Abstract
Objective
To estimate the incidence of acute cerebral ischaemia detected by magnetic resonance imaging (MRI) in acute central retinal artery occlusion (CRAO), branch retinal artery occlusion (BRAO) and transient monocular vision loss (TMVL).
Methods
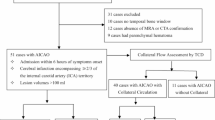
Studies reporting the incidence of acute cerebral ischaemia, detected by MRI, within 7 days from diagnosis of acute CRAO, BRAO and TMVL up to January 2019 were systematically searched for on Pubmed, Medline and Cochrane Library. Meta-analysis was performed using random effects model. The primary outcome was the pooled estimate of incidence of acute cerebral ischaemia in CRAO, BRAO and TMVL cohorts including both neurologically symptomatic and asymptomatic patients, expressed as a proportion along with 95% confidence intervals (CIs). The pooled estimate of incidence of asymptomatic acute cerebral ischaemia represented a secondary outcome measure.
Results
For the primary outcome, the pooled proportion of acute cerebral ischaemia was 0.30 (CI 0.24–0.36) in the CRAO cohort, and 0.25 (CI 0.16–0.37) in the BRAO cohort, without statistical heterogeneity. The rate of acute cerebral ischaemia was 11.8% in the TMVL cohort. For the secondary outcome, the pooled proportion of asymptomatic acute cerebral ischaemia was 0.22 (CI 0.16–0.28) in the CRAO cohort, 0.29 (CI 0.20–0.41) in the BRAO cohort and 0.08 (CI 0.05–0.15) in the TMVL cohort, with no statistical heterogeneity.
Conclusions
30% of patients with acute CRAO and 25% of patients with acute BRAO presented an acute cerebral ischaemia on MRI. Such high rates support a care pathway of prompt referral of such patients for neurological evaluation and brain imaging.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Hayreh SS. Acute retinal arterial occlusive disorders. Prog Retin Eye Res. 2011;30:359–394.
Easton JD, Saver JL, Albers GW, Alberts MJ, Chaturvedi S, Feldmann E, et al. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American academy of neurology affirms the value of this statement as an educational tool for neurologists. Stroke. 2009;40:2276–2293.
Park SJ, Choi NK, Yang BR, Park KH, Lee J, Jung SY, et al. Risk and Risk Periods for Stroke and Acute Myocardial Infarction in Patients with Central Retinal Artery Occlusion. Ophthalmology. 2015;122:2336–2343.
Hayreh SS. Do patients with retinal artery occlusion need urgent neurolgical evaluation? Am J Ophthalmol. 2018. https://doi.org/10.1016/j.ajo.2018.08.015
Arnold AC. Urgent evaluation of the patient with acute central retinal artery occlusion. Am J Ophthalmol. 2018;196:xvi–xvii.
Lavin P, Patrylo M, Hollar M, Espaillat KB, Kirshner H, Schrag M. Stroke risk and risk factors in patients with central retinal artery occlusion. Am J Ophthalmol. 2018. https://doi.org/10.1016/j.ajo.2018.08.027
Helenius J, Arsava EM, Goldstein JN, Cestari DM, Buonanno FS, Rosen BR, et al. Concurrent acute brain infarcts in patients with monocular visual loss. Ann Neurol. 2012;72:286–293.
Lee J, Kim SW, Lee SC, Kwon OW, Kim YD, Byeon SH. Co-occurrence of acute retinal artery occlusion and acute ischemic stroke: diffusion weighted magnetic resonance imaging study. Am J Ophthalmol. 2014;157:1231e1238.
Lauda F, Neugebauer H, Reiber L, Jüttler E. Acute silent brain infarction in monocular visual loss of ischemic origin. Cerebrovasc Dis. 2015;40:151e156.
Golsari A, Bittersohl D, Cheng B, Griem P, Beck C, Hassenstein A, et al. Silent brain infarctions and leukoaraiosis in patients with retinal ischemia: a prospective single-center observational study. Stroke. 2017;48:1392–1396.
Zhang LY, Zhang J, Kim RK, Matthews JL, Rudich DS, Greer DM, et al. Risk of acute ischemic stroke in patients with monocular vision loss of vascular etiology. J Neuroophthalmol. 2018;38:328–333.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012.
Davis DP, Robertson T, Imbesi SG. Diffusion-weighted magnetic resonance imaging versus computed tomography in the diagnosis of acute ischemic stroke. J Emerg Med. 2006;31:269–77. Review
Copen WA, Schwamm LH, Gonzàlez RG, Wu O, Harmath CB, Schaefer PW, et al. Ischemic stroke: effects of etiology and patient age on the time course of the core apparent diffusion coefficient. Radiology. 2001;221:27–34.
Burdette JH, Ricci PE, Petitti N, Elster AD. Cerebral infarction: time course of signal intensity changes on diffusion-weighted MR images. Am J Roentgenol. 1998;171:791–5.
Fiebach JB, Schellinger PD, Jansen O, Meyer M, Wilde P, Bender J, et al. CT and diffusion weighted MR imaging in randomized order: diffusionweighted imaging results in higher accuracy and lower interrater variability in the diagnosis of hyperacute ischemic stroke. Stroke. 2002;33:2206–2210.
Gonzalez RG, Schaefer PW, Buonanno FS, Schwamm LH, Budzik RF, Rordorf G, et al. Diffusion weighted MR imaging: diagnostic accuracy in patients imaged within 6 h of stroke symptom onset. Radiology. 1999;210:155–162.
Vermeer SE, Longstreth WT Jr, Koudstaal PJ. Silent brain infarcts: a systematic review. Lancet Neurol. 2007;6:611–9.
Stang A. Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605.
Fallico M, Russo A, Longo A, Pulvirenti A, Avitabile T, Bonfiglio V, et al. Internal limiting membrane peeling versus no peeling during primary vitrectomy for rhegmatogenous retinal detachment: a systematic review and meta-analysis. PLoS ONE. 2018;13:e0201010.
Hayreh SS, Zimmerman MB. Ocular arterial occlusive disorders and carotid artery disease. Ophthalmol Retin. 2017;1:12–18.
Biousse V, Nahab F, Newman NJ. Management of acute retinal ischemia: follow the guidelines! Ophthalmology. 2018;125:1597–1607.
Atkins E, Bruce BB, Newman NJ, Biousse V. Translation of clinical studies to clinical practice: survey on the treatment of central retinal artery occlusion. Am J Ophthalmol. 2009;148:172e173.
Youn TS, Lavin P, Patrylo M, Schindler J, Kirshner H, Greer DM, Schrag M. Current treatment of central retinal artery occlusion: a national survey. J Neurol. 2018;265:330–335.
Abel AS, Suresh S, Hussein HM, Carpenter AF, Montezuma SR, Lee MS. Practice patterns after acute embolic retinal artery occlusion. Asia Pac J Ophthalmol. 2017;6:37e39.
Zhou Y, Zhu W, Wang C. Relationship between retinal vascular occlusions and incident cerebrovascular diseases: A systematic review and meta-analysis. Medicine. 2016;95:e4075.
French DD, Margo CE, Greenberg PB. Ischemic stroke risk in medicare beneficiaries with central retinal artery occlusion: a retrospective cohort study. Ophthalmol Ther. 2018;7:125–131.
Goldstein LB. Accuracy of ICD-9-CM coding for the identification of patients with acute ischemic stroke. Effect of modifier codes. Stroke. 1998;29:1602–4.
Rothwell PM, Giles MF, Chandratheva A, Marquardt L, Geraghty O, Redgrave JN, et al. Early use of Existing Preventive Strategies for Stroke (EXPRESS) study. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet. 2007;370:1432e1442.
Lavallée PC, Meseguer E, Abboud H, Cabrejo L, Olivot JM, Simon O, et al. A transient ischaemic attack clinic with round-the-clock access (SOSTIA): feasibility and effects. Lancet Neurol. 2007;6:953e960.
Mukundan G, Seidenwurm DJ. Economic and Societal Aspects of Stroke Management. Neuroimaging Clin N Am. 2018;28:683–689.
Acknowledgements
We are grateful to Dott. A. Bridgewood of the Scientific Bureau of the University of Catania for language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Fallico, M., Lotery, A.J., Longo, A. et al. Risk of acute stroke in patients with retinal artery occlusion: a systematic review and meta-analysis. Eye 34, 683–689 (2020). https://doi.org/10.1038/s41433-019-0576-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-019-0576-y
This article is cited by
-
Retinal ischemia due to different stages of atherosclerosis - insights from a retrospective study on central retinal artery occlusion
Neurological Research and Practice (2025)
-
Incidence and risk factors associated with ischemic cerebrovascular disease in patients with retinal artery occlusion: a systematic review and meta-analysis
Scientific Reports (2025)
-
Comparison of vascular risk profile and clinical outcomes among patients with central (branch) retinal artery occlusion versus amaurosis fugax
Neurological Research and Practice (2024)
-
Plasmalogens and Octanoylcarnitine Serve as Early Warnings for Central Retinal Artery Occlusion
Molecular Neurobiology (2024)
-
Statin Treatment on Cardiovascular Risk After Retinal Artery Occlusion: A Historical Cohort Study
Journal of Epidemiology and Global Health (2023)