Abstract
Aims
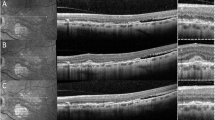
To assess hyperreflective foci (HF) number in angioid streaks (AS) by means of spectral-domain optical coherence tomography (SD-OCT).
Methods
Observational and cross-sectional study. Sixty-two eyes with AS and 62 controls underwent best-corrected visual acuity (BCVA), fundoscopy, and SD-OCT. HF were assessed on the horizontal scan of a six-line radial OCT, in the fovea (1500-μm diameter) and parafovea (500 μm external to the fovea), and sub-classified as retinal or choroidal, small or large. Eyes were distributed in one of four groups, as carrying foveal AS without choroidal neovascularization (CNV) (14 eyes), extra-foveal AS without CNV (14), active CNV (20), and inactive CNV (14). Primary outcome was HF assessment in AS. Secondary outcomes included their correlations with BCVA.
Results
AS-affected eyes had higher HF numbers. Our sub-analysis revealed that patients with active CNV had a larger number of retinal and choroidal HF than all the other groups, whereas retinal and choroidal foci were significantly increased in inactive CNV only with respect to controls. Interestingly, patients with foveal AS showed HF number increase in the choroid and fovea. BCVA deterioration positively correlated with the total HF number found in the fovea and the choroid.
Conclusion
HF are significantly increased in patients with AS. Despite being especially evident in active CNV, the increasing number in eyes without CNV might suggest new pathogenetic aspects of the disease.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Doyne RW. Choroidal and retinal changes. The result of blows on the eyes. Trans Ophthalmol Sok UK. 1889;9:128.
Gliem M, De Zaeytijd J, Finger RP, et al. An update on the clinical phenotype in patients with pseudoxanthoma elasticum. Front Genet. 2013;4:14.
Aessopos A, Voskaridou E, Kavouklis E, et al. Angioid streaks in sickle-thalassemia. Am J Ophthalmol. 1994;117:589–92.
Dabbs TR, Skjodt K. Prevalence of angioid streaks and other ocular complications of Paget’s disease of bone. Br J Ophthalmol. 1990;74:579–82.
Gurwood AS, Mastrangelo DL. Understanding angioid streaks. J Am Optom Assoc. 1997;68:309–24.
Lim JI, Bressler NM, Marsh MJ, Bressler SB. Laser treatment of choroidal neovascularization in patients with angioid streaks. Am J Ophthalmol. 1993;116:414–23.
Battaglia Parodi M, Iacono P, La Spina C, et al. Intravitreal bevacizumab for nonsubfoveal choroidal neovascularization associated with angioid streaks. Am J Ophthalmol 2014;157:374–7.e2.
Clarkson JG, Altman RD. Angioid streaks. Surv Ophthalmol 1982;26:235–46.
Bolz M, Schmidt-Erfurth U, Deak G, Diabetic Retinopathy Research Group Vienna. et al. Optical coherence tomographic hyper-reflective foci: a morphological sign of lipid extravasation in diabetic macular edema. Ophthalmology. 2009;116:914–20.
Christenbury JG, Folgar FF, O’Connell R, et al. Progression of intermediate age-related macular degeneration with proliferation and inner retinal migration of hyperreflective foci. Ophthalmology. 2013;120:1038–45.
Coscas G, De Benedetto U, Coscas F, et al. Hyperreflective dots: a new spectral-domain optical coherence tomography entity for follow-up and prognosis in exudative age-related macular degeneration. Ophthalmologica. 2013;229:32–7.
Kuroda M, Hirami Y, Hata M, et al. Intraretinal hyperreflective foci on spectral-domain optical coherence tomography images of patients with retinitis pigmentosa. Clin Ophthalmol. 2014;8:435–40.
Piri N, Nesmith BLW, Schaal S. Choroidal hyperreflective foci in Stargardt disease shown by spectral-domain optical coherence tomography imaging. Correlation with disease severity. JAMA Ophthalmol. 2015;133:398–405.
De Benedetto U, Sacconi R, Pierro L, et al. Optical coherence tomographic hyperreflective foci in early stages of diabetic retinopathy. Retina. 2015;35:449–53.
Battaglia Parodi M, Iacono P, Romano F, et al. Optical coherence tomography in best vitelliform macular dystrophy. Eur J Ophthalmol 2017;27:201–4.
Parodi MB, Romano F, Sacconi R, et al. Intraretinal hyperreflective foci in best vitelliform macular dystrophy. Retina. 2018;38:2379–86. https://doi.org/10.1097/IAE.0000000000001893.
Battaglia PM, Sacconi R, Romano F, Bandello F. Hyperreflective foci in Stargardt disease: 1-year follow-up. Graefes Arch Clin Exp Ophthalmol. 2018. https://doi.org/10.1007/s00417-018-4167-6. [e-pub ahead of print].
Charbel Issa P, Finger RP, Holz FG, Scholl HP. Multimodal imaging including spectral domain OCT and confocal near infrared reflectance for characterization of outer retinal pathology in pseudoxanthoma elasticum. Invest Ophthalmol Vis Sci. 2009;50:5913–84.
Ellabban AA, Tsujikawa A, Matsumoto A, et al. Macular choroidal thickness and volume in eyes with angioid streaks measured by swept source optical coherence tomography. Am J Ophthalmol. 2012;153:1133–43.
Lee H, Lee J, Chung H, Kim HC. Baseline spectral domain optical coherence tomographic hyperreflective foci as a predictor of visual outcome and recurrence for central serous chorioretinopathy. Retina 2016;36:1372–80.
Dreyer R, Green WR. The pathology of angioid streaks: a study of twenty-one cases. Trans Pa Acad Ophthalmol Otolaryngol. 1978;31:158–67.
Jensen OA. Bruch’s membrane in pseudoxanthoma elasticum. Histochemical, ultrastructural, and x-ray microanalytical study of the membrane and angioid streak areas. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1977;203:311–20.
Scholz R. Angioid streaks. Arch Ophthalmol. 1941;26:677–95.
Hagedoorn A. Angioid streaks and traumatic ruptures of Bruch’s membrane. Br J Ophthalmol. 1975;59:267.
Gliem M, Finger RP, Fimmers R, et al. Treatment of choroidal neovascularization due to angioid streaks: a comprehensive review. Retina. 2013;33:1300–14.
Abri Aghdam K, Pielen A, Framme C, Junker B. Correlation between hyperreflective foci and clinical outcomes in neovascular age-related macular degeneration after switching to aflibercept. Invest Ophthalmol Vis Sci. 2015;56:6448–55. https://doi.org/10.1167/iovs.15-17338.
Parodi MB, Arrigo A, Romano F, et al. Hyperreflective foci number correlates with choroidal neovascularization activity in angioid streaks. Invest Ophthalmol Vis Sci. 2018;59:3314–9. https://doi.org/10.1167/iovs.18-24291.
Schreur V, Altay L, van Asten F, et al. Hyperreflective foci on optical coherence tomography associate with treatment outcome for anti-VEGF in patients with diabetic macular edema. PLoS One 2018;13:e0206482. https://doi.org/10.1371/journal.pone.0206482.
Chen KC, Jung JJ, Curcio CA, et al. Intraretinal hyperreflective foci in acquired vitelliform lesions of the macula: clinical and histologic study. Am J Ophthalmol. 2016;164:89–98.
Turgut B, Yildirim H. The causes of hyperreflective dots in optical coherence tomography excluding diabetic macular edema and retinal venous occlusion. Open Ophthalmol J. 2015;9:36–40.
Grisanti S, Guidry C. Transdifferentiation of retinal pigment epithelial cells from epithelial to mesenchymal phenotype. Invest Ophthalmol Vis Sci. 1995;36:391–405.
Kim JW, Kang KH, Burrola P, et al. Retinal degeneration triggered by inactivation of PTEN in the retinal pigment epithelium. Genes Dev. 2008;22:3147–57.
Zanzottera EC, Messinger JD, Ach T, Smith RT, Freund KB, Curcio CA. The project MACULA retinal pigment epithelium grading system for histology and optical coherence tomography in age-related macular degeneration. Invest Ophthalmol Vis Sci. 2015;56:3253–68.
Killingsworth MC, Sarks JP, Sarks SH. Macrophages related to Bruch’s membrane in age-related macular degeneration. Eye (Lond). 1990;4:613–21.
Hu X, Plomp AS, van Soest S, Wijnholds J, de Jong PT, Bergen AA. Pseudoxanthoma elasticum: a clinical, histopathological, and molecular update. Surv Ophthalmol. 2003;48:424–38.
Cherepanoff S, McMenamin P, Gillies MC, Kettle E, Sarks SH. Bruch’s membrane and choroidal macrophages in early and advanced age-related macular degeneration. Br J Ophthalmol. 2010;94:918–25.
Chan CY, Papakostas TD, Vavvas DG. Choroidal changes associated with Bruch membrane pathology in pseudoxanthoma elasticum. Am J Ophthalmol. 2014;158:644–9.
Gliem M, Fimmers R, Müller PL, et al. Choroidal changes associated with Bruch membrane pathology in pseudoxanthoma elasticum. Am J Ophthalmol. 2014;158:198–207.
Marchese A, Parravano M, Rabiolo A, Carnevali A, Corbelli E, Cicinelli MV, et al. Optical coherence tomography analysis of evolution of Bruch’s membrane features in angioid streaks. Eye (Lond). 2017. https://doi.org/10.1038/eye.2017.112.
Grisanti S, Guidry C. Transdifferentiation of retinal pigment epithelial cells from epithelial to mesenchymal phenotype. Invest Ophthalmol Vis Sci. 1995;36:391–405.
Kim JW, Kang KH, Burrola P, et al. Retinal degeneration triggered by inactivation of PTEN in the retinal pigment epithelium. Genes Dev. 2008;22:3147–57.
Sennlaub F, Auvynet C, Calippe B, et al. CCR2(+) monocytes infiltrate atrophic lesions in age-related macular disease and mediate photoreceptor degeneration in experimental subretinal inflammation in Cx3cr1 deficient mice. EMBO Mol Med. 2013;5:1775–93.
Abri Aghdam K, Pielen A, Framme C, Junker B. Correlation between hyperreflective foci and clinical outcomes in neovascular age-related macular degeneration after switching to aflibercept. Invest Ophthalmol Vis Sci. 2015;56:6448–55.
Murdoch IE, Morris SS, Cousens SN. People and eyes: statistical approaches in ophthalmology. Br J Ophthalmol. 1998;82:971–3.
Acknowledgements
MBP has the following disclosures: Bausch & Lomb Inc (C). FB has the following disclosures: Alcon (C), Allergan Plc.(C), Famila-Thea (C), Bayer Schering Pharma AG (C), Bausch & Lomb (C), Hoffmann-La-Roche (C), Novartis (C), Sanofi-Aventis (C), and Carl Zeiss AG (C). FR, SM, AA, AM, MVC, and GCA have no financial disclosures.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Romano, F., Mercuri, S., Arrigo, A. et al. Identification of hyperreflective foci in angioid streaks. Eye 33, 1916–1923 (2019). https://doi.org/10.1038/s41433-019-0483-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-019-0483-2
This article is cited by
-
Inner retinal hyper-reflective foci number correlates with flood-illumination adaptive optics ophthalmoscopy grading and systemic organ involvement in patients with Fabry disease
Eye (2025)
-
The identification of activity of choroidal neovascularization complicating angioid streaks
Eye (2022)
-
Choroidal Modifications Preceding the Onset of Macular Neovascularization in Age-Related Macular Degeneration
Ophthalmology and Therapy (2022)