Abstract
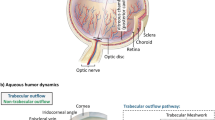
Despite glaucoma being the second leading cause of blindness globally, its pathogenesis remains incompletely understood. Although intraocular pressure (IOP) contributes to glaucoma, and reducing IOP slows progress of the disease, some patients progress despite normal IOP (NTG). Glaucomatous damage causes characteristic cupping of the optic nerve where it passes through the lamina cribrosa. There is evidence that cerebrospinal fluid (CSF) within the optic nerve sheath has a different composition from CSF surrounding the brain. Furthermore, fluctuations in CSF flow into the optic nerve sheath may be reduced by trabeculae within the sheath, and on standing intracranial pressure (ICP) within the sheath is stabilised at around 3 mmHg due to orbital pressure. Blood pressure has been linked both to glaucoma and ICP. These facts have led some to conclude that ICP does not play a role in glaucoma. However, according to stress formulae and Laplace’s Law, stress within the lamina cribrosa is dependent on the forces on either side of it, (IOP and ICP), and its thickness. On lying flat at night, ICP between the brain and optic nerve sheath should equalise. Most evidence suggests ICP is lower in glaucoma than in control groups, and that the lamina cribrosa is thinner and more posteriorly displaced in glaucoma. Subjects who have had ICP reduced have developed signs of glaucoma. This review finds most evidence supports a role for low ICP in the pathogenesis of glaucoma. Caffeine, theophylline and vitamin A may increase ICP, and could be new candidates for an oral treatment.
摘要
青光眼为全球第二大致盲眼病, 其发病机制仍不完全清楚。尽管眼内压 (IOP) 为青光眼发病的主要因素, 降低IOP可减缓病情发展, 但有些患者尽管IOP正常仍可发展为青光眼 (NTG), 导致穿过筛板处的视神经特征性的视杯改变。有证据表明, 视神经鞘内的脑脊液 (CSF) 与大脑周围的CSF中的成分不同。此外, 鞘内的小梁可以减少CSF流入视神经鞘, 从而减少IOP的波动, 鞘内颅内压 (ICP) 在静止时由于眼眶压可稳定在3mmHg左右。血压与青光眼和ICP有关。这些事实可以得出结论: ICP与青光眼的发病作用不大。
然而, 根据应力公式和拉普拉斯定律, 筛板内部的应力取决于其两侧的力量 (眼压和颅内压) 及其厚度。夜间平躺时, 大脑和视神经鞘之间的ICP应是均衡的。大多数证据表明青光眼患者的ICP低于对照组, 并且青光眼患者的筛板更薄且更后移, 降低ICP后, 受试者出现了青光眼症状。
本综述发现大多数证据支持低颅内压在青光眼发病中的作用。咖啡因、茶碱和维生素A有增加颅内压的可能, 因此也可能成为新的候选口服药物。
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Leske MC. Open-angle glaucoma—an epidemiologic overview. Ophthalmic Epidemiol. 2007;14:166–72.
Anderson DR. Normal tension glaucoma study Collaborative normal tension glaucoma study. Curr Opin Ophthalmol. 2003;14:86–90.
Garway-Heath DF, Crabb DP, Bunce C, Lascaratos G, Amalfitano F, Anand N, et al. Latanoprost for open-angle glaucoma (UKGTS): a randomised, multicentre, placebo-controlled trial. Lancet. 2015;385:1295–304.
Sommer A, Tielsch JM, Katz J, Quigley HA, Gottsch JD, Javitt J, et al. Relationship between intraocular pressure and primary open angle glaucoma among white and black Americans. The Baltimore Eye Survey. Arch Ophthalmol. 1991;109:1090–5.
Iwase A, Suzuki Y, Araie M, Yamamoto T, Abe H, Shirato S, et al. The prevalence of primary open-angle glaucoma in Japanese. Ophthalmology. 2004;111:1641–8.
Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120:701–13.
Drance SM, Sweeney VP, Morgan RW, Feldman F. Studies of factors involved in the production of low tension glaucoma. Arch Ophthalmol. 1973;89:457–65.
Flammer J, Orgül S, Costa VP, Orzalesi N, Krieglstein GK, Serra LM, et al. The impact of ocular blood flow in glaucoma. Prog Retin Eye Res. 2002;21:359–93.
Killer HE, Jaggi GP, Flammer J, Miller NR. Is open-angle glaucoma caused by impaired cerebrospinal fluid circulation: around the optic nerve? Clin Exp Ophthalmol. 2008;36:308–11.
Hammam T, Montgomery D, Morris D, Imrie F. Prevalence of serum autoantibodies and paraproteins in patients with glaucoma. Eye. 2008;22:349–53.
Sigal IA, Flanagan JG, Tertinegg I, Ethier CR. Predicted extension, compression and shearing of optic nerve head tissues. Exp Eye Res. 2007;85:312–22.
Wang YX, Xu L, Wei WBin, Jonas JB. Intraocular pressure and its normal range adjusted for ocular and systemic parameters. The Beijing Eye Study 2011. PLoS ONE Public Libr Sci. 2018;13:e0196926.
Ren R, Jonas JB, Tian G, Zhen Y, Ma K, Li S, et al. Cerebrospinal fluid pressure in glaucoma. Ophthalmology. 2010;117:259–66.
Magnaes B. Body position and cerebrospinal fluid pressure. J Neurosurg. 1976;44:698–705.
Jain MR, Marmion VJ. Rapid pneumatic and Mackey-Marg applanation tonometry to evaluate the postural effect on intraocular pressure. Br J Ophthalmol. 1976;60:687–93.
Morgan WH, Balaratnasingam C, Lind CRP, Colley S, Kang MH, House PH, et al. Cerebrospinal fluid pressure and the eye. Br J Ophthalmol. 2016;100:71–7.
Hayreh SS. Cerebrospinal fluid pressure and glaucomatous optic disc cupping. Graefe’s Arch Clin Exp Ophthalmol. 2009;247:721–4.
Li L, Bian A, Cheng G, Zhou Q. Posterior displacement of the lamina cribrosa in normal-tension and high-tension glaucoma. Acta Ophthalmol. 2016;94:e492–500.
Kim YW, Kim DW, Jeoung JW, Kim DM, Park KH. Peripheral lamina cribrosa depth in primary open-angle glaucoma: a swept-source optical coherence tomography study of lamina cribrosa. Eye. 2015;29:1368–74.
Wells AP, Garway-Heath DF, Poostchi A, Wong T, Chan KCY, Sachdev N. Corneal Hysteresis but not corneal thickness correlates with optic nerve surface compliance in glaucoma patients. Investig Opthalmology Vis Sci. 2008;49:3262.
Digre KB, Nakamoto BK, Warner JEA, Langeberg WJ, Baggaley SK, Katz BJ. A comparison of idiopathic intracranial hypertension with and without papilledema. Headache NIH Public Access. 2009;49:185–93.
Killer HE, Laeng HR, Flammer J, Groscurth P. Architecture of arachnoid trabeculae, pillars, and septa in the subarachnoid space of the human optic nerve: anatomy and clinical considerations. Br J Ophthalmol. 2003;87:777–81.
Costa VP, Arcieri ES, Harris A. Blood pressure and glaucoma. Br J Ophthalmol. 2009;93:1276–82.
Fleischman D, Bicket AK, Stinnett SS, Berdahl JP, Jonas JB, Wang NL, et al. Analysis of cerebrospinal fluid pressure estimation using formulae derived from clinical data. Investig Opthalmology Vis Sci Assoc Res Vis Ophthalmol. 2016;57:5625.
Wang N, Xie X, Yang D, Xian J, Li Y, Ren R, et al. Orbital cerebrospinal fluid space in glaucoma: the Beijing Intracranial and Intraocular Pressure (iCOP) Study. Ophthalmology. 2012;119:2065–2073.e1.
Berdahl JP, Allingham RR, Johnson DH. Cerebrospinal fluid pressure is decreased in primary open-angle glaucoma. Ophthalmology. 2008;115:763–8.
Ren R, Wang N, Zhang X, Cui T, Jonas JB. Trans-lamina cribrosa pressure difference correlated with neuroretinal rim area in glaucoma. Graefe’s Arch Clin Exp Ophthalmol. 2011;249:1057–63.
Downs JC, Roberts MD, Burgoyne CF. Mechanical environment of the optic nerve head in glaucoma. Optom Vis Sci. 2008;85:E425–35.
Young W, Budynas R, Sadegh A, Roark R. Roark’s formulas for stress and strain. 8th ed. Blackwell’s, New York; 2012.
Feola AJ, Myers JG, Raykin J, Mulugeta L, Nelson ES, Samuels BC, et al. Finite element modeling of factors influencing optic nerve head deformation due to intracranial pressure. Investig Opthalmology Vis Sci. 2016;57:1901.
Hua Y, Voorhees AP, Sigal IA. Cerebrospinal fluid pressure: revisiting factors influencing optic nerve head biomechanics. Investig Opthalmology Vis Sci. 2018;59:154.
Tong J, Ghate D, Kedar S, Gu L. Relative contributions of intracranial pressure and intraocular pressure on lamina cribrosa behavior. J Ophthalmol. 2019;2019:1–8.
Hou R, Zhang Z, Yang D, Wang H, Chen W, Li Z, et al. Intracranial pressure (ICP) and optic nerve subarachnoid space pressure (ONSP) correlation in the optic nerve chamber: the Beijing Intracranial and Intraocular Pressure (iCOP) study. Brain Res. 2016;1635:201–8.
Morgan WH, Yu DY, Alder VA, Cringle SJ, Cooper RL, House PH, et al. The correlation between cerebrospinal fluid pressure and retrolaminar tissue pressure. Invest Ophthalmol Vis Sci. 1998;39:1419–28.
Bidot S, Bruce BB, Saindane AM, Newman NJ, Biousse V. Asymmetric papilledema in idiopathic intracranial hypertension. J Neuro-Ophthalmol. 2015;35:31–6.
Bidot S, Clough L, Saindane AM, Newman NJ, Biousse V, Bruce BB. The optic canal size is associated with the severity of papilledema and poor visual function in idiopathic intracranial hypertension. J Neuro-Ophthalmol. 2016;36:120–5.
Mathieu E, Gupta N, Paczka-Giorgi LA, Zhou X, Ahari A, Lani R, et al. Reduced cerebrospinal fluid inflow to the optic nerve in glaucoma. Investig Opthalmology Vis Sci. 2018;59:5876.
Killer HE, Miller NR, Flammer J, Meyer P, Weinreb RN, Remonda L, et al. Cerebrospinal fluid exchange in the optic nerve in normal-tension glaucoma. Br J Ophthalmol. 2012;96:544–8.
Jaggi GP, Mironov A, Huber AR, Killer HE. Optic nerve compartment syndrome in a patient with optic nerve sheath meningioma. Eur J Ophthalmol. 2007;17:454–8.
Plog BA, Nedergaard M. The glymphatic system in central nervous system health and disease: past, present, and future. Annu Rev Pathol NIH Public Access. 2018;13:379–94.
Geeraerts T, Newcombe VF, Coles JP, Abate M, Perkes IE, Hutchinson PJ, et al. Use of T2-weighted magnetic resonance imaging of the optic nerve sheath to detect raised intracranial pressure. Crit Care. 2008;12:R114.
Chen L, Wang L, Hu Y, Jiang X, Wang Y, Xing Y. Ultrasonic measurement of optic nerve sheath diameter: a non-invasive surrogate approach for dynamic, real-time evaluation of intracranial pressure. Br J Ophthalmol BMJ Publ Group Ltd. 2019;103:437–41.
Watanabe A, Kinouchi H, Horikoshi T, Uchida M, Ishigame K. Effect of intracranial pressure on the diameter of the optic nerve sheath. J Neurosurg. 2008;109:255–8.
Cennamo G, Montorio D, Breve MA, Brescia Morra V, Menna F, Cennamo G. Evaluation of optic nerve subarachnoid space in primary open angle glaucoma using ultrasound examination. PLoS ONE. 2018;13:e0208064.
Pircher A, Montali M, Berberat J, Remonda L, Killer HE. Relationship between the optic nerve sheath diameter and lumbar cerebrospinal fluid pressure in patients with normal tension glaucoma. Eye. 2017;31:1365–72.
Serot J-M, Zmudka J, Jouanny P. A possible role for csf turnover and choroid plexus in the pathogenesis of late onset Alzheimer’s disease. J Alzheimer’s Dis. 2012;30:17–26.
Preston JE. Ageing choroid plexus-cerebrospinal fluid system. Microsc Res Tech. 2001;52:31–7.
Tamura H, Kawakami H, Kanamoto T, Kato T, Yokoyama T, Sasaki K, et al. High frequency of open-angle glaucoma in Japanese patients with Alzheimer’s disease. J Neurol Sci. 2006;246:79–83.
Chang TC, Singh K. Glaucomatous disease in patients with normal pressure hydrocephalus. J Glaucoma. 2009;18:243–6.
Kessing LV, Lopez AG, Andersen PK, Kessing SV. No increased risk of developing alzheimer disease in patients with glaucoma. J Glaucoma. 2007;16:47–51.
Yoneda S, Hara H, Hirata A, Fukushima M, Inomata Y, Tanihara H. Vitreous fluid levels of β-amyloid(1–42) and tau in patients with retinal diseases. Jpn J Ophthalmol. 2005;49:106–8.
Park H-YL, Jeon SH, Park CK. Enhanced depth imaging detects lamina cribrosa thickness differences in normal tension glaucoma and primary open-angle glaucoma. Ophthalmology. 2012;119:10–20.
Kwun Y, Han JC, Kee C. Comparison of lamina cribrosa thickness in normal tension glaucoma patients with unilateral visual field defect. Am J Ophthalmol. 2015;159:512–518.e1.
Jonas JB, Berenshtein E, Holbach L. Lamina cribrosa thickness and spatial relationships between intraocular space and cerebrospinal fluid space in highly myopic eyes. Investig Opthalmology Vis Sci. 2004;45:2660.
Bae SH, Kang SH, Feng CS, Park J, Jeong JH, Yi K. Influence of myopia on size of optic nerve head and retinal nerve fiber layer thickness measured by spectral domain optical coherence tomography. Korean J Ophthalmol Korean Ophthalmological Soc. 2016;30:335–43.
Girkin CA, Fazio MA, Yang H, Reynaud J, Burgoyne CF, Smith B, et al. Variation in the three-dimensional histomorphometry of the normal human optic nerve head with age and race: lamina cribrosa and peripapillary scleral thickness and position. Invest Ophthalmol Vis Sci Assoc Res Vis Ophthalmol. 2017;58:3759–69.
Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ, Johnson CA, et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol (Chic, Ill 1960). 2002;120:714–20. discussion 829–30.
Marcus MW, de Vries MM, Montolio FGJ, Jansonius NM. Myopia as a risk factor for open-angle glaucoma: a systematic review and meta-analysis. Ophthalmology. 2011;118:1989–1994.e2.
Lee EJ, Kim T-W, Weinreb RN, Kim H. Reversal of lamina cribrosa displacement after intraocular pressure reduction in open-angle glaucoma. Ophthalmology. 2013;120:553–9.
Yan DB, Coloma FM, Metheetrairut A, Trope GE, Heathcote JG, Ethier CR. Deformation of the lamina cribrosa by elevated intraocular pressure. Br J Ophthalmol. 1994;78:643–8.
Perez-Lopez M, Ting DSJ, Clarke L. Lamina cribrosa displacement after optic nerve sheath fenestration in idiopathic intracranial hypertension: a new tool for monitoring changes in intracranial pressure? Br J Ophthalmol. 2014;98:1603–4.
Morgan WH, Chauhan BC, Yu D-Y, Cringle SJ, Alder VA, House PH. Optic disc movement with variations in intraocular and cerebrospinal fluid pressure. Investig Ophthalmol Vis Sci. 2002;43:3236–42.
Jonas JB, Holbach L. Central corneal thickness and thickness of the lamina cribrosa in human eyes. Investig Opthalmology Vis Sci. 2005;46:1275.
Sigal IA. Interactions between geometry and mechanical properties on the optic nerve head. Investig Opthalmology Vis Sci. 2009;50:2785.
Berdahl JP, Fautsch MP, Stinnett SS, Allingham RR. Intracranial pressure in primary open angle glaucoma, normal tension glaucoma, and ocular hypertension: a case–control study. Investig Opthalmology Vis Sci. 2008;49:5412.
Abegão Pinto L, Vandewalle E, Pronk A, Stalmans I. Intraocular pressure correlates with optic nerve sheath diameter in patients with normal tension glaucoma. Graefes Arch Clin Exp Ophthalmol. 2012;250:1075–80.
Siaudvytyte L, Januleviciene I, Daveckaite A, Ragauskas A, Siesky B, Harris A. Neuroretinal rim area and ocular haemodynamic parameters in patients with normal-tension glaucoma with differing intracranial pressures. Br J Ophthalmol. 2016;100:1134–8.
Lee SH, Kwak SW, Kang EM, Kim GA, Lee SY, Bae HW, et al. Estimated trans-lamina cribrosa pressure differences in low-teen and high-teen intraocular pressure normal tension glaucoma: the Korean National Health and Nutrition Examination Survey. PLoS ONE. 2016;11:e0148412.
Wang YX, Jonas JB, Wang NX, You QS, Yang D. Intraocular pressure and estimated cerebrospinal fluid pressure. the Beijing Eye Study. PLoS ONE. 2014;9:104267.
Xie X, Zhang X, Fu J, Wang H, Jonas JB, Peng X, et al. Noninvasive intracranial pressure estimation by orbital subarachnoid space measurement: the Beijing Intracranial and Intraocular Pressure (iCOP) study. Crit Care. 2013;17:R162.
Jonas JB, Nangia V, Wang N, Bhate K, Nangia P, Nangia P, et al. Trans-lamina cribrosa pressure difference and open-angle glaucoma. The Central India Eye and Medical Study. PLoS ONE. 2013;8:e82284.
Loiselle AR, de Kleine E, van Dijk P, Jansonius NM. Noninvasive intracranial pressure assessment using otoacoustic emissions: an application in glaucoma. PLoS ONE. 2018;13:e0204939.
Bershad EM, Urfy MZ, Pechacek A, McGrath M, Calvillo E, Horton NJ, et al. Intracranial pressure modulates distortion product otoacoustic emissions. Neurosurgery. 2014;75:445–55.
Lindén C, Qvarlander S, Jóhannesson G, Johansson E, Östlund F, Malm J, et al. Normal-tension glaucoma has normal intracranial pressure. Ophthalmology. 2018;125:361–8.
Pircher A, Remonda L, Weinreb RN, Killer HE. Translaminar pressure in Caucasian normal tension glaucoma patients. Acta Ophthalmol. 2017;95:e524–31.
Igarashi N, Honjo M, Asano S, Takagi K, Aihara M. Optic disc cupping characteristics of normal pressure hydrocephalus patients with normal-tension glaucoma. Sci Rep Nat Publ Group. 2019;9:3108.
Gallina P, Savastano A, Becattini E, Orlandini S, Scollato A, Rizzo S, et al. Glaucoma in patients with shunt-treated normal pressure hydrocephalus. J Neurosurg. 2018;129:1078–84.
Yablonski M, Ritch R, Pokorny K. Effect of decreased intracranial pressure on optic disc. Investig Ophthalmol Vis Sci. 1979;18:165.
Yang D, Fu J, Hou R, Liu K, Jonas JB, Wang H, et al. Optic neuropathy induced by experimentally reduced cerebrospinal fluid pressure in monkeys. Investig Opthalmology Vis Sci. 2014;55:3067.
Zhao D, He Z, Vingrys AJ, Bui BV, Nguyen CTO. The effect of intraocular and intracranial pressure on retinal structure and function in rats. Physiol Rep. 2015;3:e12507.
Bäuerle J, Schuchardt F, Schroeder L, Egger K, Weigel M, Harloff A. Reproducibility and accuracy of optic nerve sheath diameter assessment using ultrasound compared to magnetic resonance imaging. BMC Neurol. 2013;13:187.
Kavi T, Gupta A, Hunter K, Schreiber C, Shaikh H, Turtz AR. Optic nerve sheath diameter assessment in patients with intracranial pressure monitoring. Cureus. 2018;10:e3546.
Xu L, Wang H, Wang Y, Jonas JB. Intraocular pressure correlated with arterial blood pressure: the Beijing Eye Study. Am J Ophthalmol. 2007;144:461–2.
Mitchell P, Smith W, Attebo K, Healey PR. Prevalence of open-angle glaucoma in Australia. The Blue Mountains Eye Study. Ophthalmology. 1996;103:1661–9.
Leske MC, Wu S-Y, Hennis A, Honkanen R, Nemesure B. Risk factors for incident open-angle glaucoma. Ophthalmology. 2008;115:85–93.
Topouzis F, Coleman AL, Harris A, Jonescu-Cuypers C, Yu F, Mavroudis L, et al. Association of blood pressure status with the optic disk structure in non-glaucoma subjects: the Thessaloniki Eye Study. Am J Ophthalmol. 2006;142:60–67.e1.
Hayreh SS. The role of age and cardiovascular disease in glaucomatous optic neuropathy. Surv Ophthalmol. 1999;43:S27–42.
Yilmaz KC, Sur Gungor S, Ciftci O, Akman A, Muderrisoglu H. Relationship between primary open angle glaucoma and blood pressure. Acta Cardiol. 2019;16:1–5.
Graham SL, Drance SM, Wijsman K, Douglas GR, Mikelberg FS. Ambulatory blood pressure monitoring in glaucoma. The nocturnal dip. Ophthalmol. 1995;102:61–9.
He Z, Nguyen CTO, Armitage JA, Vingrys AJ, Bui BV. Blood pressure modifies retinal susceptibility to intraocular pressure elevation. PLoS ONE Public Libr Sci. 2012;7:e31104.
Li M, Wang M, Guo W, Wang J, Sun X. The effect of caffeine on intraocular pressure: a systematic review and meta-analysis. Graefe’s Arch Clin Exp Ophthalmol. 2011;249:435–42.
Han M-E, Kim H-J, Lee Y-S, Kim D-H, Choi J-T, Pan C-S, et al. Regulation of cerebrospinal fluid production by caffeine consumption. BMC Neurosci BioMed Cent. 2009;10:110.
Basurto Ona X, Martínez García L, Solà I, Bonfill Cosp X. Drug therapy for treating post-dural puncture headache. Cochrane Database Syst Rev. 2011;10:CD007887.
Fraunfelder F, Fraunfelder FT, Corbett JJ. Isotretinoin-associated intracranial hypertension*1. Ophthalmology. 2004;111:1248–50.
de Botton S, Coiteux V, Chevret S, Rayon C, Vilmer E, Sanz M, et al. Outcome of childhood acute promyelocytic leukemia with all- trans-retinoic acid and chemotherapy. J Clin Oncol. 2004;22:1404–12.
Jacobson DM, Berg R, Wall M, Digre KB, Corbett JJ, Ellefson RD. Serum vitamin A concentration is elevated in idiopathic intracranial hypertension. Neurology. 1999;53:1114–8.
Tabassi A, Salmasi AH, Jalali M. Serum and CSF vitamin A concentrations in idiopathic intracranial hypertension. Neurology. 2005;64:1893–6.
Friedman DI, Gordon LK, Egan RA, Jacobson DM, Pomeranz H, Harrison AR, et al. Doxycycline and intracranial hypertension. Neurology. 2004;62:2297–9.
Gardner K, Cox T, Digre KB. Idiopathic intracranial hypertension associated with tetracycline use in fraternal twins: case reports and review. Neurology. 1995;45:6–10.
Chiu AM, Chuenkongkaew WL, Cornblath WT, Trobe JD, Digre KB, Dotan SA, et al. Minocycline treatment and pseudotumor cerebri syndrome. Am J Ophthalmol. 1998;126:116–21.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Baneke, A.J., Aubry, J., Viswanathan, A.C. et al. The role of intracranial pressure in glaucoma and therapeutic implications. Eye 34, 178–191 (2020). https://doi.org/10.1038/s41433-019-0681-y
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-019-0681-y
This article is cited by
-
Systemic Carbonic Anhydrase Inhibitors in Common Ophthalmic Diseases: A Scoping Review from A Clinical Standpoint
Current Ophthalmology Reports (2025)
-
Large-scale in-silico analysis of CSF dynamics within the subarachnoid space of the optic nerve
Fluids and Barriers of the CNS (2024)
-
Derivation, external and clinical validation of a deep learning approach for detecting intracranial hypertension
npj Digital Medicine (2024)
-
Normal intraocular pressure in Egyptian children and meta-analysis
Eye (2022)
-
Response to “Comment on: The role of intracranial pressure in glaucoma and therapeutic implications”
Eye (2021)