Abstract
Purpose
To evaluate the management and long-term outcomes of patients with diabetic macular oedema (DMO) and good initial visual acuity in real-world settings.
Methods
We reviewed 122 eyes of 100 patients with treatment-naive DMO and initial best-corrected visual acuity (BCVA) of 20/25 or better. We assessed clinical characteristics, logMAR BCVA, central subfield thickness (CST), cumulative intravitreal injections and laser treatments at yearly intervals, and characteristics at time of initial treatment. Linear mixed effects models were used to identify predictors of visual outcomes.
Results
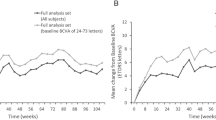
At presentation, mean BCVA was 0.057 ± 0.048 logMAR (Snellen 20/23) and mean CST was 288 ± 57 μm. After a median follow-up of 3 years, 51% of eyes underwent treatment. More eyes underwent intravitreal injection as initial treatment (54%), but lasers were initiated at an earlier time and at better BCVA. Final BCVA was associated with better BCVA (P < 0.001) and earlier timing (P = 0.017) at initial treatment, but not CST at first treatment (P = 0.634) or cumulative number of injections or lasers (P = 0.441–0.606).
Conclusion
DMO with good initial visual acuity should be monitored closely, as delay in treatment initiation is associated with worse visual outcomes. BCVA at time of initial treatment is the strongest determinant of final visual acuity.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Klein R, et al. The Wisconsin epidemiologic study of diabetic retinopathy. IV. Diabetic macular edema. Ophthalmology. 1984;91:1464–74.
Todorich B, Yiu G, Hahn P. Current and investigational pharmacotherapeutic approaches for modulating retinal angiogenesis. Expert Rev Clin Pharm. 2014;7:375–91.
Lois N, et al. Diabetic macular oedema and diode subthreshold micropulse laser (DIAMONDS): study protocol for a randomised controlled trial. Trials. 2019;20:122.
Chen G, et al. Subthreshold micropulse diode laser versus conventional laser photocoagulation for diabetic macular edema: a meta-analysis of randomized controlled trials. Retina. 2016;36:2059–65.
Moisseiev E, et al. Subthreshold micropulse laser reduces anti-VEGF injection burden in patients with diabetic macular edema. Eur J Ophthalmol. 2018;28:68–73.
Vujosevic S, et al. Subthreshold micropulse yellow laser versus subthreshold micropulse infrared laser in center-involving diabetic macular edema: morphologic and functional safety. Retina. 2015;35:1594–603.
Hagenau F, et al. Vitrectomy for diabetic macular edema: optical coherence tomography criteria and pathology of the vitreomacular interface. Am J Ophthalmol. 2019;200:34–46.
Hu XY, et al. Efficacy and safety of vitrectomy with internal limiting membrane peeling for diabetic macular edema: a Meta-analysis. Int J Ophthalmol. 2018;11:1848–55.
Diabetic Retinopathy Clinical Research N. et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2010;117:1064–77 e1035.
Nguyen QD, et al. Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology. 2012;119:789–801.
Heier JS, et al. Intravitreal aflibercept for diabetic macular edema: 148-week results from the VISTA and VIVID studies. Ophthalmology. 2016;123:2376–85.
Korobelnik JF, et al. Intravitreal aflibercept for diabetic macular edema. Ophthalmology. 2014;121:2247–54.
Diabetic Retinopathy Clinical Research N. et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. New Engl J Med. 2015;372:1193–203.
Wells JA, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema: two-year results from a comparative effectiveness randomized clinical trial. Ophthalmology. 2016;123:1351–9.
Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Early Treatment Diabetic Retinopathy Study research group. Arch Ophthalmol. 1985;103:1796–806.
Baker CW, et al. Effect of initial management with aflibercept vs laser photocoagulation vs observation on vision loss among patients with diabetic macular edema involving the center of the macula and good visual acuity: a randomized clinical trial. JAMA. 2019;321:1880–94.
Yiu G, et al. Effect of anti-vascular endothelial growth factor therapy on choroidal thickness in diabetic macular edema. Am J Ophthalmol. 2014;158:745–51 e742.
Moisseiev E, et al. 25-gauge vitrectomy with epiretinal membrane and internal limiting membrane peeling in eyes with very good visual acuity. Curr eye Res. 2016;41:1387–92.
Funding
BPD is supported by NIH UL1 TR001860. AM is supported by NIH K08 EY027463, NIH U24 EY029904. LSM received personal fees for consultancy from Genentech & Iridex. SSP is supported by NIH 1UG1EY026876 and received grant from received grant support from Allergan and Roche Novartis. GY is supported by NIH K08 EY026101, E. Matilda Ziegler Foundation for the Blind, Barr Foundation for Retinal Research, and Macula Society, received grant support from Alcon, Clearside Biomedical, and Iridex, and personal fees for consultancy from Alimera, Allergan, Carl Zeiss Meditec, Genentech, and Iridex. No funding organisations had any role in the design or conduct of this research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Luu, KY., Akhter, M.M., Durbin-Johnson, B.P. et al. Real-world management and long-term outcomes of diabetic macular oedema with good visual acuity. Eye 34, 1108–1115 (2020). https://doi.org/10.1038/s41433-019-0647-0
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-019-0647-0