Abstract
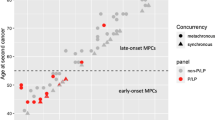
Patients with tumors displaying high microsatellite instability (MSI-H) but no germline MMR inactivation are suspected for Lynch-like syndrome (LLS). To explore the involvement of acquired somatic MMR alteration as a cause, we screened 113 patient tumor samples for MMR gene variations and loss of heterozygosity. Somatic MMR alterations were found in 85.8% of patients including “double hits” in 63.7% of patients, mainly diagnosed with colon and endometrial cancers. Interestingly, 37.5% of them were under the age of 50, and seven patients were under 30. Somatic alterations were mainly attributed to the MLH1, MSH2 genes, likely reflecting the functional importance of these key MMR genes. Pathogenic variants co-existed in other cancer genes in particular the APC gene displaying a characteristic MMR deficiency-related “mutational signature”, indicating that it may be inactivated owing to MMR deficiency. We speculated that APC inactivation could trigger an accelerated malignant transformation underlying early-onset cancers. Our findings provide further insight into the mechanisms underlying LLS, somatic MMR inactivation being a major cause for early-onset LLS through pathways differing from those involved in late-onset sporadic cases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Bonneville R, Krook MA, Kautto EA, Miya J, Wing MR, Chen HZ, et al. Landscape of microsatellite instability across 39 cancer types. JCO Precis Oncol. 2017; 2017:PO.17.00073.
Carethers JM. Differentiating Lynch-like from Lynch syndrome. Gastroenterology. 2014;146:602–4.
Mensenkamp AR, Vogelaar IP, van Zelst-Stams WA, Goossens M, Ouchene H, Hendriks-Cornelissen SJ, et al. Somatic mutations in MLH1 and MSH2 are a frequent cause of mismatch-repair deficiency in Lynch syndrome-like tumours. Gastroenterology. 2014;146:643–6.
Geurts-Giele WR, Leenen CH, Dubbink HJ, Meijssen IC, Post E, Sleddens HF, et al. Somatic aberrations of mismatch repair genes as a cause of microsatellite-unstable cancers. J Pathol. 2014;234:548–59.
Haraldsdottir S, Hampel H, Tomsic J, Frankel WL, Pearlman R, de la Chapelle A, et al. Colon and endometrial cancers with mismatch repair deficiency can arise from somatic, rather than germline, mutations. Gastroenterology. 2014;147:1308–16.
Huang J, Papadopoulos N, McKinley AJ, Farrington SM, Curtis LJ, Wyllie AH, et al. APC mutations in colorectal tumours with mismatch repair deficiency. Proc Natl Acad Sci USA. 1996;93:9049–54.
Olschwang S, Hamelin R, Laurent-Puig P, Thuille B, De RY, Li YJ, et al. Alternative genetic pathways in colorectal carcinogenesis. Proc Natl Acad Sci USA. 1997;94:12122–7.
Morak M, Heidenreich B, Keller G, Hampel H, Laner A, de la Chapelle A, et al. Biallelic MUTYH mutations can mimic Lynch syndrome. Eur J Hum Genet. 2014;22:1334–7.
Jansen AM, Van WT, van den Akker BE, Ventayol GM, Ruano D, Tops CM, et al. Combined mismatch repair and POLE/POLD1 defects explain unresolved suspected Lynch syndrome cancers. Eur J Hum Genet. 2016;24:1089–92.
Bonadona V, Bonaiti B, Olschwang S, Grandjouan S, Huiart L, Longy M, et al. Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in Lynch syndrome. JAMA. 2011;305:2304–10.
Sourrouille I, Coulet F, Lefevre JH, Colas C, Eyries M, Svrcek M, et al. Somatic mosaicism and double somatic hits can lead to MSI colorectal tumours. Fam Cancer. 2013;12:27–33.
Rosty C, Clendenning M, Walsh MD, Eriksen SV, Southey MC, Winship IM, et al. Germline mutations in PMS2 and MLH1 in individuals with solitary loss of PMS2 expression in colorectal carcinomas from the Colon Cancer Family Registry Cohort. BMJ. 2016;6:e010293.
Joly MO, Attignon V, Saurin JC, Desseigne F, Leroux D, Martin-Denavit T, et al. Somatic MMR gene mutations as a cause for MSI-H sebaceous neoplasms in Muir-Torre syndrome-like patients. Hum Mutat. 2015;36:292–5.
Kadyrov FA, Dzantiev L, Constantin N, Modrich P. Endonucleolytic function of MutLalpha in human mismatch repair. Cell. 2006;126:297–308.
Ten Broeke SW, van der Klift HM, Tops CMJ, Aretz S, Bernstein I, Buchanan DD, et al. Cancer risks for PMS2-associated Lynch Syndrome. J Clin Oncol. 2018;36:2961–8.
Fearon ER, Vogelstein B. A genetic model for colorectal tumourigenesis. Cell. 1990;61:759–67.
Schell MJ, Yang M, Teer JK, Lo FY, Madan A, Coppola D, et al. A multigene mutation classification of 468 colorectal cancers reveals a prognostic role for APC. Nat Commun. 2016;7:11743.
The cancer Genome Atlas. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487:330–7.
Miyoshi Y, Nagase H, Ando H, Horii A, Ichii S, Nakatsuru S, et al. Somatic mutations of the APC gene in colorectal tumours: mutation cluster region in the APC gene. Hum Mol Genet. 1992;1:229–33.
Helleday T, Eshtad S, Nik-Zainal S. Mechanisms underlying mutational signatures in human cancers. Nat Rev Genet. 2014;15:585–98.
Acknowledgements
We thank Drs. E. Barouk-Simonet, B. Buecher, MN. Bonnet-Dupeyron, O. Caron, C. Corsini, F. Desseigne, M. Dhooge, S. Fert Ferrer, S. Giraud, M. Lebrun, D. Leroux, JM. Limacher, A. Lortholary, D. Malka, T. Martin-Denavit, S. Olschwang, F. Prieur, JC. Saurin, and their genetic counseling assistants for case collection and for providing clinical information. We thank Drs. O. Cabaret, C. Ferraro-Peyret, L. Golmard, C. Maugard for tumor sampling and DNA preparation. And we thank Mrs. Brigitte Manship for manuscript editing assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lefol, C., Sohier, E., Baudet, C. et al. Acquired somatic MMR deficiency is a major cause of MSI tumor in patients suspected for “Lynch-like syndrome” including young patients. Eur J Hum Genet 29, 482–488 (2021). https://doi.org/10.1038/s41431-020-00778-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41431-020-00778-6
This article is cited by
-
Tissue-based genomic profiling of 300,000 tumors highlights the detection of variants with low allele fraction
npj Precision Oncology (2025)
-
A tumor focused approach to resolving the etiology of DNA mismatch repair deficient tumors classified as suspected Lynch syndrome
Journal of Translational Medicine (2023)
-
The European Journal of Human Genetics is turning 30: a selection of major cancer genetics papers published by the Journal
European Journal of Human Genetics (2022)
-
Somatic hits in mismatch repair genes in colorectal cancer among non-seminoma testicular cancer survivors
British Journal of Cancer (2022)