Aggarwal BB. Therapeutic roles of Curcumin: Lessons learned from clinical trials. AAPS J. 2013;15:195–218. https://doi.org/10.1208/s12248-012-9432-8.
Kumari S, Jayakumar S, Gupta GD, Bihani SC, Sharma D, Kutala VK, Sandur SK, Kumara V. Antibacterial activity of new structural class of semisynthetic molecule, triphenyl-phosphonium conjugated diarylheptanoid. Free Radic Biol Med. 2019;143:140–5. https://doi.org/10.1016/j.freeradbiomed.2019.08.003.
Kumari S, Jayakumar S, Bihani SC, Shetake N, Naidu R, Kutala VK, Sarma HD, Gupta GD, Sandur SK, Kumar V. Pharmacological characterization of a structurally new class of antibacterial compound, triphenyl-phosphonium conjugated diarylheptanoid: Antibacterial activity and molecular mechanism. J Biosci. 2020;45:147. https://doi.org/10.1007/s12038-020-00113-7.
Fialová SB, Kello M, Coma M, Slobodníková L, Drobná E, Holková I, Garajová M, Mrva M, Zachar V, Lukác M. Derivatization of rosmarinic acid enhances its in vitro antitumor, antimicrobial and antiprotozoal properties. Molecules. 2019;24:1078. https://doi.org/10.3390/molecules24061078.
Rokitskaya TI, Terekhova NV, Khailova LS, Kotova EA, Plotnikov EY, Zorov DB, Tatarinov DA, Antonenko YU. Zwitterionic protonophore derived from 2-(2-hydroxyaryl)alkenylphosphonium as an uncoupler of oxidative phosphorylation. Bioconjugate Chem. 2019;30:2435–43. https://doi.org/10.1021/acs.bioconjchem.9b00516.
Terekhova NV, Tatarinov DA, Shaihutdinova ZM, Pashirova TN, Lyubina AP, Voloshina AD, Sapunova AS, Zakharova LYA, Mironov VF. Design and synthesis of amphiphilic 2-hydroxybenzylphosphonium salts with antimicrobial and antitumor dual action. Bioorg Med Chem Lett. 2020;30:127234. https://doi.org/10.1016/j.bmcl.2020.127234.
Galkina I, Bakhtiyarova YU, Andriyashin V, Galkin V, Cherkasov R. Synthesis and antimicrobial activities of phosphonium salts on basis of triphenylphosphine and 3,5-di-tert-butyl-4-hydroxybenzyl bromide. Phosph Sulfur Silicon Relat Elem. 2013;188:15–18. https://doi.org/10.1080/10426507.2012.740694.
Galkina IV, Andriyashin VV, Romanov SR, Davletshin RR, Pozdeev OK, Shulaeva MP, Litvinov IA, Bakhtiyarova YuV. Synthesis and structure of quaternary phosphonium salts based on phosphorylated sterically hindered phenols. Russ J Gen Chem. 2022;92:1199–207. https://doi.org/10.1134/S1070363222070040.
Cuthbert TJ, Hisey B, Harrison TD, Trant JF, Gillies ER, Ragogna PJ. Surprising antibacterial activity and selectivity of hydrophilic polyphosphoniums featuring sugar and hydroxy substituents. Angew Chem Int Ed. 2018;57:12707–10. https://doi.org/10.1002/anie.201806412.
Cao P, Bai X, He Y, Song P, Wang R, Huang J. Nano-assemblies of phosphonium-functionalized diblock copolymers with fabulous antibacterial properties and relationships of structure-activity. J Mater Chem B. 2022;10:9202. https://doi.org/10.1039/d2tb01778d.
Crismaru M, Asri LATW, Loontjens TJA, Krom BP, de Vries J, van der Mei HC, Busscher HJ. Survival of adhering Staphylococci during exposure to a quaternary ammonium compound evaluated by using atomic force microscopy imaging. Antimicrob Agents Chemother. 2011;55:5010–17. https://doi.org/10.1128/aac.05062-11.
Alfei S. Shifting from Ammonium to Phosphonium Salts: A Promising Strategy to Develop Next-GenerationWeapons against Biofilms. Pharmaceutics. 2024;16:80. https://doi.org/10.3390/pharmaceutics16010080.
Nikitina EV, Zeldi MI, Pugachev MV, Sapozhnikov SV, Shtyrlin NV, Kuznetsova SV, Evtygin VE, Bogachev MI, Kayumov AR, Shtyrlin. YuG. Antibacterial effects of quaternary bis-phosphonium and ammonium salts of pyridoxine on Staphylococcus aureus cells: A single base hitting two distinct targets?. World J Microbiol Biotechnol. 2016;32:5. https://doi.org/10.1007/s11274-015-1969-0.
Wang J, Liu X, Yin F, Xu Y, Fu B, Li J, Qin Z. Triphenylphosphonium (TPP)-conjugated quinolone analogs displayed significantly enhanced fungicidal activity superior to its parent molecule. J Fungi. 2023;9:685. https://doi.org/10.3390/jof9060685.
Strobykina IYU, Voloshina AD, Andreeva OV, Sapunova AS, Lyubina AP, Amerhanova SK, Belenok MG, Saifina LF, Semenov VE, Kataev VE. Synthesis, antimicrobial activity and cytotoxicity of triphenylphosphonium (TPP) conjugates of 1,2,3-triazolyl nucleoside analogues. Bioorg Chem. 2021;116:105328. https://doi.org/10.1016/j.bioorg.2021.105328.
Grymel M, Lalik A, Kazek-Kesik A, Szewczyk M, Grabiec P, Erfurt K. Design, synthesis and preliminary evaluation of the cytotoxicity and antibacterial activity of novel triphenylphosphonium derivatives of betulin. Molecules. 2022;27:5156. https://doi.org/10.3390/molecules27165156.
Jędrzejczyk M, Sulik M, Mielczarek-Puta M, Lim GY, Podsiad M, Hoser J, Bednarczyk P, Struga M, Huczyński A. Anticancer activity of salinomycin quaternary phosphonium salts. Eur J Med Chem. 2025;282:117055. https://doi.org/10.1016/j.ejmech.2024.117055.
Andreeva OV, Voloshina AD, Lyubina AP, Garifullin BF, Sapunova AS, Amerhanova SK, IYu Strobykina, Belenok MG, Babaeva OB, Saifina LF, Semenov VE, Kataev VE. Acetylenyl substituted nucleic bases and their triphenylphosphonium (TPP) conjugates. Unexpected surge in cytotoxicity. Bioorg Chem. 2024;142:106959. https://doi.org/10.1016/j.bioorg.2023.106959.
Tyagi P, Singh M, Kumari H, Kumari A, Mukhopadhyay K. Bactericidal activity of curcumin I is associated with damaging of bacterial membrane. PloS One. 2015;10:e0121313. https://doi.org/10.1371/journal.pone.0121313.
Winkel JD, Gray DA, Seistrup KH, Hamoen LW, Strahl H. Analysis of antimicrobial-triggered membrane depolarization using voltage sensitive dyes. Front Cell Dev Biol. 2016;4:29. https://doi.org/10.3389/fcell.2016.00029.
Ma B, Zhang FahgC, Wang J, Luo M, Hou X. Z. Contemporaneous Measurement of outer and inner membrane permeability in Gram-negative bacteria. Bio-Protoc. 2020;10:e3548. https://doi.org/10.21769/BioProtoc.3548.
He Q, Liu D, Ashokkumar M, Ye X, Jin TZ, Guo M. Antibacterial mechanism of ultrasound against Escherichia coli: Alterations in membrane microstructures and properties. Ultrason Sonochem. 2021;73:105509. https://doi.org/10.1016/j.ultsonch.2021.105509.
Alonso B, Cruces R, Pérez A, Sánchez-Carrillo C, Guembe M. Comparison of the XTT and resazurin assays for quantification of the metabolic activity of Staphylococcus aureus biofilm. J Microbiol Methods. 2017;139:135–7. https://doi.org/10.1016/j.mimet.2017.06.004.
Wang X, Liu J, Chen J, Zhang M, Tian C, Peng X, Li G, Chang W, Lou H. Azole-triphenylphosphonium conjugates combat antifungal resistance and alleviate the development of drug-resistance. Bioorg Chem. 2021;110:e104771. https://doi.org/10.1016/j.bioorg.2021.104771.
Wang J, Liu X, Zhang X, Du S, Han X, Li J-Q, Xiao Y, Xu Z, Wu Q, Xu L, Qin Z. Fungicidal action of the triphenylphosphonium-driven succinate dehydrogenase inhibitors is mediated by reactive oxygen species and suggests an effective resistance management strategy. J Agric Food Chem. 2022;70:111–23. https://doi.org/10.1021/acs.jafc.1c05784.
Liu X, Liu H, Yin F, Li Y, Jiang J, Xiao Y, Wu Y, Qin Z. Phytopathogenic fungicidal activity and mechanism approach of three kinds of triphenylphosphonium salts. J Fungi. 2024;10:450. https://doi.org/10.3390/jof10070450.
Qin Y, Wang J, Lv Q, Han B. Recent progress in research on mitochondrion-targeted antifungal drugs: a Review. Antimicrob Agents Chemother. 2023;67:e00003–23. https://doi.org/10.1128/aac.00003-23.
Chang H-I, Yang MS, Liang M. The synthesis, characterization and antibacterial activity of quaternized poly(2,6-dimethyl-1,4-phenylene oxide)s modified with ammonium and phosphonium salts. React Funct Polym. 2010;70:944–50. https://doi.org/10.1016/j.reactfunctpolym.2010.09.005.
Davies JA, Anderson GK, Beveridge TJ, Clark HC. Chemical mechanism of the gram stain and synthesis of a new electron-opaque marker for electron microscopy which replaces the iodine mordant of the stain. J Bacteriol. 1983;156:837–45. https://doi.org/10.1128/jb.156.2.837-845.1983.
Wu M, Maier E, Benz R, Hancock REW. Mechanism of interaction of different classes of cationic antimicrobial peptides with planar bilayers and with the cytoplasmic membrane of Escherichia coli. Biochemistry. 1999;38:7235–42. https://doi.org/10.1021/bi9826299.
Li M, Nyantakyi SA, Gopal P, Aziz D, Dick T, Go M-L. Indolylalkyltriphenylphosphonium analogues are membrane-depolarizing mycobactericidal agents. ACS Med Chem Lett. 2017;8:1165–70. https://doi.org/10.1021/acsmedchemlett.7b00287.
Boix-Lemonche G, Lekka M, Skerlavaj B. A rapid fluorescence-based microplate assay to investigate the interaction of membrane active antimicrobial peptides with whole Gram-positive bacteria. Antibiotics. 2020;9:92 https://doi.org/10.3390/antibiotics9020092.
Silhavy TJ, Kahne D, Walker S. The bacterial cell envelope. Cold Spring Harb Perspect Biol. 2010;5:a000414. https://doi.org/10.1101/cshperspect.a000414.
Kima SJ, Chang J, Singh M. Peptidoglycan architecture of Gram-positive bacteria by solid-state NMR. Biochim Biophys Acta Biomembr. 2015;1848:350–62. https://doi.org/10.1016/j.bbamem.2014.05.031.
Garde S, Chodisetti PK, Reddy M. Peptidoglycan: Structure, Synthesis, and Regulation. EcoSal Plus 2021;9:domain 7. https://doi.org/10.1128/ecosalplus.ESP-0010-2020.
Heesterbeek DAC, Muts RM, van Hensbergen VP, de Saint Aulaire P, Wennekes T, Bardoel BW, van Sorge NM, Rooijakkers SHM. Outer membrane permeabilization by the membrane attack complex sensitizes Gramnegative bacteria to antimicrobial proteins in serum and phagocytes. PLoS Pathog. 2021;17:e1009227. https://doi.org/10.1371/journal.ppat.1009227.
Alegun O, Pandeya A, Cui J, Ojo I, Wei Y. Donnan potential across the outer membrane of Gram-negative bacteria and its effect on the permeability of Antibiotics. Antibiotics. 2021;10:701. https://doi.org/10.3390/antibiotics10060701.
Maher C, Hassan KA. The Gram-negative permeability barrier: tipping the balance of the in and the out. mBio. 2023;14:e01205–23. https://doi.org/10.1128/mbio.01205-23.
Muheim C, Götzke H, Eriksson AU, Lindberg S, Lauritsen I, Nørholm MHH, Daley DO. Increasing the permeability of Escherichia coli using MAC13243. Sci Rep. 2017;7:17629. https://doi.org/10.1038/s41598-017-17772-6.
Vergalli J, Bodrenko IV, Masi M, Moynie L, Acosta- Gutierrez S, Naismith JH, Davin-Regli A, Ceccarelli M, van den Berg B, Winterhalter M, Pages J-M. Porins and small- molecule translocation across the outer membrane of Gram-negative bacteria. Nat Rev Microbiol. 2020;18:164–76. https://doi.org/10.1038/s41579-019-0294-2.
Rojas ER, Billings G, Odermatt PD, Auer GK, Zhu L, Miguel A, Chang F, Weibel DB, Theriot JA, Huang KC. The outer membrane is an essential load-bearing element in Gram-negative bacteria. Nature. 2018;559:617–21. https://doi.org/10.1038/s41586-018-0344-3.
Egan AJF. Bacterial outer membrane constriction. Mol Microbiol. 2019;107:676–97. https://doi.org/10.1111/mmi.13908.
Pandit S, Fazilati M, Gaska K, Derouiche A, Nypelö T, Mijakovic I, Kádár R. The exo-polysaccharide component of extracellular matrix is essential for the viscoelastic properties of Bacillus subtilis biofilms. Int J Mol Sci. 2020;21:6755. https://doi.org/10.3390/ijms21186755.
Strempel N, Strehmel J, Overhage J. Potential application of antimicrobial peptides in the treatment of bacterial biofilm infections. Curr Pharm Des. 2015;21:67–84. https://doi.org/10.2174/1381612820666140905124312.
Starra CG, Ghimirea J, Guha S, Hoffmann JP, Wang YU, Sun L, Landreneau BN, Kolansky ZD, Kilanowski-Doroh IM, Sammarco MC, Morici LA, Wimley WC. Synthetic molecular evolution of host cell-compatible, antimicrobial peptides effective against drug-resistant, biofilm-forming bacteria. Proc Natl Acad Sci USA. 2020;117:8437–48. https://doi.org/10.1073/pnas.1918427117.
Xu Z, Liang Y, Lin S, Chen D, Li B, Li B, Deng Y. Crystal Violet and XTT assays on Staphylococcus aureus biofilm quantification. Curr Microbiol. 2016;73:474–82. https://doi.org/10.1007/s00284-016-1081-1.
Corte L, Pierantoni DC, Tascini C, Roscini L, Cardinali G. Biofilm specific activity: A measure to quantify microbial biofilm. Microorganisms. 2019;7:73. https://doi.org/10.3390/microorganisms7030073.
Acknowledgements
We are grateful to the Assigned Spectral-Analytical Center of FRC Kazan Scientific Center of RAS for technical assistance in research.
Funding
This research was funded by the Russian Science Foundation (grant no. 24-13-00006).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Andreeva, O.V., Voloshina, A.D., Lyubina, A.P. et al. Antimicrobial activity of triphenylphosphonium (TPP) conjugates of alkynyl−substituted nucleic bases and their analogues. J Antibiot 78, 731–756 (2025). https://doi.org/10.1038/s41429-025-00864-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41429-025-00864-1
This article is cited by
-
In vitro cytotoxicity evaluation of triphenylphosphonium (TPP) conjugates of some acetylenated nucleic bases and their analogues
Medicinal Chemistry Research (2025)