Abstract
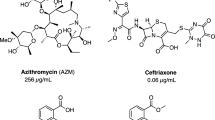
Neisseria gonorrhoeae is the bacterium that causes gonorrhea, and multidrug resistance is becoming progressively more severe in many countries. Therefore, limited drugs are available for treatment. It is predicted that further drug resistance will be acquired, making treatment still more difficult, so there is an urgent need to develop new drugs. We discovered three compounds with a new kalafungin-type pyranonaphthoquinone skeleton, thiofrenomycins A-C, that exhibit strong antibacterial activity against N. gonorrhoeae in a culture solution of Streptomyces sp. MM863L-181F9 derived from fallen leaves. The absolute stereochemistry of these compounds was determined using X-ray crystal structure analysis. These substances exhibit minimal inhibitory concentrations of 0.125–16 µg/mL against N. gonorrhoeae.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
WHO: Global progress report on HIV, viral hepatitis and sexually transmitted infections, 2021. https://www.who.int/publications/i/item/9789240027077.
Unemo M, et al. Gonorrhoea. Nat Rev Dis Prim. 2019;5:79.
WHO: Treatment of Neisseria gonorrhoeae. https://iris.who.int/bitstream/handle/10665/246114/9789241549691-eng.pdf.
Unemo M, et al. WHO global antimicrobial resistance surveillance for Neisseria gonorrhoeae 2017–18: a retrospective observational study. Lancet Microbe. 2021;2:e627–636.
Xiu L, Zhang L, Peng J. Surge in ceftriaxone-resistant Neisseria gonorrhoeae FC428-like strains, Asia-Pacific region, 2015−2022. Emerg Infect Dis. 2024;30:1683–6.
Fifer H, Doumith M, Rubinstein L, Mitchell L, Wallis M. Ceftriaxone-resistant Neisseria gonorrhoeae detected in England, 2015–24: an observational analysis. J Antimicrob Chemother. 2024;79:3332–9.
Melendez JH, et al. Local emergence and global evolution of Neisseria gonorrhoeae with high-level resistance to azithromycin. Antimicrob Agents Chemother. 2024;68:e0092724.
Eyre DW, et al. Gonorrhoea treatment failure caused by a Neisseria gonorrhoeae strain with combined ceftriaxone and high-level azithromycin resistance, England, February 2018. Eur Surveill. 2018;23:1800323.
Caméléna F, et al. Emergence of extensively drug-resistant Neisseria gonorrhoeae, France, 2023. Emerg Infect Dis. 2024;30:1903–6.
Wagenlehner F, et al. Oral gepotidacin versus nitrofurantoin in patients with uncomplicated urinary tract infection (EAGLE-2 and EAGLE-3): two randomised, controlled, double-blind, double-dummy, phase 3, non-inferiority trials. Lancet. 2024;403:741–55.
Ross JDC, et al. Oral gepotidacin for the treatment of uncomplicated urogenital gonorrhoea (EAGLE-1): a phase 3 randomised, open-label, non-inferiority, multicentre study. Lancet. 2025;405:1608–20.
Wang XC, et al. Frenolicins C-G, Pyranonaphthoquinones from sp RM-4-15. J Nat Prod. 2013;76:1441–7.
Tsukamoto M, et al. New cytotoxic agents, BE-52440A and B, produced by a streptomycete. J Antibiotics. 2000;53:687–93.
Tatsuta K, Suzuki Y, Toriumi T, Furuya Y, Hosokawa S. The first total synthesis and structural determination of (+)-BE-52440A. Tetrahedron Lett. 2007;48:8018–21.
Derewacz DK, et al. Structure and Stereochemical Determination of Hypogeamicins from a Cave-Derived Actinomycete. J Nat Prod. 2014;77:1759–63.
Ding X, et al. Crepidamycins A-E, pyranonaphthoquinones from endophytic Streptomyces sp. MG-F-1 of Dendrobium crepidatum by the co-culture strategy. Phytochem. 2025;233:114404.
Nakayama S, et al. New ceftriaxone- and multidrug-resistant Neisseria gonorrhoeae strain with a novel mosaic penA gene isolated in Japan. Antimicrob Agents Chemother. 2016;60:4339–41.
Yahara K, et al. Genomic surveillance of Neisseria gonorrhoeae to investigate the distribution and evolution of antimicrobial-resistance determinants and lineages. Microb Genomics. 2018;4:e000205.
Zarantonelli L, Borthagaray G, Lee EH, Shafer WM. Decreased azithromycin susceptibility of Neisseria gonorrhoeae due to mtrR mutations. Antimicrob Agents Chemother. 1999;43:2468–72.
Veal WL, Nicholas RA, Shafer WM. Overexpression of the MtrC- MtrD-MtrE efflux pump due to an mtrR mutation is required for chromosomally mediated penicillin resistance in Neisseria gonorrhoeae. J Bacteriol. 2002;184:5619–24.
Naysmith BJ, Hume PA, Sperry J, Brimble MA. Pyranonaphthoquinones – isolation, biology and synthesis: an update. Nat Prod Rep. 2017;34:25–61.
Ye Q, et al. Frenolicin B targets peroxiredoxin 1 and glutaredoxin 3 to trigger ROS/4E-BPl-mediated antitumor effects. Cell Chem Biol. 2019;26:366–77.
Acknowledgements
We thank Y. Kubota, Y. Takahashi and K. Iijima for technical assistance in determining the structure of thiofrenomycins. We also thank Y. Shibuya for technical support for the genetic modification of N. gonorrhoeae strains and R. Onodera for cytotoxicity assay. We gratefully acknowledge the contributions of the researchers and institutions who provided bacterial strains for this study. Their support was crucial for the success of this research. We thank Laura Murray, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kimura, T., Ishizaki, Y., Umekita, M. et al. Thiofrenomycins, new kalafungin-type pyranonaphthoquinone skeleton with sulfide linkage from Streptomyces sp. MM863L-181F9. J Antibiot 79, 67–73 (2026). https://doi.org/10.1038/s41429-025-00883-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41429-025-00883-y