Abstract
Purpose
To estimate informal caregiver (ICG) strain in people from a glaucoma clinic.
Methods
Patients with glaucoma were consecutively identified from a single clinic in England for a cross-sectional postal survey. The sample was deliberately enriched with a number of patients designated as having advanced glaucoma (visual field [VF] mean deviation worse than −12 dB in both eyes). Patients were asked to identify an ICG who recorded a Modified Caregiver Strain Index (MCSI), a validated 13 item instrument scored on a scale of 0–26. Previous research has indicated mean MCSI to be >10 in multiple sclerosis and Parkinson’s disease. All participants gave a self-reported measure of general health (EQ5D).
Results
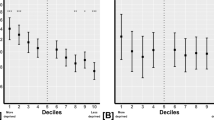
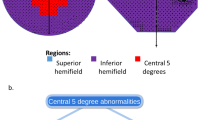
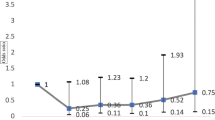
Responses from 105 patients (43% of those invited) were analysed; only 38 of the 105 named an ICG. Mean (95% confidence interval [CI]) MCSI was 2.4 (1.3, 3.6) and only three ICGs recorded a MCSI > 7. The percentage of patients with an ICG was much higher in patients with advanced VF loss (82%; 9/11) when compared with those with non-advanced VF loss (31%; 29/94; p = 0.001). Mean (standard deviation) MCSI was considerably inflated in the advanced patients (5.6 [4.9] vs 1.5 [2.2] for non-advanced; p = 0.040). Worsening VF and poorer self-reported general health (EQ5D) of the patient were associated with worsening MCSI.
Conclusion
ICG strain, as measured by MCSI, for patients with non-advanced glaucoma is negligible, compared with other chronic disease. ICG strain increases moderately with worsening VFs but this could be partly explained by worse general health in our sample of patients.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Crabb DP. A view on glaucoma—are we seeing it clearly? Eye (Lond). 2016;30:304–13.
Glen FC, Crabb DP. Living with glaucoma: a qualitative study of functional implications and patients’ coping behaviours. BMC Ophthalmol. 2015;15:128.
Shtein RM, Newman-Casey PA, Herndon L, Coleman AL, Lee PP. Assessing the role of the family/support system perspective in patients with glaucoma. J Glaucoma. 2016;25:e676–e680.
Keeffe JE, Chou SL, Lamoureux EL. The cost of care for people with impaired vision in Australia. Arch Ophthalmol. 2009;127:1377–81.
Burleson Sullivan A, Miller D. Who is taking care of the caregiver? J Patient Exp. 2015;2:7–12.
Peters M, Jenkinson C, Doll H, Playford D, Fitzpatrick R. Carer quality of life and experiences of health services: a cross-sectional survey across three neurological conditions. Health Qual Life Outcomes. 2013;11:103.
van den Heuvel E, de Witte L, Schure L, Sanderman R, Meyboom-de Jong B. Risk-factors for burn-out in caregivers for stroke patients, and possibilities for intevention. Clin Rehabil. 2001;40:669–667.
Yee J, Schulz R. Gender differences in psychiatric morbidity among family caregivers: a review and analysis. Gerontologist. 2000;36:147–64.
McCullagh E, Brigstocke G, Donaldson N, Kalra L. Determinants of caregiving burden and quality of life in caregivers of stroke patients. Stroke. 2005;36:2181–6.
Royal College of General Practitioners and Royal College of Nursing. Matters of life and death: helping people to live well until they die. London: Royal College of General Practitioners and Royal College of Nursing; 2012. http://www.rcgp.org.uk/clinical-and-research/toolkits/~/media/Files/CIRC/Matters%20of%20Life%20and%20Death%20FINAL.ashx. Accessed Nov 2019.
Northouse LL, Katapodi MC, Schafenecker AM, Weiss D. The impact of caregiving on the psychological well-being of family caregivers and cancer patients. Semin Oncol Nurs. 2012;28:236–45.
Chang S, Zhang Y, Jeyagurunathan A, Lau YW, Sagayadevan V, Chong SA, et al. Providing care to relatives with mental illness: reactions and distress among primary informal caregivers. BMC Psychiatry. 2016;16:80.
Schmier JK, Halpern MT, Covert D, Delgado J, Sharma S. Impact of visual impairment on use of caregiving by individuals with age-related macular degeneraton. Retina. 2006;26:1056–62.
Gohil R, Crosby-Nwaobi R, Forbes A, Burton B, Hykin P, Sivaprasad S. Caregiver burden in patients recieving ranibizumab therapy for neovascular macular degeneration. PLOS ONE. 2015;10:e0129361.
Vukicevic M, Heraghty J, Cummins R, Gopinath B, Mitchell P. Caregiver perceptions about the impact of caring for patients with wet age-related macular degeneration. Eye (Lond). 2016;30:413–21.
Hanemoto T, Hikichi Y, Kikuci N, Kozawa T. The impact of different anti-vascular endothelial growth factor treatment regimens on reducing burden for caregivers and patients with wet age-related macular degeneration in a single-center real-world Japanese setting. PLOS ONE. 2017;12:e0189035.
Gopinath B, Craig A, Kifley A, Liew G, Bloffwitch J, van Vu J, et al. Implementing a multi-modal support service model for the family caregivers of persons with age-related macular degeneration: a study protocol for a randomised controlled trial. BMJ Open. 2017;7:e018204.
Gothwal K, Bharani S, Mandal SK. Glaucoma quality of life of caregivers of children with congenital glaucoma: development and validation of a novel questionnaire (CarCGQoL). Invest Ophthalmol Vis Sci. 2015;56:770–7.
Kantipuly A, Pillai MR, Shroff S, Khatiwala R, Raman GV, Krishnadas SR, et al. Caregiver burden in primary congenital glaucoma. Am J Ophthalmol. 2019. https://doi.org/10.1016/j.ajo.2019.05.003
Thornton M, Travis SS. Analysis of the reliability of the modified caregiver strain index. J Gerontol B Psychol Sci Soc Sci. 2003;58:S127–S13.
Boodhna T, Crabb DP. More frequent, more costly? Health economic modelling aspects of monitoring glaucoma patients in England. BMC Health Serv Res. 2016;16:611.
Saunders LJ, Russell RA, Crabb DP. Practical landmarks for visual field disability in glaucoma. Br J Ophthalmol. 2012;96:1185–9.
van Hout B, Janssen MF. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health. 2012;15:708–15.
van den Burg B, Al M, van Exel J, Koopmanschap M, Brouwer W. Economic valuation of informal care: conjoint analysis applied in a heterogeneous population of informal caregivers. Value Health. 2008;11:1041–50.
Ariza-Vega P, Ortiz-Pina M, Kristensen MT, Castellote-Caballero Y, Jimenez-Moleon JJ. High perceived caregiver burden for relatives of patients following hip fracture surgery. Disabil Rehabil. 2019;41:311–8.
Hsu T, Loscalzo M, Ramani R, Forman S, Popplewell L, Clark K, et al. Are disagreements in caregiver and patient assessment of patient health associated with increased caregiver burden in caregivers of older adults with cancer? Oncologist. 2017;22:1383–91.
van der Hiele K, van Gorp DAM, Heerings MAP, Jongen P, van der Klink JJL, Frequin STFM, et al. Caregiver strain among life partners of persons with mild disability due to relapsing-remitting multiple sclerosis. Mult Scler Rel Dis. 2019;31:5–11.
Peters D, Heijl A, Brenner L, Bengtsson B. Visual impairment and vision related quality of life in the early manigest glaucoma trial after 20 years of follow up. Acta Ophthalmol. 2015;93:745–52.
Jones L, Bryan SR, Crabb DP. Gradually then suddenly? Decline in vision-related quality of life as glaucoma worsens. J Opthalmol. 2017;2017:7 https://doi.org/10.1155/2017/1621640
Marques AP, Macedo AF, Hernandez-Moreno L, Ramos PL, Butt T, Rubin G, et al. The use of informal care by people with vision impairment. PLOS ONE. 2018;13:e0198631.
Skalicky SE, Lamoureux EL, Crabb DP, Ramulu PY. Patient-reported outcomes, functional assessment, and utility values in glaucoma. J Glaucoma. 2019;28:89–96.
Jones L, Garway-Heath DF, Azuara-Blanco A, Crabb DP, UKGTS Investigators. Are patient self-reported outcome measures sensitive enough to be used as end points in clinical trials? Evidence from the United Kingdom Glaucoma Treatment Study. Ophthalmology. 2019;126:682–9.
Bhargava JS, Bhan-Bhargava A, Foss AJ, King AJ. Views of glaucoma patients on provision of follow-up care; an assessment of patient preferences by conjoint analysis. Br J Ophthalmol. 2008;92:1601–5.
Read S, Waterman H, Morgan JE, Harper RA, Spencer AF, Stanford P. Glaucoma, dementia, and the “precipice of care”: transitions between states of medication adherence. Patient Prefer Adherence. 2018;12:1315–25.
Haley WE, Roth DL, Howard G, Safford MM. Caregiving strain and estimated risk for stroke and coronary heart disease among spouse caregivers. Differential effects by race and sex. Stroke. 2010;41:331–6.
Funding
This work was supported by an unrestricted investigator initiated grant from Santen UK and Santen International but they had no role in the design of the study, collection and analysis of data or decision to publish.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
McDonald, L., Turnbull, P., Chang, L. et al. Taking the strain? Impact of glaucoma on patients' informal caregivers. Eye 34, 197–204 (2020). https://doi.org/10.1038/s41433-019-0688-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-019-0688-4
This article is cited by
-
What support do caregivers of people with visual impairment receive and require? An exploratory study of UK healthcare and charity professionals’ perspectives
Eye (2022)
-
Family reported outcomes, an unmet need in the management of a patient's disease: appraisal of the literature
Health and Quality of Life Outcomes (2021)