Abstract
Purpose
To investigate fluorescence lifetime imaging ophthalmoscopy (FLIO) findings in preclinical Alzheimer’s disease (AD).
Methods
This prospective, observational study enrolled patients with early AD undergoing Alzheimer’s biomarker analysis and matched controls. Alzheimer-associated parameters (β-amyloid [Aβ], total tau in cerebrospinal fluid [CSF], Mini-Mental Status Examination [MMSE], etc.), risk factor-associated data (body mass index [BMI], hypertension, lipid profile, etc.), ganglion cell layer plus inner plexiform layer (GCIPL) thickness in structural optical coherence tomography (OCT), OCT angiography data, and FLIO-derived parameters (τm, τ1, τ2, and τ3) in short and long spectral channels (SSC and LSC) were compared and correlated between the two groups. Additional analyses were performed separately within subgroups of phakic and pseudophakic.
Results
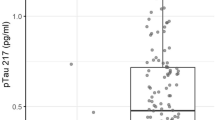
A total of 28 eyes from 15 subjects (8 control and 7 AD) were included in this analysis. In FLIO parameters, τm in AD group showed longer lifetimes compared to the controls in phakic subjects (593.9 ± 93.3, 454.4 ± 38.6 ps; 475.0 ± 71.6, 394.1 ± 28.2 ps in SSC and LSC of AD and control groups, respectively, p = 0.036 and 0.024). Aβ, tau in CSF, and GCIPL thickness correlated with τm in the LSC for phakic subjects (r = −0.611 to 0.562, p < 0.05 for all), but only the GCIPL thickness showed a correlation with FLIO parameters in pseudophakic subjects (r = −0.893 to −0.795, p < 0.001 for all).
Conclusion
FLIO-derived parameters appear to correlate with Aβ, tau levels in the CSF, and GCIPL thickness on OCT in AD patients. If these findings can be validated in future longitudinal studies, FLIO may prove to be useful as a simple, non-invasive diagnostic tool for AD.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Prince PM, Ali G, Ali G. World Alzheimer Report 2015. The global impact of dementia. London: Alzheimers Disease International; 2015.
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263–9.
Villemagne VL, Burnham S, Bourgeat P, Brown B, Ellis KA, Salvado O, et al. Amyloid β deposition, neurodegeneration and cognitive decline in sporadic Alzheimer’s disease: a prospective cohort study. Lancet Neurol. 2013;12:357–67.
Lim YY, Maruff P, Getter C, Snyder PJ. Discloure of PET amyloid imaging results: a preliminary study of safety and tolerability. Alzheimers Dement. 2016;12:454–8.
Hinton DR, Sadun AA, Blanks JC, Miller CA. Optic nerve degeneration in Alzheimer’s disease. N Eng J Med. 1986;315:485–7.
Feke GT, Hyman BT, Stern RA, Pasquale LR. Retinal blood flow in mild cognitive impairment and Alzheimer’s disease. Alzheimers Dement. 2015;1:144–51.
Bambo MP, Garcia-Martin E, Pinilla J, Herrero R, Satue M, Otin S, et al. Detection of retinal nerve fiber layer degeneration in patients with Alzheimer’s disease using optical coherence tomography: searching new biomarkers. Acta Ophthalmol. 2014;92:581–2.
Koronyo-Hamaoui M, Koronyo Y, Ljubimov AV, Miller CA, Ko MK, Black KL, et al. Identification of amyloid plaques in retinas from Alzheimer’s patients and noninvasive in vivo optical imaging of retinal plaques in a mouse model. Neuroimage. 2011;54:S204–17.
Schweitzer D, Hammer M, Schwietzer F, Schweitzer F, Jentsch S, Birckner E, et al. In vivo measurement of time-resolved autofluorescence at the human fundus. J Biomed Opt. 2004;9:1214–22.
Schweitzer D, Schenke S, Hammer M, Schweitzer F, Jentsch S, Birckner E, et al. Towards metabolic mapping of the human retina. Microsc Res Technol. 2007;70:410–9.
Dysli C, Quellec G, Abegg M, Menke MN, Wolf-Schnurrbusch U, Kowal J, et al. Quantitative analysis of fluorescence lifetime measurements of the macula using the fluorescence liftime imaging ophthalmoscope in healthy subjects. Invest Ophthalmol Vis Sci. 2014;55:2106–13.
Dysli C, Wolf S, Berezin MY, Sauer L, Hammer M, Zinkernagel MS. Fluorescence lifetime imaging ophthalmoscopy. Prog Retin Eye Res. 2017;60:120–43.
Schweitzer D, Deutsch L, Klemm M, Jentsch S, Hammer M, Peters S, et al. Fluorescence lifetime imaging ophthalmoscopy in type 2 diabetic patients who have no signs of diabetic retinopathy. J Biomed Opt. 2015;20:61106.
Jentsch S, Schweitzer D, Schmidtke KU, Peters S, Dawczynski J, Bär KJ, et al. Retinal fluorescence lifetime imaging ophthalmoscopy measures depend on the severity of Alzheimer’s disease. Acta Ophthalmol. 2015;93:e241–7.
Bulut M, Kurtuluş F, Gözkaya O, Erol MK, Cengiz A, Akıdan M, et al. Evaluation of optical coherence tomography angiographic findings in Alzheimer’s type dementia. Br J Ophthalmol. 2018;102:233–7.
McGrory S, Taylor AM, Kirin M, Corley J, Pattie A, Cox SR, et al. Retinal microvascular network geometry and cognitive abilities in community-dwelling older people: The Lothian Birth Cohort 1936 study. Br J Ophthalmol. 2017;101:993–8.
Golzan SM, Goozee K, Georgevsky D, Avolio A, Chatterjee P, Shen K, et al. Retinal vascular and structural changes are associated with amyloid burden in the elderly: ophthalmic biomarkers of preclinical Alzheimer’s disease. Alzheimers Res Ther. 2017;9:13.
Kim AY, Chu Z, Shahidzadeh A, Wang RK, Puliafito CA, Kashani AH. Quantifying microvascular density and morphology in diabetic retinopathy using spectral-domain optical coherence tomography angiography. Invest Ophthalmol Vis Sci. 2016;57:362–70.
Uji A, Balasubramanian S, Lei J, Baghdasaryan E, Al-Sheikh M, Sadda SR. Impact of multiple en face image averaging on quantitative assessment from optical coherence tomography angiography images. Ophthalmology. 2017;124:944–52.
Rabinovici GD, Rosen HJ, Alkalay A, Kornak J, Furst AJ, Agarwal N, et al. Amyloid vs FDG-PET in the differential diagnosis of AD and FTLD. Neurology. 2011;77:2034–42.
Delori FC, Dorey KC, Staurenghi G, Arend O, Goger DG, Weiter JJ. In vivo fluorescence of the ocular fundus exhibits retinal pigment epithelium lipofusin characteristics. Invest Ophthalmol Vis Sci. 1995;36:718–29.
Ishibashi T, Murata T, Hanagai M, Nagai R, Horiuchi S, Lopez PF, et al. Advanced glycation end products in age related macular degeneration. Arch Ophthalmol. 1998;116:1629–32.
Dysli C, Wolf S, Zinkernagel MS. autofluorescence lifetimes in geographic atrophy in patients with age-related macular degeneration. Invest Ophthalmol Vis Sci. 2016;57:2479–87.
Marziani E, Pomati S, Ramolfo P, Cigada M, Giani A, Mariani C, et al. Evaluation of retinal nerve fiber layer and ganglion cell layer thickness in Alzheimer’s disease using spectral-domain optical coherence tomography. Invest Ophthalmol Vis Sci. 2013;54:5953–8.
Lu Y, Li Z, Zhang X, Ming B, Jia J, Wang R, et al. Retinal nerve fiber layer structure abnormalities in early Alzheimer’s disease: evidence in optical coherence tomography. Neurosci Lett. 2010;480:69–72.
Acknowledgements
We thank Yoshihiko Katayama, PhD, and Ali Tafreshi, BS, from Heidelberg Engineering GmBH, Heidelberg, Germany for their valuable advices and providing technical assistance for the FLIO device.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SRS is a consultant for and receives research support from Optos and Carl Zeiss Meditec, and serves as a consultant for Centervue, and has access to research instruments provided by Heidelberg Engineering, Topcon Medical Systems, Optos, Carl Zeiss Meditec, Nidek, and Centervue. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The other authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sadda, S.R., Borrelli, E., Fan, W. et al. A pilot study of fluorescence lifetime imaging ophthalmoscopy in preclinical Alzheimer’s disease. Eye 33, 1271–1279 (2019). https://doi.org/10.1038/s41433-019-0406-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-019-0406-2
This article is cited by
-
Detection sensitivity of fluorescence lifetime imaging ophthalmoscopy for laser-induced selective damage of retinal pigment epithelium
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
Retina Oculomics in Neurodegenerative Disease
Annals of Biomedical Engineering (2023)
-
Photobiology of lipofuscin granules in the retinal pigment epithelium cells of the eye: norm, pathology, age
Biophysical Reviews (2022)
-
Plasma phosphorylated-tau181 levels reflect white matter microstructural changes across Alzheimer’s disease progression.
Metabolic Brain Disease (2022)