Abstract
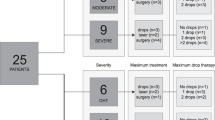
Presentation with advanced glaucoma is a significant risk factor for lifetime blindness. The asymptomatic nature of glaucoma, particularly in early disease, means that substantial vision loss in one eye does not always translate into a perceptible loss of visual function. This, along with the lack of an effective screening strategy, contributes to late presentation. Those most at risk of presenting with advanced glaucoma have asymptomatic high intraocular pressure (IOP), no family history of glaucoma, are socially disadvantaged, and do not attend sight testing. Patients with glaucoma may have impaired functionality for daily activities, such as reading, walking and driving. Quality of life measures have shown this to be significantly worse in patients with more severe visual field loss, particularly if bilateral. In addition, quality of life decreases faster with further bilateral visual field loss when advanced visual field damage is present. Management of these patients requires disproportionally more resources than those with earlier disease. Both medical and surgical options are used as the initial approach to treat patients presenting with advanced glaucoma. The most recently published National Institute for Health and Care Excellence (NICE) guidelines suggest that patients presenting with advanced disease should be offered trabeculectomy as a primary intervention. However, more evidence is required to determine the best initial management. The Treatment of Advanced Glaucoma Study (TAGS) is being conducted, comparing primary medical management with primary mitomycin C-augmented trabeculectomy for people presenting with advanced open-angle glaucoma. The results of TAGS will provide robust evidence for the most appropriate initial intervention.
摘要
晚期青光眼为不可逆致盲性眼病。青光眼发病隐匿, 特别是早期阶段, 而随后会出现单眼视力损害通常不会引起可察觉的视功能丧失。由于对无症状青光眼缺乏有效的筛查手段, 此类疾病容易进展到晚期阶段。无青光眼家族史、较低的社会地位、未进行视力筛查同时伴有高眼压的无症状青光眼是发展为晚期青光眼的高危人群。青光眼的视功能受损会影响患者日常生活, 比如阅读, 走路, 驾驶。生活质量评估显示严重的视力损害尤其是病变累及双眼时, 会极大影响患者的生活质量。此外, 随着青光眼患者发展为严重的视野缺损, 出现双侧视野缺损, 生活质量会迅速下降。无症状的晚期青光眼患者的管理比早期患者需要更多资源。药物及手术治疗均为晚期青光眼治疗的首选方法。国家健康和保健卓越研究所 (NICE) 最新指南建议, 晚期青光眼患者首选小梁切除术, NICE在近期发布的指南中提出, 晚期青光眼患者应首先进行小梁切除术, 但对于首选的治疗方式尚缺乏循证证据。目前, 正在进行的晚期青光眼治疗研究 (TAGS), 通过对比传统的治疗方式与小梁切除术联合丝裂霉素C治疗晚期开角型青光眼的疗效, 为晚期青光眼的最佳治疗提供有力证据。
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
National Institute for Health and Care Excellence. Glaucoma diagnosis and management NICE guideline [NG81]. 2017. https://www.nice.org.uk/guidance/ng81. Accessed 01/06/2019.
Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90:262–7.
Minassian DC, Reidy A, Coffey M, Minassian A. Utility of predictive equations for estimating the prevalence and incidence of primary open angle glaucoma in the UK. Br J Ophthalmol. 2000;84:1159–61.
Burr JM, Mowatt G, Hernandez R, Siddiqui MA, Cook J, Lourenco T, et al. The clinical effectiveness and cost-effectiveness of screening for open angle glaucoma: a systematic review and economic evaluation. Health Technol Assess. 2007;11:1–190. p.iii-iv, ix-x
Spry PG, Spencer IC, Sparrow JM, Peters TJ, Brookes ST, Gray S, et al. The Bristol Shared Care Glaucoma Study: reliability of community optometric and hospital eye service test measures. Br J Ophthalmol. 1999;83:707–12.
Harrison RJ, Wild JM, Hobley AJ. Referral patterns to an ophthalmic outpatient clinic by general practitioners and ophthalmic opticians and the role of these professionals in screening for ocular disease. BMJ. 1988;297:1162–7.
Morley AM, Murdoch I. The future of glaucoma clinics. Br J Ophthalmol. 2006;90:640–5.
Lee PP, Walt JG, Doyle JJ, Kotak SV, Evans SJ, Budenz DL, et al. A multicenter, retrospective pilot study of resource use and costs associated with severity of disease in glaucoma. Arch Ophthalmol. 2006;124:12–9.
The European Glaucoma Society. Terminology and Guidelines for Glaucoma, 4th Edition - Part 1 Supported by the EGS Foundation. Br J Ophthalmol. 2017;101:1–72.
The World Health Organization. International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM).
Parekh AS, Tafreshi A, Dorairaj SK, Weinreb RN. Clinical applicability of the International Classification of Disease and Related Health Problems (ICD-9) glaucoma staging codes to predict disease severity in patients with open-angle glaucoma. J Glaucoma. 2014;23:e18–22.
Ng M, Sample PA, Pascual JP, Zangwill LM, Girkin CA, Liebmann JM, et al. Comparison of visual field severity classification systems for glaucoma. J Glaucoma. 2012;21:551–61.
Brusini P, Johnson CA. Staging functional damage in glaucoma: review of different classification methods. Surv Ophthalmol. 2007;52:156–79.
de Moraes CG, Liebmann JM, Medeiros FA, Weinreb RN. Management of advanced glaucoma: Characterization and monitoring. Surv Ophthalmol. 2016;61:597–615.
Hodapp E, Parrish RK, Anderson DR. Clinical decisions in glaucoma. 1993, St Louis C.V.: Mosby.
Ng WS, Agarwal PK, Sidiki S, McKay L, Townend J, Azuara-Blanco A. The effect of socio-economic deprivation on severity of glaucoma at presentation. Br J Ophthalmol. 2010;94:85–7.
Boodhna T, Crabb DP. Disease severity in newly diagnosed glaucoma patients with visual field loss: trends from more than a decade of data. Ophthalmic Physiol Opt. 2015;35:225–30.
Inuzuka H, Sawada A, Yamamoto T. Comparison of changes in macular ganglion cell - inner plexiform layer thickness between medically and surgically treated eyes with advanced glaucoma. Am J Ophthalmol. 2018;187:43–50.
Tsagkataki M, Bampouras TM, Choudhary A. Outcomes of viscocanalostomy and phaco-viscocanalostomy in patients with advanced glaucoma. Graefes Arch Clin Exp Ophthalmol. 2018;256:1481–7.
Peters D, Bengtsson B, Heijl A. Factors associated with lifetime risk of open-angle glaucoma blindness. Acta Ophthalmol. 2014;92:421–5.
King AJ, Fernie G, Azuara-Blanco A, Burr JM, Garway-Heath T, Sparrow JM, et al. Treatment of Advanced Glaucoma Study: A multicentre randomised controlled trial comparing primary medical treatment with primary trabeculectomy for people with newly diagnosed advanced glaucoma - Study protocol. British Journal of Ophthalmology. 2018;102:922–8.
Heijl A, Bengtsson B, Oskarsdottir SE. Prevalence and severity of undetected manifest glaucoma: results from the early manifest glaucoma trial screening. Ophthalmology. 2013;120:1541–5.
Gillespie BW, Musch DC, Guire KE, Mills RP, Lichter PR, Janz NK, et al. The collaborative initial glaucoma treatment study: baseline visual field and test-retest variability. Invest Ophthalmol Vis Sci. 2003;44:2613–20.
Song W, Shan L, Cheng F, Fan P, Zhang L, Qu W, et al. Prevalence of glaucoma in a rural northern china adult population: a population-based survey in Kailu County, inner Mongolia. Ophthalmology. 2011;118:1982–8.
Dandona L, Dandona R, Srinivas M, Mandal P, John RK, McCarty CA, et al. Open-angle glaucoma in an urban population in southern India: the Andhra Pradesh eye disease study. Ophthalmology. 2000;107:1702–9.
Coffey M, Reidy A, Wormald R, Xian WX, Wright L, Courtney P. Prevalence of glaucoma in the west of Ireland. Br J Ophthalmol. 1993;77:17–21.
Sheldrick JH, Ng C, Austin DJ, Rosenthal AR. An analysis of referral routes and diagnostic accuracy in cases of suspected glaucoma. Ophthalmic Epidemiol. 1994;1:31–9.
Sukumar S, Spencer F, Fenerty C, Harper R, Henson D. The influence of socioeconomic and clinical factors upon the presenting visual field status of patients with glaucoma. Eye (Lond). 2009;23:1038–44.
Elkington AR, MacKean JPS. A collaborative hospital glaucoma survey. Res Clin Forums. 1982;4:31–40.
The UK National Screening Committee. The UK NSC recommendation on Glaucoma screening in adults. Available at https://legacyscreening.phe.org.uk/glaucoma. 2016.
Prior M, Francis JJ, Azuara-Blanco A, Anand N, Burr JM. Glaucoma Screening Platform Study Group. Why do people present late with advanced glaucoma? A qualitative interview study. Br J Ophthalmol. 2013;97:1574–8.
Fraser S, Bunce C, Wormald R. Risk factors for late presentation in chronic glaucoma. Invest Ophthalmol Vis Sci. 1999;40:2251–7.
Fraser S, Bunce C, Wormald R, Brunner E. Deprivation and late presentation of glaucoma: case-control study. BMJ. 2001;322:639–43.
Shickle D, Griffin M. Why don't older adults in England go to have their eyes examined? Ophthalmic Physiol Opt. 2014;34:38–45.
Leamon S, Hayden C, Lee H, Trudinger D, Appelbee E, Hurrell DL, et al. Improving access to optometry services for people at risk of preventable sight loss: a qualitative study in five UK locations. J Public Health (Oxf). 2014;36:667–73.
McLaughlan BEA. Understanding of the purpose of an eye test among people aged 60 and over in the UK. Optometry Pract. 2010;11:179–88.
Awobem JF, Cassels-Brown A, Buchan JC, Hughes KA. Exploring glaucoma awareness and the utilization of primary eye care services: community perceived barriers among elderly African Caribbeans in Chapeltown, Leeds. Eye (Lond). 2009;23:243. author reply 243.
Cross V, Shah P, Bativala R, Spurgeon P. ReGAE 2: glaucoma awareness and the primary eye-care service: some perceptions among African Caribbeans in Birmingham UK. Eye (Lond). 2007;21:912–20.
Patel DBH, Murdoch I. Barriers to uptake of eye care services by the Indian population living in Ealing, West London. Health Educ J. 2006;65:267–76.
Shickle D, Farragher TM. Geographical inequalities in uptake of NHS-funded eye examinations: small area analysis of Leeds, UK. J Public Health (Oxf). 2015;37:337–45.
Burr J, Hernandez R, Ramsay C, Prior M, Campbell S, Azuara-Blanco A, et al. Is it worthwhile to conduct a randomized controlled trial of glaucoma screening in the United Kingdom? J Health Serv Res Policy. 2014;19:42–51.
Sommer A, Tielsch JM, Katz J, Quigley HA, Gottsch JD, Javitt JC, et al. Racial differences in the cause-specific prevalence of blindness in east Baltimore. N Engl J Med. 1991;325:1412–7.
Kulkarni BB, Leighton P, King AJ. Exploring patients’ expectations and preferences of glaucoma surgery outcomes to facilitate healthcare delivery and inform future glaucoma research. British Journal of Ophthalmology. Published Online First: April 2019. https://doi.org/10.1136/bjophthalmol-2018-313401.
Braithwaite T, Calvert M, Gray A, Pesudovs K, Denniston AK. The use of patient-reported outcome research in modern ophthalmology: impact on clinical trials and routine clinical practice. Patient Relat Outcome Meas. 2019;10:9–24.
Sotimehin AE, Ramulu PY. Measuring Disability in Glaucoma. J Glaucoma. 2018;27:939–49.
Tomomitsu MS, Alonso AC, Morimoto E, Bobbio TG, Greve JM. Static and dynamic postural control in low-vision and normal-vision adults. Clinics (Sao Paulo). 2013;68:517–21.
Shabana N, Cornilleau-Peres V, Droulez J, Goh JC, Lee GS, Chew PT. Postural stability in primary open angle glaucoma. Clin Exp Ophthalmol. 2005;33:264–73.
Kotecha A, Richardson G, Chopra R, Fahy RT, Garway-Heath DF, Rubin GS. Balance control in glaucoma. Invest Ophthalmol Vis Sci. 2012;53:7795–801.
de Luna RA, Mihailovic A, Nguyen AM, Friedman DS, Gitlin LN, Ramulu PY. The Association of Glaucomatous Visual Field Loss and Balance. Transl Vis Sci Technol. 2017;6:8.
Black AA, Wood JM, Lovie-Kitchin JE, Newman BM. Visual impairment and postural sway among older adults with glaucoma. Optom Vis Sci. 2008;85:489–97.
Diniz-Filho A, Boer ER, Gracitelli CP, Abe RY, van Driel N, Yang Z, et al. Evaluation of Postural Control in Patients with Glaucoma Using a Virtual Reality Environment. Ophthalmology. 2015;122:1131–8.
Friedman DS, Freeman E, Munoz B, Jampel HD, West SK. Glaucoma and mobility performance: the Salisbury Eye Evaluation Project. Ophthalmology. 2007;114:2232–7.
Mihailovic A, Swenor BK, Friedman DS, West SK, Gitlin LN, Ramulu PY. Gait Implications of Visual Field Damage from Glaucoma. Transl Vis Sci Technol. 2017;6:23.
Turano KA, Rubin GS, Quigley HA. Mobility performance in glaucoma. Invest Ophthalmol Vis Sci. 1999;40:2803–9.
Ramrattan RS, Wolfs RC, Panda-Jonas S, Jonas JB, Bakker D, Pols HA, et al. Prevalence and causes of visual field loss in the elderly and associations with impairment in daily functioning: the Rotterdam Study. Arch Ophthalmol. 2001;119:1788–94.
Hong T, Mitchell P, Burlutsky G, Samarawickrama C, Wang JJ. Visual impairment and the incidence of falls and fractures among older people: longitudinal findings from the Blue Mountains Eye Study. Invest Ophthalmol Vis Sci. 2014;55:7589–93.
Freeman EE, Munoz B, Rubin G, West SK. Visual field loss increases the risk of falls in older adults: the Salisbury eye evaluation. Invest Ophthalmol Vis Sci. 2007;48:4445–50.
Patino CM, McKean-Cowdin R, Azen SP, Allison JC, Choudhury F, Varma R, et al. Central and peripheral visual impairment and the risk of falls and falls with injury. Ophthalmology. 2010;117:199–206 e1.
Coleman AL, Cummings SR, Ensrud KE, Yu F, Gutierrez P, Stone KL, et al. Visual field loss and risk of fractures in older women. J Am Geriatr Soc. 2009;57:1825–32.
Lamoureux EL, Chong E, Wang JJ, Saw SM, Aung T, Mitchell P, et al. Visual impairment, causes of vision loss, and falls: the singapore malay eye study. Invest Ophthalmol Vis Sci. 2008;49:528–33.
Klein BE, Moss SE, Klein R, Lee KE, Cruickshanks KJ. Associations of visual function with physical outcomes and limitations 5 years later in an older population: The Beaver Dam eye study. Ophthalmology. 2003;110:644–50.
Black AA, Wood JM, Lovie-Kitchin JE. Inferior field loss increases rate of falls in older adults with glaucoma. Optom Vis Sci. 2011;88:1275–82.
Coleman AL, Cummings SR, Yu F, Kodjebacheva G, Ensrud KE, Gutierrez P, et al. Binocular visual-field loss increases the risk of future falls in older white women. J Am Geriatr Soc. 2007;55:357–64.
Sotimehin AE, Yonge AV, Mihailovic A, West SK, Friedman DS, Gitlin LN, et al. Locations, Circumstances, and Outcomes of Falls in Patients With Glaucoma. Am J Ophthalmol. 2018;192:131–41.
Bramley T, Peeples P, Walt JG, Juhasz M, Hansen JE. Impact of vision loss on costs and outcomes in medicare beneficiaries with glaucoma. Arch Ophthalmol. 2008;126:849–56.
McGwin G Jr, Mays A, Joiner W, Decarlo DK, McNeal S, Owsley C. Is glaucoma associated with motor vehicle collision involvement and driving avoidance? Invest Ophthalmol Vis Sci. 2004;45:3934–9.
Haymes SA, Leblanc RP, Nicolela MT, Chiasson LA, Chauhan BC. Risk of falls and motor vehicle collisions in glaucoma. Invest Ophthalmol Vis Sci. 2007;48:1149–55.
Kwon M, Huisingh C, Rhodes LA, McGwin G Jr, Wood JM, Owsley C. Association between Glaucoma and At-fault Motor Vehicle Collision Involvement among Older Drivers: A Population-based Study. Ophthalmology. 2016;123:109–16.
Hu PS, Trumble DA, Foley DJ, Eberhard JW, Wallace RB. Crash risks of older drivers: a panel data analysis. Accid Anal Prev. 1998;30:569–81.
Tanabe S, Yuki K, Ozeki N, Shiba D, Abe T, Kouyama K, et al. The association between primary open-angle glaucoma and motor vehicle collisions. Invest Ophthalmol Vis Sci. 2011;52:4177–81.
van Landingham SW, Hochberg C, Massof RW, Chan E, Friedman DS, Ramulu PY. Driving patterns in older adults with glaucoma. BMC Ophthalmol. 2013;13:4.
Ramulu PY, West SK, Munoz B, Jampel HD, Friedman DS. Driving cessation and driving limitation in glaucoma: the Salisbury Eye Evaluation Project. Ophthalmology. 2009;116:1846–53.
Gilhotra JS, Mitchell P, Ivers R, Cumming RG. Impaired vision and other factors associated with driving cessation in the elderly: The Blue Mountains Eye Study. Clin Exp Ophthalmol. 2001;29:104–7.
Bhargava JS, Patel B, Foss AJ, Avery AJ, King AJ. Views of glaucoma patients on aspects of their treatment: an assessment of patient preference by conjoint analysis. Invest Ophthalmol Vis Sci. 2006;47:2885–8.
Nguyen AM, van Landingham SW, Massof RW, Rubin GS, Ramulu PY. Reading ability and reading engagement in older adults with glaucoma. Invest Ophthalmol Vis Sci. 2014;55:5284–90.
Burton R, Saunders LJ, Crabb DP. Areas of the visual field important during reading in patients with glaucoma. Jpn J Ophthalmol. 2015;59:94–102.
Glen FC, Crabb DP, Smith ND, Burton R, Garway-Heath DF. Do patients with glaucoma have difficulty recognizing faces? Invest Ophthalmol Vis Sci. 2012;53:3629–37.
Zhang X, Olson DJ, Le P, Lin FC, Fleischman D, Davis RM. The Association Between Glaucoma, Anxiety, and Depression in a Large Population. Am J Ophthalmol. 2017;183:37–41.
Jung KI, Park CK. Mental Health Status and Quality of Life in Undiagnosed Glaucoma Patients: A Nationwide Population-Based Study. Medicine (Baltimore). 2016;95:e3523.
Lim NC, Fan CH, Yong MK, Wong EP, Yip LW. Assessment of Depression, Anxiety, and Quality of Life in Singaporean Patients With Glaucoma. J Glaucoma. 2016;25:605–12.
Su CC, Chen JY, Wang TH, Huang JY, Yang CM, Wang IJ. Risk factors for depressive symptoms in glaucoma patients: a nationwide case-control study. Graefes Arch Clin Exp Ophthalmol. 2015;253:1319–25.
Wang SY, Singh K, Lin SC. Prevalence and predictors of depression among participants with glaucoma in a nationally representative population sample. Am J Ophthalmol. 2012;154:436–444 e2.
Mabuchi F, Yoshimura K, Kashiwagi K, Shioe K, Yamagata Z, Kanba S, et al. High prevalence of anxiety and depression in patients with primary open-angle glaucoma. J Glaucoma. 2008;17:552–7.
Zhou C, Qian S, Wu P, Qiu C. Anxiety and depression in Chinese patients with glaucoma: sociodemographic, clinical, and self-reported correlates. J Psychosom Res. 2013;75:75–82.
Ramulu PY, Mihailovic A, West SK, Gitlin LN, Friedman DS. Predictors of Falls per Step and Falls per Year At and Away From Home in Glaucoma. Am J Ophthalmol. 2019;200:169–78.
McKean-Cowdin R, Varma R, Wu J, Hays RD, Azen SP. Los Angeles Latino Eye Study G, Severity of visual field loss and health-related quality of life. Am J Ophthalmol. 2007;143:1013–23.
McKean-Cowdin R, Wang Y, Wu J, Azen SP, Varma R, Los Angeles Latino Eye Study G. Impact of visual field loss on health-related quality of life in glaucoma: the Los Angeles Latino Eye Study. Ophthalmology. 2008;115:941–948 e1.
Gutierrez P, Wilson MR, Johnson C, Gordon M, Cioffi GA, Ritch R, et al. Influence of glaucomatous visual field loss on health-related quality of life. Arch Ophthalmol. 1997;115:777–84.
Che Hamzah J, Burr JM, Ramsay CR, Azuara-Blanco A, Prior M. Choosing appropriate patient-reported outcomes instrument for glaucoma research: a systematic review of vision instruments. Qual Life Res. 2011;20:1141–58.
Quaranta L, Riva I, Gerardi C, Oddone F, Floriani I, Konstas AG. Quality of Life in Glaucoma: A Review of the Literature. Adv Ther. 2016;33:959–81.
Vandenbroeck S, De Geest S, Zeyen T, Stalmans I, Dobbels F. Patient-reported outcomes (PRO's) in glaucoma: a systematic review. Eye (Lond). 2011;25:555–77.
Dempster M, McCorry NK, Donnelly M, Barton K, Azuara-Blanco A. Individualisation of glaucoma quality of life measures: a way forward? Br J Ophthalmol. 2019;103:293–5.
Nelson P, Aspinall P, Papasouliotis O, Worton B, O'Brien C. Quality of life in glaucoma and its relationship with visual function. J Glaucoma. 2003;12:139–50.
Medeiros FA, Gracitelli CP, Boer ER, Weinreb RN, Zangwill LM, Rosen PN. Longitudinal changes in quality of life and rates of progressive visual field loss in glaucoma patients. Ophthalmology. 2015;122:293–301.
Abe RY, Diniz-Filho A, Costa VP, Gracitelli CP, Baig S, Medeiros FA. The Impact of Location of Progressive Visual Field Loss on Longitudinal Changes in Quality of Life of Patients with Glaucoma. Ophthalmology. 2016;123:552–7.
Odberg T. Visual field prognosis in advanced glaucoma. Acta Ophthalmol. 1987;65(suppl):27–29.
Grant WM, Burke JF Jr. Why do some people go blind from glaucoma? Ophthalmology. 1982;89:991–8.
Wilson R, Walker AM, Dueker DK, Crick RP. Risk factors for rate of progression of glaucomatous visual field loss: a computer-based analysis. Arch Ophthalmol. 1982;100:737–41.
Mikelberg FS, Schulzer M, Drance SM, Lau W. The rate of progression of scotomas in glaucoma. Am J Ophthalmol. 1986;101:1–6.
Lee JM, Caprioli J, Nouri-Mahdavi K, Afifi AA, Morales E, Ramanathan M, et al. Baseline prognostic factors predict rapid visual field deterioration in glaucoma. Invest Ophthalmol Vis Sci. 2014;55:2228–36.
Oliver JE, Hattenhauer MG, Herman D, Hodge DO, Kennedy R, Fang-Yen M, et al. Blindness and glaucoma: a comparison of patients progressing to blindness from glaucoma with patients maintaining vision. Am J Ophthalmol. 2002;133:764–72.
Mokhles P, Schouten JS, Beckers HJ, Azuara-Blanco A, Tuulonen A, Webers CA. A Systematic Review of End-of-Life Visual Impairment in Open-Angle Glaucoma: An Epidemiological Autopsy. J Glaucoma. 2016;25:623–8.
Goh YW, Ang GS, Azuara-Blanco A. Lifetime visual prognosis of patients with glaucoma. Clin Experiment Ophthalmol. 2011;39:766–70.
Ernest PJ, Busch MJ, Webers CA, Beckers HJ, Hendrikse F, Prins MH, et al. Prevalence of end-of-life visual impairment in patients followed for glaucoma. Acta Ophthalmol. 2013;91:738–43.
Hattenhauer MG, Johnson DH, Ing HH, Herman DC, Hodge DO, Yawn BP, et al. The probability of blindness from open-angle glaucoma. Ophthalmology. 1998;105:2099–104.
Mokhles P, Schouten JS, Beckers HJ, Azuara-Blanco A, Tuulonen A, Webers CA. Glaucoma blindness at the end of life. Acta Ophthalmol. 2017;95:10–11.
Forsman E, Kivela T, Vesti E. Lifetime visual disability in open-angle glaucoma and ocular hypertension. J Glaucoma. 2007;16:313–9.
Ang GS, Eke T. Lifetime visual prognosis for patients with primary open-angle glaucoma. Eye (Lond). 2007;21:604–8.
Griffith JF, Goldberg JL. Prevalence of comorbid retinal disease in patients with glaucoma at an academic medical center. Clin Ophthalmol. 2015;9:1275–84.
Kolar P. Risk factors for central and branch retinal vein occlusion: a meta-analysis of published clinical data. J Ophthalmol. 2014;2014:724780.
Yin X, Li J, Zhang B, Lu P. Association of glaucoma with risk of retinal vein occlusion: A meta-analysis. Acta Ophthalmol. 2019;97:652–9.
Rahman MQ, Beard SM, Discombe R, Sharma R, Montgomery DM. Direct healthcare costs of glaucoma treatment. Br J Ophthalmol. 2013;97:720–4.
Grodum K, Heijl A, Bengtsson B. Glaucoma and mortality. Graefes Arch Clin Exp Ophthalmol. 2004;242:397–401.
Peters D, Bengtsson B, Heijl A. Lifetime risk of blindness in open-angle glaucoma. Am J Ophthalmol. 2013;156:724–30.
Garway-Heath DF, Crabb DP, Bunce C, Lascaratos G, Amalfitano F, Anand N, et al. Latanoprost for open-angle glaucoma (UKGTS): a randomised, multicentre, placebo-controlled trial. Lancet. 2015;385:1295–304.
The AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000;130:429–40.
Maier PC, Funk J, Schwarzer G, Antes G, Falck-Ytter YT. Treatment of ocular hypertension and open angle glaucoma: meta-analysis of randomised controlled trials. BMJ. 2005;331:134.
The Collaborative Normal-Tension Glaucoma Study Group. Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Am J Ophthalmol. 1998;126:487–97.
Lichter PR, Musch DC, Gillespie BW, Guire KE, Janz NK, Wren PA, et al. Interim clinical outcomes in the Collaborative Initial Glaucoma Treatment Study comparing initial treatment randomized to medications or surgery. Ophthalmology. 2001;108:1943–53.
Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ, Johnson CA, et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120:714–20. discussion 829-30
Ederer F, Gaasterland DE, Sullivan EK. The Advanced Glaucoma Intervention Study (AGIS): 1. Study design and methods and baseline characteristics of study patients. Control Clin Trials. 1994;15:299–325.
Greenrod EB, Jones MNA, Kaye S, Larkin DFP. Center and surgeon effect on outcomes of endothelial keratoplasty versus penetrating keratoplasty in the United Kingdom. American Journal of Ophthalmology. 2014;158:957–66.
Gedde SJ, Schiffman JC, Feuer WJ, Parrish RK 2nd, Heuer DK, Brandt JD, et al. The tube versus trabeculectomy study: design and baseline characteristics of study patients. Am J Ophthalmol. 2005;140:275–87.
Gedde SJ, Feuer WJ, Shi W, Lim KS, Barton K, Goyal S, et al. Treatment Outcomes in the Primary Tube Versus Trabeculectomy Study after 1 Year of Follow-up. Ophthalmology. 2018;125:650–63.
Kirwan JF, Lockwood AJ, Shah P, Macleod A, Broadway DC, King AJ, et al. Trabeculectomy in the 21st century: a multicenter analysis. Ophthalmology. 2013;120:2532–9.
Stead RE, King AJ. Outcome of trabeculectomy with mitomycin C in patients with advanced glaucoma. Br J Ophthalmol. 2011;95:960–5.
Burr J, Azuara-Blanco A, Avenell A, Tuulonen A. Medical versus surgical interventions for open angle glaucoma. Cochrane Database of Systematic Reviews, 2012: https://doi.org/10.1002/14651858.CD004399.pub3.
Smith R. A comparison between medical and surgical treatment of glaucoma simplex–results of a prospective study. Trans Ophthalmol Soc Aust. 1968;27:17–29.
Migdal C, Gregory W, Hitchings R, Kolker AE. Long-term functional outcome after early surgery compared with laser and medicine in open-angle glaucoma. Ophthalmology. 1994;101:1651–7.
Jay JL, Murray SB. Early trabeculectomy versus conventional management in primary open angle glaucoma. Br J Ophthalmol. 1988;72:881–9.
The European Glaucoma Society. Terminology and Guidelines for Glaucoma. 4th ed. 2014, Italy.
Prum BE Jr, Rosenberg LF, Gedde SJ, Mansberger SL, Stein JD, Moroi SE, et al. Primary Open-Angle Glaucoma Preferred Practice Pattern Guidelines. Ophthalmology. 2016;123:P41–p111.
Stead R, Azuara-Blanco A, King AJ. Attitudes of consultant ophthalmologists in the UK to initial management of glaucoma patients presenting with severe visual field loss: a national survey. Clin Experiment Ophthalmol. 2011;39:858–64.
Moster MR, Moster ML. Wipe-out: a complication of glaucoma surgery or just a blast from the past? Am J Ophthalmol. 2005;140:705–6.
Law SK, Nguyen AM, Coleman AL, Caprioli J. Severe loss of central vision in patients with advanced glaucoma undergoing trabeculectomy. Arch Ophthalmol. 2007;125:1044–50.
Costa VP, Smith M, Spaeth GL, Gandham S, Markovitz B. Loss of visual acuity after trabeculectomy. Ophthalmology. 1993;100:599–612.
Balekudaru S, George R, Panday M, Singh M, Neog A, Lingam V. Prospective evaluation of early visual loss following glaucoma-filtering surgery in eyes with split fixation. J Glaucoma. 2014;23:211–8.
Topouzis F, Tranos P, Koskosas A, Pappas T, Anastasopoulos E, Dimitrakos S, et al. Risk of sudden visual loss following filtration surgery in end-stage glaucoma. Am J Ophthalmol. 2005;140:661–6.
Guedes RA, Guedes VM, Freitas SM, Chaoubah A. Quality of life of medically versus surgically treated glaucoma patients. J Glaucoma. 2013;22:369–73.
Varma R, Lee PP, Goldberg I, Kotak S. An assessment of the health and economic burdens of glaucoma. Am J Ophthalmol. 2011;152:515–22.
Rouland JF, Berdeaux G, Lafuma A. The economic burden of glaucoma and ocular hypertension: implications for patient management: a review. Drugs Aging. 2005;22:315–21.
Traverso CE, Walt JG, Kelly SP, Hommer AH, Bron AM, Denis P, et al. Direct costs of glaucoma and severity of the disease: a multinational long term study of resource utilisation in Europe. Br J Ophthalmol. 2005;89:1245–9.
Bunce C, Xing W, Wormald R. Causes of blind and partial sight certifications in England and Wales: April 2007-March 2008. Eye (Lond). 2010;24:1692–9.
Pezzullo L, Streatfeild J, Simkiss P, Shickle D. The economic impact of sight loss and blindness in the UK adult population. BMC Health Serv Res. 2018;18:63.
Chakravarthy U, Biundo E, Saka RO, Fasser C, Bourne R, Little JA. The Economic Impact of Blindness in Europe. Ophthalmic Epidemiol. 2017;24:239–47.
Meads C, Hyde C. What is the cost of blindness? Br J Ophthalmol. 2003;87:1201–4.
Thygesen J, Aagren M, Arnavielle S, Bron A, Frohlich SJ, Baggesen K, et al. Late-stage, primary open-angle glaucoma in Europe: social and health care maintenance costs and quality of life of patients from 4 countries. Curr Med Res Opin. 2008;24:1763–70.
Department of Health. Improving outcomes and supporting transparency in Public Health Outcomes Framework. 2012, London.
King AJ, Stead RE, Rotchford AP. Treating patients presenting with advanced glaucoma - should we reconsider current practice? Br J Ophthalmol. 2011;95:1185–92.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kastner, A., King, A.J. Advanced glaucoma at diagnosis: current perspectives. Eye 34, 116–128 (2020). https://doi.org/10.1038/s41433-019-0637-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-019-0637-2
This article is cited by
-
Visual and surgical outcomes of MMC augmented combined non-penetrating deep sclerectomy and phacoemulsification in eyes with severe and end stage glaucoma
Eye (2025)
-
Visual field progression in Asian glaucoma patients: a 10-year stratified cohort analysis from a national health system with universal coverage
Graefe's Archive for Clinical and Experimental Ophthalmology (2025)
-
Clinical Benefits of Preservative-Free Treatment for Glaucoma with a Focus on Preservative-Free Latanoprost
Ophthalmology and Therapy (2025)
-
Leveraging Alzheimer’s Disease Omics to Identify Pleiotropic Genes Contributing to Neurodegeneration in Primary Open-Angle Glaucoma
Molecular Neurobiology (2025)
-
Associations of human blood metabolome with optic neurodegenerative diseases: a bi-directionally systematic mendelian randomization study
Lipids in Health and Disease (2024)