Abstract
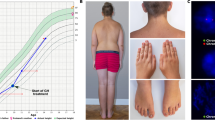
The founder variant DHCR7:c.964-1G>C causing autosomal recessive Smith–Lemli–Opitz (SLOS) was introduced into the Israeli preconception carrier program for Ashkenazi Jews in 2017 because of the high carrier frequency in this population (2.3%). Other disease-causing variants in DHCR7 are relatively rare in Israeli population. Discrepancy between the carrier frequency and disease prevalence raises the question of the actual risks for affected offspring for couples detected by the screening program. We performed a literature review of all relevant publications regarding homozygous DHCR7:c.964-1G>C fetuses/patients. We also collected clinical data about couples identified in the national screening program, including reproductive history. Out of 32 homozygous fetuses, six died in utero, 11 pregnancies were terminated during second trimester, and 15 children were born. All died between first days of life till 3 months of age. Reproductive history of SLOS-at-risk couples showed that after correction for ascertainment bias, out of 61 pregnancies, there was an absence of affected fetuses/children and an excess of miscarriages even if assumed that all the homozygous fetuses were miscarried. Out of these, eight families were Israelis, they had a total of one sick child, 21 healthy children, and 21 miscarriages. Our observations support the previous knowledge that homozygosity for c.964-1G>C in DHCR7 leads to a severe phenotype or early miscarriage. An unexpected observation was the excess of early miscarriages. This phenomenon is unclear and awaits further studies.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Nowaczyk MJ, Irons MB. Smith–Lemli–Opitz syndrome: phenotype, natural history, and epidemiology. Am J Med Genet C Semin Med Genet. 2012;160C:250–62.
Jira PE, Waterham HR, Wanders RJ, Smeitink JA, Sengers RC, Wevers RA. Smith–Lemli–Opitz syndrome and the DHCR7 gene. Ann Hum Genet. 2003;67:269–80.
Lazarin GA, Haque IS, Evans EA, Goldberg JD. Smith–Lemli–Opitz syndrome carrier frequency and estimates of in utero mortality rates. Prenat Diagn. 2017;37:350–5.
Witsch-Baumgartner M, Fitzky BU, Ogorelkova M, Kraft HG, Moebius FF, Glossmann H, et al. Mutational spectrum in the Delta7-sterol reductase gene and genotype-phenotype correlation in 84 patients with Smith–Lemli–Opitz syndrome. Am J Hum Genet. 2000;66:402–12.
Nowaczyk MJ, Waye JS, Douketis JD. DHCR7 mutation carrier rates and prevalence of the RSH/Smith–Lemli–Opitz syndrome: where are the patients? Am J Med Genet A. 2006;140:2057–62.
Battaile KP, Battaile BC, Merkens LS, Maslen CL, Steiner RD. Carrier frequency of the common mutation IVS8-1G>C in DHCR7 and estimate of the expected incidence of Smith–Lemli–Opitz syndrome. Mol Genet Metab. 2001;72:67–71.
Lek M, Karczewski KJ, Minikel EV, Samocha KE, Banks E, Fennell T, et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature. 2016;536:285–91.
Zlotogora J, Grotto I, Kaliner E, Gamzu R. The Israeli national population program of genetic carrier screening for reproductive purposes. Genet Med. 2016;18:203–6.
Quélin C, Loget P, Verloes A, Bazin A, Bessières B, Laquerrière A, et al. Phenotypic spectrum of fetal Smith–Lemli–Opitz syndrome. Eur J Med Genet. 2012;55:81–90.
Travessa A, Dias P, Rocha P, Sousa AB. Prenatal diagnosis of holoprosencephaly associated with Smith–Lemli–Opitz syndrome (SLOS) in a 46,XX fetus. Taiwan J Obstet Gynecol. 2017;56:541–4.
Moosa S, Loeys B, Altmüller J, Mortier G, Nürnberg P, Li Y, et al. Metatarsal bony syndactyly in 2 fetuses with Smith–Lemli–Opitz syndrome: an under-recognized part of the clinical spectrum. Clin Genet. 2017;92:342–3.
Nowaczyk MJ, Farrell SA, Sirkin WL, Velsher L, Krakowiak PA, Waye JS, et al. Smith–Lemli–Opitz (RHS) syndrome: holoprosencephaly and homozygous IVS8-1G->C genotype. Am J Med Genet. 2001;103:75–80.
Goldenberg A, Chevy F, Bernard C, Wolf C, Cormier-Daire V. Clinical characteristics and diagnosis of Smith–Lemli–Opitz syndrome and tentative phenotype–genotype correlation: report of 45 cases. Arch Pediatr. 2003;10:4–10.
Jira PE, Wanders RJ, Smeitink JA, De Jong J, Wevers RA, Oostheim W, et al. Novel mutations in the 7-dehydrocholesterol reductase gene of 13 patients with Smith–Lemli–Opitz syndrome. Ann Hum Genet. 2001;65:229–36.
Lanthaler B, Steichen-Gersdorf E, Kollerits B, Zschocke J, Witsch-Baumgartner M. Maternal ABCA1 genotype is associated with severity of Smith–Lemli–Opitz syndrome and with viability of patients homozygous for null mutations. Eur J Hum Genet. 2013;21:286–93.
Balogh I, Koczok K, Szabó GP, Török O, Hadzsiev K, Csábi G, et al. Mutational spectrum of smith-lemli-opitz syndrome patients in hungary. Mol Syndromol. 2012;3:215–22.
Donoghue SE, Pitt JJ, Boneh A, White SM. Smith–Lemli–Opitz syndrome: clinical and biochemical correlates. J Pediatr Endocrinol Metab. 2018;31:451–9.
Scalco FB, Correa-Cerro LS, Wassif CA, Porter FD, Moretti-Ferreira D. DHCR7 mutations in Brazilian Smith–Lemli–Opitz syndrome patients. Am J Med Genet A. 2005;136:278–81.
Statistical Abstracts of Israel. Jerusalem: Central Bureau of Statistics; 2018.
Chen R, Shi L, Hakenberg J, Naughton B, Sklar P, Zhang J, et al. Analysis of 589,306 genomes identifies individuals resilient to severe Mendelian childhood diseases. Nat Biotechnol. 2016;34:531–8.
Rossen LM, Ahrens KA, Branum AM. Trends in risk of pregnancy loss among US women, 1990–2011. Paediatr Perinat Epidemiol. 2018;32:19–29.
Dhaded SM, Somannavar MS, Jacob JP, McClure EM, Vernekar SS, Yogesh Kumar S, et al. Early pregnancy loss in Belagavi, Karnataka, India 2014–2017: a prospective population-based observational study in a low-resource setting. Reprod Health. 2018;15(Suppl 1):95.
Ammon Avalos L, Galindo C, Li DK. A systematic review to calculate background miscarriage rates using life table analysis. Birth Defects Res A Clin Mol Teratol. 2012;94:417–23.
Korade Z, Genaro-Mattos TC, Tallman KA, Liu W, Garbett KA, Koczok K. et al. Vulnerability of DHCR7+/− mutation carriers to aripiprazole and trazodone exposure. J Lipid Res. 2017;58:2139–46.
Acknowledgements
We would like to thank our collaborators all across the country that searched for relevant data. Data that were not yet submitted, were deposited in ClinVar. accession number for DHCR7 variant in ClinVar: SCV000998809.1 (There are 38 citations regarding the variant at https://www.ncbi.nlm.nih.gov/clinvar/variation/93725/).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Daum, H., Meiner, V., Michaelson-Cohen, R. et al. Smith–Lemli–Opitz syndrome: what is the actual risk for couples carriers of the DHCR7:c.964-1G>C variant?. Eur J Hum Genet 28, 938–942 (2020). https://doi.org/10.1038/s41431-020-0577-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41431-020-0577-0
This article is cited by
-
Miscarriage risk assessment: a bioinformatic approach to identifying candidate lethal genes and variants
Human Genetics (2024)
-
Mendelian inheritance revisited: dominance and recessiveness in medical genetics
Nature Reviews Genetics (2023)
-
Deficit of homozygosity among 1.52 million individuals and genetic causes of recessive lethality
Nature Communications (2023)