Abstract
Aims/objectives
This systematic review aimed to evaluate the effectiveness of auxiliary aids—Transcutaneous Electrical Nerve Stimulation (TENS), vibrotactile devices, and Low-Level Laser Therapy (LLLT) in reducing pain and anxiety during dental local anesthesia in pediatric patients.
Methods
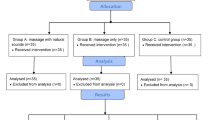
The review followed PRISMA guidelines, employing a comprehensive search strategy across multiple databases (PubMed, Cochrane, EBSCO, LILACS, Google Scholar, and Embase) from 2014 to July 2024. Eligibility criteria were based on the PICOS framework, focusing on randomized clinical trials and clinical studies involving pediatric patients undergoing dental procedures with local anesthesia. The interventions included TENS, vibrotactile devices, or LLLT. Pain and anxiety were assessed using validated scales such as the Wong-Baker Faces Pain Rating Scale and physiological measures like heart rate.
Results
Nineteen studies with a total of 1094 pediatric patients aged 4–12 were included. TENS and vibrotactile devices consistently showed significant reductions in pain and anxiety compared to standard methods. LLLT results were more variable, with some studies reporting significant pain reduction while others showed no significant difference. Meta-analysis was not possible due to heterogeneity among the studies. Overall, TENS and vibrotactile devices were more effective in alleviating injection-related pain, especially when combined with cold applications or topical anesthetics.
Discussion
The findings highlight the potential of these auxillary aids as non-invasive and effective adjuncts for reducing pain and anxiety in pediatric dental procedures. LLLT showed mixed outcomes, likely due to variability in application protocols, suggesting a need for standardized methods. While all interventions demonstrated promise, inconsistencies in study designs and subjective measures limit the generalizability of the results.
Conclusions
TENS and vibrotactile devices are effective auxiliary aids for reducing pain and anxiety during dental local anesthesia in children. Further research is required to optimize LLLT protocols and standardize intervention applications to achieve consistent results across studies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The data supporting this article can be made available by the corresponding author upon request.
References
Stevens BJ, Harrison D, Rashotte J, Yamada J, Abbott LK, Coburn G, et al. Pain assessment and intensity in hospitalized children in Canada. J Pain. 2012;13:857–65.
Taddio A, Appleton M, Bortolussi R, Chambers C, Dubey V, Halperin S, et al. Reducing the pain of childhood vaccination: an evidence-based clinical practice guideline.Can Med Assoc J = J de l’Assoc Med Canadienne. 2010;182:E843–855.
Taddio A, Chambers CT, Halperin SA, Ipp M, Lockett D, Rieder MJ, et al. Inadequate pain management during routine childhood immunizations: the nerve of it. Clin Ther. 2009;31:S152.
Berde Charles, Wolfe Joanne. Pain, anxiety, distress, and suffering: interrelated, but not interchangeable. J Pediatr. 2003;ume 142:361–3. https://doi.org/10.1067/mpd.2003.194.
Veneva ER, Belcheva A. Local anesthesia in pediatric patients –a review of current and alternative methods, devices and techniques. Folia Med (Plovdiv). 2018;60:381–8.
Şermet Elbay Ü, Elbay M, Kaya C, Uğurluel C, Baydemir C. The Efficacy of Dental Vibe injection comfort system producing vibration impuls to reduce injection pain of palatal local infiltration anesthesia in children. J Dent Sci. 2015;21:207–15.
Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150:971–9. https://doi.org/10.1126/science.150.3699.971.
Midha V, Midha V, Dua R, et al. Auxiliary aids to alleviate pain and anxiety during local anesthesia administration: a comparative study. Int J Clin Pediatr Dent. 2021;14:104–8.
Bhawana DR. Comparison of vibraject with conventional syringe during local anesthesia administration. IOSR J Dent Med Sci. 2019;18:08–12.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Locker D, Liddell A, Dempster L, Shapiro D. Age of onset of dental anxiety. J Dent Res. 1999;78:790–6.
Ayer W. Psychology and Dentistry: Mental Health Aspects of Patient Care. New York: Haworth Press, 2005.
Klingberg G, Berggren U, Carlsson SG, Noren JG. Child dental fear: cause-related factors and clinical eKects. Eur J Oral Sci. 1995;103:405–12.
van Wijk AJ, Makkes PC. Highly anxious dental patients report more pain during dental injections. Br Dent J. 2008;205:E7142–3.
Skaret E, Kvale G, Raadal M. General self-eKicacy, dental anxiety and multiple fears among 20-year- olds in Norway. Scand J Psychol. 2003;44:331–7.
Townend E, Dimigen G, Fung D. A clinical study of child dental anxiety. Behav Res Ther. 2000;38:31–46. https://doi.org/10.1016/s0005-7967(98)00205-8.
Versloot J, Veerkamp J, Hoogstrate J. Dental anxiety and psychological functioning in children: its relationship with behaviour during treatment. Eur Arch Paediatr Dent. 2008;9:36–40.
Majstorovic M, Veerkamp JS. Relationship between needle phobia and dental anxiety. J Dent Child. 2004;71:201–5.
Vika M, Skaret E, Raadal M, Ost LG, Kvale G. Fear of blood, injury, and injections, and its relationship to dental anxiety and probability of avoiding dental treatment among 18-yearolds in Norway. Int J Paediatr Dent. 2008;18:163–9.
Weisman SJ, Bernstein B, Schechter N. Consequences of inadequate analgesia during painful procedures in children. Arch Pediatr Adolesc Med. 1998;152:147–9.
Ashley PF, Williams CECS, Moles DR, Parry J. Sedation versus general anaesthesia for provision of dental treatment to patients younger than 18 years. Cochrane Database Syst Rev. 2015. https://doi.org/10.1002/14651858.CD006334.pub4.
Campbell C, Soldani F, Busuttil-Naudi A, Chadwick B. Update of non-pharmacological behavior management guideline. Clinical Guidelines in Paediatric Dentistry. Br Soc Paediatr Dent. https://api.semanticscholar.org/CorpusID:52027183
Fayle S, Crawford PJ. Making dental treatment acceptable to children. Dent Rofile. 1997;4:18–22.
Berg J. Topical anesthetic before primary molar buccal anesthesia is not better than placebo in reducing child's pain perception. J Evid Based Dent Pract. 2007;7:116–7.
Meechan JG. Pain control in local analgesia. Eur Arch Paediatr Dent. 2009;10:71–6.
Krikken JB, van Wijk AJ, ten Cate JM, Veerkamp JS. Measuring dental fear using the CFSS-DS. Do children and parents agree? Int J Paediatr Dent. 2010;23:94–100.
Patil SB, Popali DD, Bondarde PA, Khandare NS, Kothari AR, Chawla PS, et al. Comparative evaluation of the effectiveness of different pain- alleviating methods before local anesthetic administration in children of 6 to 12 years of age: a clinical study. Int J Clin Pediatr Dent. 2021;14:447–53. https://doi.org/10.5005/jp-journals-10005-1998.
Singh K, Jhingan P, Mathur S, Malik M, Kashyap K. Intercomparison of efficacy of transcutaneous electrical nerve stimulation and precooling vibration device on pain and anxiety management during administration of local anesthesia injection in 6-12-year-olds. Int J Clin Pediatr Dent. 2024;17:297–302. https://doi.org/10.5005/jp-journals-10005-2807.
Shilpapriya M, Jayanthi M, Reddy VN, Sakthivel R, Selvaraju G, Vijayakumar P. Effectiveness of new vibration delivery system on pain associated with injection of local anesthesia in children. J Indian Soc Pedod Prev Dent. 2015;33:173–6. https://doi.org/10.4103/0970-4388.160343.
Alanazi KJ, Pani S, AlGhanim N. Efficacy of external cold and a vibrating device in reducing discomfort of dental injections in children: a split mouth randomised crossover study. Eur Arch Paediatr Dent. 2019;20:79–84. https://doi.org/10.1007/s40368-018-0399-8.
Tandon S, Kalia G, Sharma M, Mathur R, Rathore K, Gandhi M. Comparative evaluation of mucosal vibrator with topical anesthetic gel to reduce pain during administration of local anesthesia in pediatric patients: an in vivo study. Int J Clin Pediatr Dent. 2018;11:261–5. https://doi.org/10.5005/jp-journals-10005-1523.
Bilsin E, Güngörmüş Z, Güngörmüş M. The efficacy of external cooling and vibration on decreasing the pain of local anesthesia injections during dental treatment in children: a randomized controlled 375 study. J Perianesth Nurs. 2020;35:44–47. https://doi.org/10.1016/j.jopan.2019.06.007.
Hegde KM, Neeraja R, Srinivasan I, Murali Krishna DR, Melwani A, Radhakrishna S. Effect of vibration during local anesthesia administration on pain, anxiety, and behavior of pediatric patients aged 6-11 years: a crossover 379 split-mouth study. J Dent Anesth Pain Med. 2019;19:143–9. https://doi.org/10.17245/jdapm.2019.19.3.143.
Felemban O, Oghli AR, Alsaati I, Alattas LK, Olwi AM, Bagher SM. The effect of Dental Vibe on pain and discomfort during local anesthesia in children: a randomized clinical trial. Quintessence Int. 2021;52:434–43. https://doi.org/10.3290/j.qi.b912695.
Subramaniam P, Ghai SK. Efficacy of an innovative device in reducing discomfort during local anesthesia administration in children: a clinical study. Int J Clin Pediatr Dent. 2021;14:353–6. https://doi.org/10.5005/jp-journals-10005-1948.
Jain N, Juneja P, Masih U, Bhushan AKB, Bhaduaria US, Badjatya K. Efficacy of external cold and a vibrating device in reducing pain and anxiety during local anaesthesia. J Fam Med Prim Care. 2021;10:4017–22. https://doi.org/10.4103/jfmpc.jfmpc_305_21.
Uçar G, Şermet Elbay Ü, Elbay M. Effects of low level laser therapy on injection pain and anesthesia efficacy during local anesthesia in children: A randomized clinical trial. Int J Paediatr Dent. 2022;32:576–84. https://doi.org/10.1111/ipd.12936.
Khan BS, Setty JV, Srinivasan I, Kibriya S, Anu S, Radhakrishna S, et al. Low-level laser therapy to alleviate pain of local anesthesia injection in children: a randomized control trial. Int J Clin Pediatr Dent. 2023;16:283–7. https://doi.org/10.5005/jp-journals-10005-2699.
Ananthu H, Rao A, Natarajan S, Yarmunja Mahabala K, Nayak A. Efficacy of an external cold and vibrating device in reducing discomfort during the administration of an inferior alveolar nerve block in children: a split-mouth randomised crossover study. F1000Res. 2023;12:984 https://doi.org/10.12688/f1000research.138340.1.
Shetty A, Naik SS, Patil RB, Valke PS, Mali S, Patil D. Effectiveness of an extraoral cold and vibrating device in reducing pain perception during deposition of local anesthesia in pediatric patients aged 3-12 years: a split-mouth crossover study. J Dent Anesth Pain Med. 2023;23:317–25. https://doi.org/10.17245/jdapm.2023.23.6.317.
AmruthaVarshini I, Vinay C, Uloopi KS, RojaRamya KS, Chandrasekhar R, Penmatsa C. Effectiveness of pre-cooling the injection site, laser biostimulation, and topical local anesthetic gel in reduction of local anesthesia injection pain in children. Int J Clin Pediatr Dent. 2021;14:81–83. https://doi.org/10.5005/jp-journals-10005-1913.
Shekarchi F, Nokhbatolfoghahaei H, Chiniforush N, Mohaghegh S, Haeri Boroojeni HS, Amini S.et al. Evaluating the preemptive analgesic effect of photo-biomodulation therapy on pain perception during local anesthesia injection in children: a split-mouth triple-blind randomized controlled clinical trial. Photoche Photobiol. 2022;98:1195–200. https://doi.org/10.1111/php.13605.
Elbay M, Elbay ÜŞ, Kaya E, Kalkan ÖP. Effects of photobiomodulation with different application parameters on injection pain in children: a randomized clinical trial. J Clin Pediatr Dent. 2023;47:54–62. https://doi.org/10.22514/jocpd.2023.035.
Seraj B, Bavaghar A, Hakimiha N, Hosseini Z, Kharazifard MJ, Ghadimi S. Effect of photobiomodulation therapy with an 810-nm diode laser on pain perception associated with dental injections in children: a double-blind randomized controlled clinical trial. J Lasers Med Sci. 2023;14:e19. https://doi.org/10.34172/jlms.2023.19.
Funding
The author(s) received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
SB conceived the idea, collected the data, analyzed the data, and led the writing. GM conceived the idea, analyzed and resolved any differences in opinion, also contributing to the writing. SA assisted in resolving differences and helped with data analysis. PS, AS, GY, and SP were responsible for data collection and performing data extraction and analysis. AS additionally led the writing alongside SB.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Saxena, B., Goswami, M., Saxena, A. et al. Auxillary aids for pain and anxiety reduction during dental local anesthesia in pediatric patients: a systematic review. Evid Based Dent 26, 114–115 (2025). https://doi.org/10.1038/s41432-024-01094-4
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41432-024-01094-4