Abstract
Background
The etiology of aphakic glaucoma is unclear. It has been suggested that remaining lens epithelium releases cytokines transducing trabecular meshwork cells. Therefore, we compared two cohorts of children undergoing lensectomy. In cohort 1, the entire lens including its capsule was removed, in cohort 2 the peripheral lens capsule was left intact, also to facilitate secondary intraocular lens implantation later on.
Methods
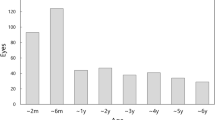
We included children with uni- or bilateral congenital cataract who underwent lensectomy during the first year of life with subsequent contact lenses fitting. Group 1 comprised 41 eyes, group 2 comprised 33 eyes. In group 1, the median age at surgery was 4.0 months in unilateral and 3.0 months in bilateral cases 1, in group 2, 8.1 months and 2.4 months, respectively. The mean follow-up was 12.8 years in group 1 and 9.3 years in group 2. All cases were analyzed for the prevalence of aphakic glaucoma, for visual acuity and for compliance in visual rehabilitation (contact lens/occlusion therapy).
Results
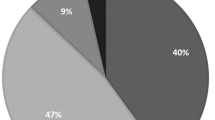
We found no significant difference in glaucoma prevalence between group 1 and group 2 (p = 0.68). The overall glaucoma rate was 26% after the mean follow-up of 11 years in both groups. In unilateral cases, the median visual acuity was logMAR 0.7 in both groups. In bilateral cases it was logMAR 0.4 in group 1 and logMAR 0.2 in group 2 (p = 0.05).
Conclusions
Leaving the peripheral lens capsule intact had no negative effect on the incidence of glaucoma and on resulting visual acuity.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Sheeladevi S, Lawrenson JG, Fielder AR, Suttle CM. Global prevalence of childhood cataract: a systematic review. Eye Lond Engl. 2016;30:1160–9.
Magnusson G, Haargaard B, Basit S, Lundvall A, Nyström A, Rosensvärd A. et al. The Paediatric Cataract Register (PECARE): an overview of operated childhood cataract in Sweden and Denmark. Acta Ophthalmol. (2017). https://doi.org/10.1111/aos.13497
Haargaard B, Ritz C, Oudin A, Wohlfahrt J, Thygesen J, Olsen T. et al. Risk of glaucoma after pediatric cataract surgery. Invest Ophthalmol Vis Sci. 2008;49:1791–6.
Alsheikheh A, Klink J, Klink T, Steffen H, Grehn F. Long-term results of surgery in childhood glaucoma. Graefes Arch Clin Exp Ophthalmol. 2007;245:195–203.
Lambert SR. The timing of surgery for congenital cataracts: Minimizing the risk of glaucoma following cataract surgery while optimizing the visual outcome. J AAPOS. 2016;20:191–2.
Michael I, Walton DS, Levenberg S. Infantile aphakic glaucoma: a proposed etiologic role of IL-4 and VEGF. J Aapos. 2011;48:98–107.
Witschel H. Pars plana lentectomy. Klin Mon Für Augenheilkd. 1987;190:406–11.
Gessner B, Wiese S, Lagreze WA. Results of pars plana lensectomy for childhood cataract. Ophthalmologe. 2004;101:901–6.
Trivedi RH, Wilson ME, Golub RL. Incidence and risk factors for glaucoma after pediatric cataract surgery with and without intraocular lens implantation. J Aapos. 2006;10:117–23.
Michaelides M, Bunce C, Adams GG. Glaucoma following congenital cataract surgery–the role of early surgery and posterior capsulotomy. BMC Ophthalmol. 2007;7:13.
Lawrence MG, Kramarevsky NY, Christiansen SP, Wright MM, Young TL, Summers CG. et al. Glaucoma following cataract surgery in children: surgically modifiable risk factors. Trans Am Ophthalmol Soc. 2005;103:46–55.
Freedman SF, Lynn MJ, Beck AD, Bothun ED, Örge FH, Lambert SR; Infant Aphakia Treatment Study Group. et al. Glaucoma-related adverse events in the first 5 years after unilateral cataract removal in the infant aphakia treatment study. JAMA Ophthalmol. 2015;133:907–14.
Mataftsi A, Haidich AB, Kokkali S, Rabiah PK, Birch E, Stager DR Jr. et al. Postoperative glaucoma following infantile cataract surgery: an individual patient data meta-analysis. JAMA Ophthalmol. 2014;132:1059–67.
Birch EE, Stager DR. The critical period for surgical treatment of dense congenital unilateral cataract. Invest Ophthalmol Vis Sci. 1996;37:1532–8.
Hartmann EE, Lynn MJ, Lambert SR. Baseline characteristics of the infant aphakia treatment study population: predicting recognition acuity at 4.5 years of age. Invest Ophthalmol Vis Sci. 2015;56:388–95.
Birch EE, Cheng C, Stager DR, Weakley DR, Stager DR. The critical period for surgical treatment of dense congenital bilateral cataracts. J AAPOS. 2009;13:67–71.
Lambert SR, Lynn MJ, Reeves R, Plager DA, Buckley EG, Wilson ME. et al. Is there a latent period for the surgical treatment of children with dense bilateral congenital cataracts? J AAPOS. 2006;10:30–36.
Chen D, Gong XH, Xie H, Zhu XN, Li J, Zhao YE. et al. The long-term anterior segment configuration after pediatric cataract surgery and the association with secondary glaucoma. Sci Rep. 2017;7:43015.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stech, M., Grundel, B., Daniel, M. et al. Risk of aphakic glaucoma after pars plana-lensectomy with and without removal of the peripheral lens capsule. Eye 33, 1472–1477 (2019). https://doi.org/10.1038/s41433-019-0435-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-019-0435-x
This article is cited by
-
Katarakt im Kindesalter
Monatsschrift Kinderheilkunde (2025)
-
Glaukom im Säuglings- und Kindesalter
Spektrum der Augenheilkunde (2025)
-
Katarakt im Kindesalter – Teil 2
Die Ophthalmologie (2025)
-
Katarakt im Kindesalter – Teil 1
Die Ophthalmologie (2025)
-
Development of a prognostic model for predicting long-term visual acuity after cataract surgery in children with bilateral congenital cataracts: a single centre retrospective, observational study
BMC Ophthalmology (2024)