Abstract
Objective
To compare fibrin glue (with three cardinal sutures) (FG) and polygalactin suture (PS) for mucous membrane grafting (MMG) in terms of graft apposition and recurrence of lid margin keratinization (LMK) and metaplastic lashes (ML) in patients with Stevens–Johnson syndrome (SJS).
Design
Prospective randomized comparative interventional study.
Methods
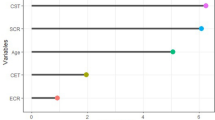
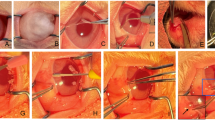
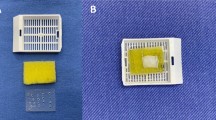
Twenty patients diagnosed with SJS and lid margin abnormalities including LMK with or without ML were randomized to undergo either fibrin glue (FG)-assisted MMG (n = 10) or continuous 8-0 polygalactin suture (PS)-assisted MMG (n = 10). They were evaluated preoperatively and during follow-up at 1 week and 1, 2, 3, and 6 months. The parameters assessed were best-corrected visual acuity (BCVA), tear break-up time (TBUT), Schirmer-1 test, corneal and conjunctival complications, graft apposition and width (GW), LMK, ML, impression cytology, and operative time. The primary outcome measures are incidence of graft displacement and recurrence of LMK and ML.
Results
None of the eyelids in FG group (0/40) and 1 eyelid in PS group (1/40) had graft displacement. Recurrence of LMK occurred in 7.5% of eyelids (3/40) in both the study groups. Recurrence of ML occurred in 2.5% (1/40) in FG group and 5% (2/40) in PS group. The mean operative time for MMG in FG group was 39.5 ± 2.40 min and in PS group was 56 ± 1.63 min (p = 0.001).
Conclusions
As graft apposition with suture involves significantly longer intraoperative time, if cost is not a limiting factor then fibrin glue is a viable option for the MMG for lid margin pathologies.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Dipascuale M, Espana E, Liu D, Kawakita T, Li W, Gao Y, et al. Correlation of corneal complications with eyelid cicatricial pathologies in patients with Stevens–Johnson syndrome and toxic epidermal necrolysis syndrome. Ophthalmology. 2005;112:904–12.
Pullum K, Buckley R. Therapeutic and ocular surface indications for scleral contact lenses. Ocul Surf. 2007;5:40–8.
Iyer G, Pillai VS, Srinivasan B, Guruswami S, Padmanabhan P. Mucous membrane grafting for lid margin keratinization in Stevens–Johnson syndrome: results. Cornea. 2010;29:146–51.
Fu Y, Liu J, Tseng SCG. Oral mucosal graft to correct lid margin pathologic features in cicatricial ocular surface diseases. Am J Ophthalmol. 2011;152:600–608.e1.
Koranyi G, Seregard S, Kopp ED. Cut and paste: a no suture, small incision approach to pterygium surgery. Br J Ophthalmol. 2004;88:911–4.
Sharma N, Thenarasun SA, Kaur M, Pushker N, Khanna N, Agarwal T, et al. Adjuvant role of amniotic membrane transplantation in acute ocular stevens-johnson syndrome: a randomized control trial. Ophthalmology. 2016;123:484–91.
Queiroz de Paiva AR, Abreu de Azevedo Fraga L, Torres VLL. Surgical reconstruction of ocular surface tumors using fibrin sealant tissue adhesive. Ocul Oncol Pathol. 2016;2:207–11.
Bahar I, Weinberger D, Dan G, Avisar R. Pterygium surgery: fibrin glue versus vicryl sutures for conjunctival closure. Cornea. 2006;25:1168–72.
Hall RC, Logan AJ, Wells AP. Comparison of fibrin glue with sutures for pterygium excision surgery with conjunctival autografts. Clin Exp Ophthalmol. 2009;37:584–9.
Ratnalingam V, Keat Eu AL, Ng GL, Taharin R, John E. Fibrin adhesive is better than sutures in pterygium surgery. Cornea. 2010;29:485–9.
Sotozono C, Ang LPK, Koizumi N, Higashihara H, Ueta M, Inatomi T, et al. New grading system for the evaluation of chronic ocular manifestations in patients with Stevens-Johnson syndrome. Ophthalmology. 2007;114:1294–302.
Kompella VB, Sangwan VS, Bansal AK, Garg P, Aasuri MK, Rao GN. Ophthalmic complications and management of Stevens-Johnson syndrome at a tertiary eye care centre in south India. Indian J Ophthalmol. 2002;50:283–6.
Weinberg DA, Tham V, Hardin N, Antley C, Cohen AJ, Hunt K, et al. Eyelid mucous membrane grafts: a histologic study of hard palate, nasal turbinate, and buccal mucosal grafts. Ophthal Plast Reconstr Surg. 2007;23:211–6.
Henderson HWA, Collin JRO. Mucous membrane grafting. In: Geerling G, Brewitt H, editors. Developments in ophthalmology. Basel: Karger; 2008. p. 230–42.
Araújo ALde, Ricardo JRdaS, Sakai VN, Barros JNde, Gomes JÁP. Impression cytology and in vivo confocal microscopy in corneas with total limbal stem cell deficiency. Arq Bras Oftalmol. 2013;76:305–8.
Fatima A, Iftekhar G, Sangwan VS, Vemuganti GK. Ocular surface changes in limbal stem cell deficiency caused by chemical injury: a histologic study of excised pannus from recipients of cultured corneal epithelium. Eye. 2008;22:1161–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pushker, N., Gorimanipalli, B., Sharma, N. et al. Mucous membrane grafting (fibrin glue vs. suture) for lid margin pathologies in Stevens–Johnson syndrome: randomized comparative study. Eye 35, 1985–1992 (2021). https://doi.org/10.1038/s41433-020-01203-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-020-01203-4