Abstract
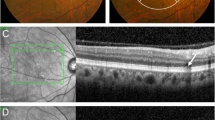
The pachychoroid disease spectrum encompasses seven major retinal conditions including central serous chorioretinopathy (CSC), polypoidal choroidal vasculopathy (PCV), and pachychoroid neovasculopathy or type I macular neovascularisation (MNV) secondary to chronic persistent thickening and dysfunction of the choroidal vasculature. Drusen are focal yellow-white deposits of extracellular debris, which consist of complement proteins, esterified and nonesterified cholesterol, apolipoproteins, carbohydrates, and trace elements, above the retinal pigment epithelium (RPE) or between the RPE and Bruch’s membrane. Although drusen are an essential disease precursor of advanced age-related macular degeneration (AMD), a new entity “pachydrusen” has been identified to be associated with some of the enitites that constitute the pachychoroid spectrum. It remains to be determined what the exact differences are between soft drusen, pseudodrusen, and pachydrusen in terms of phenotype, genotype, and pathogenesis. Improving our knowledge in these areas will inevitably improve our understanding of their clinical significance especially as in disease prediction in AMD and the pachychroid spectrum disorders. It remains controversial whether PCV is a subtype of AMD. Understanding the pathogenesis of different types of drusen may also help in addressing if phenotype and/or genotype of type 1 MNV associated with pachychoroid are similar to type 1 MNV related to AMD. Furthermore, because pachydrusen links two pachychoroid diseases, CSC and PCV, it is also of great interest to investigate if CSC is an early stage or a predictor of PCV in future research. In this review, we share our experience in clinical practice and the latest published evidence-based literature to emphasize the differences and similarities in morphology, pathogenesis, and clinical significance of drusen and pachydrusen, a new member of the pachychoroid spectrum disorders.
摘要
肥厚型脉络膜疾病(Pachychoroidal diseases, PCD)目前主要涵盖七类视网膜脉络膜疾病, 包括中心性浆液性脉络膜视网膜病变(central serous chorioretinopathy, CSC), 息肉状脉络膜血管病变 (polypoidal choroidal vasculopathy, PCV)以及肥厚性脉络膜新生血管即I型黄斑新生血管 (macular neovascularization, MNV)等, 这些疾病的共同特征为慢性的、持续性脉络膜增厚或功能障碍。玻璃膜疣 (drusen) 是富含补体蛋白、酯化及非酯化胆固醇、载脂蛋白、糖类以及微量元素的局灶性黄白色细胞外碎片状沉着物, 沉积于视网膜色素上皮层或视网膜色素上皮与Bruch膜之间。Drusen是老年性黄斑变性(age related macular degeneration, AMD)的重要预测因素。新命名的“与肥厚型脉络膜疾病相关的drusen (pachydrusen)”已被证实与肥厚型脉络膜疾病谱中的一些疾病相关。然而, 软性drusen、假性drusen和pachydrusen在表型、基因型、发病机制方面的具体区别尚待阐明。在此方面的深入认识, 有助于深入理解drusen的临床意义及其对AMD和肥厚型脉络膜疾病的预测作用。PCV是否为AMD亚型仍存在争议, 掌握不同类型drusen的发病机制将有助于理解drusen 与pachydrusen的临床意义, 特别是在预测AMD及肥厚型脉络膜疾病方面的作用。另外, 由于pachydrusen与两类肥厚型脉络膜疾病CSC和PCV相关, 在未来的研究中, CSC是否为PCV的早期阶段或预测因素也值得进一步研究论证。本篇综述从临床实践经验和最新的循证证据出发, 探讨了drusen和肥厚型脉络膜疾病谱家族的新成员pachydrusen在形态、发病机制和临床意义方面的异同。
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Warrow DJ, Hoang QV, Freund KB. Pachychoroid pigment epitheliopathy. Retina. 2013;33:1659–72.
Pang CE, Freund KB. Pachychoroid neovasculopathy. Retina. 2015;35:1.
Gallego-Pinazo R, Dolz-Marco R, Gómez-Ulla F, Mrejen S, Freund KB. Pachychoroid diseases of the macula. Med Hypothesis Discov Innov Ophthalmol. 2014;3:111–5.
Kim JH, Chang YS, Kim JW, Lee TG, Kim CG. Prevalence of subtypes of reticular pseudodrusen in newly diagnosed exudative age-related macular degeneration and polypoidal choroidal vasculopathy in Korean patients. Retina. 2015;35:2604–12.
Donders FC. Beiträge zur pathologischen Anatomie des Auges. Graef Arch Clin Exp. 1855;1:106–18.
Anatomische HM. Beiträge zur ophthalmologie – untersuchungen über die Glashäute des Auges, insbesondere die Glaslamelle der Chorioidea und ihre senilen Veränderungen. Graefes Arch Clin Exp. 1856;2:1–69.
Mimoun G, Soubrane G, Coscas G. [Macular drusen]. J Franais Dophtalmologie. 1990;13:511–30.
Rabiolo A, Sacconi R, Cicinelli MV, Querques L, Bandello F, Querques G. Spotlight on reticular pseudodrusen. Clin Ophthalmol. 2017;11:1707–18.
Arnold JJ, Sarks SH, Killingsworth MC, Sarks JP. Reticular pseudodrusen. A risk factor in age-related maculopathy. Retina. 1995;15:183–91.
Klein R, Meuer SM, Knudtson MD, Iyengar SK, Klein BE. The epidemiology of retinal reticular drusen. Am J Ophthalmol. 2008;145:317–26.
Finger RP, Chong E, McGuinness MB, Robman LD, Aung KZ, Giles G, et al. Reticular pseudodrusen and their association with age-related macular degeneration: the melbourne collaborative cohort study. Ophthalmology. 2016;123:599–608.
Joachim N, Mitchell P, Rochtchina E, Tan AG, Wang JJ. Incidence and progression of reticular drusen in age-related macular degeneration: findings from an older Australian cohort. Ophthalmology. 2014;121:917–25.
Klein R, Klein BE, Knudtson MD, Meuer SM, Swift M, Gangnon RE. Fifteen-year cumulative incidence of age-related macular degeneration: the Beaver Dam Eye Study. Ophthalmology. 2007;114:253–62.
Knudtson MD, Klein R, Klein BE. Physical activity and the 15-year cumulative incidence of age-related macular degeneration: the Beaver Dam Eye Study. Br J Ophthalmol. 2006;90:1461–3.
Armstrong J, Davis M, Danis Jr R, Klein R, Klein B, Lee LY, et al. Reticular drusen as a baseline risk factor for progression to advanced AMD in AREDS. Invest Ophthalmol Vis Sci. 2005;46. --this is a conference (ARVO) Abstract.
Schmitz-Valckenberg S, Alten F, Steinberg JS, Jaffe GJ, Fleckenstein M, Mukesh BN, et al. Reticular drusen associated with geographic atrophy in age-related macular degeneration. Invest Ophthalmol Vis Sci. 2011;52:5009–15.
Gil JQ, Marques JP, Hogg R, Rosina C, Cachulo ML, Santos A, et al. Clinical features and long-term progression of reticular pseudodrusen in age-related macular degeneration: findings from a multicenter cohort. Eye. 2017;31:364–71.
Cohen SY, Dubois L, Tadayoni R, Delahaye-Mazza C, Debibie C, Quentel G. Prevalence of reticular pseudodrusen in age-related macular degeneration with newly diagnosed choroidal neovascularisation. Br J Ophthalmol. 2007;91:354–9.
Ueda-Arakawa N, Ooto S, Nakata I, Yamashiro K, Tsujikawa A, Oishi A, et al. Prevalence and genomic association of reticular pseudodrusen in age-related macular degeneration. Am J Ophthalmol. 2013;155:260–269.e2.
Hogg RE, Silva R, Staurenghi G, Murphy G, Santos AR, Rosina C, et al. Clinical characteristics of reticular pseudodrusen in the fellow eye of patients with unilateral neovascular age-related macular degeneration. Ophthalmology. 2014;121:1748–55.
Naysan J, Jung JJ, Dansingani KK, Balaratnasingam C, Freund KB. Type 2 (subretinal) neovascularization in age-related macular degeneration associated with pure reticular pseudodrusen phenotype. Retina. 2016;36:449–57.
Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol. 2001;119:1417–36.
Spaide RF, Curcio CA. Drusen characterization with multimodal imaging. Retina. 2010;30:1441–54.
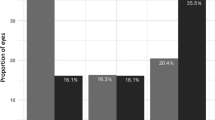
Lee J, Byeon SH. Prevalence and clinical characteristics of pachydrusen in polypoidal choroidal vasculopathy: multimodal image study. Retina. 2019;39:670–8.
Fukuda Y, Sakurada Y, Sugiyama A, Yoneyama S, Matsubara M, Kikushima W, et al. Title: Pachydrusen in fellow eyes predict response to aflibercept monotherapy in patients with polypoidal choroidal vasculopathy. J Clin Med. J Clin Med. 2020;9:2459. https://doi.org/10.3390/jcm9082459.
Matsubara M, Sakurada Y, Sugiyama A, Fukuda Y, Parikh R, Kashiwagi K. Response to photodynamic therapy combined with intravitreal aflibercept for polypoidal choroidal vasculopathy depending on fellow-eye condition:2-year results. PLoS ONE. 2020;15:e0237330.
Yanagi Y. Pachychoroid disease: a new perspective on exudative maculopathy. Jpn J Ophthalmol. 2020;64:323–37.
Lee J, Kim M, Lee CS, Kim SS, Koh HJ, Lee SC, et al. Drusen subtypes and choroidal characteristics in Asian eyes with typical neovascular age-related macular degeneration. Retina. 2020;40:490–8.
Cheung CMG, Gan A, Yanagi Y, Wong TY, Spaide R. Association between choroidal thickness and drusen subtypes in age-related macular degeneration. Opthalmol Retina. 2018;2:1196–205.
Yamashiro K, Hosoda Y, Miyake M, Ooto S, Tsujikawa A. Characteristics of pachychoroid diseases and age-related macular degeneration: multimodal imaging and genetic backgrounds. J Clin Med. 2020;9:2034. https://doi.org/10.3390/jcm9072034.
Singh SR, Chakurkar R, Goud A, Rasheed MA, Vupparaboina KK, Chhablani J. Pachydrusen in polypoidal choroidal vasculopathy in an Indian cohort. Indian J Ophthalmol. 2019;67:1121–6.
Fukuda Y, Sakurada Y, Yoneyama S, Kikushima W, Sugiyama A, Matsubara M, et al. Clinical and genetic characteristics of pachydrusen in patients with exudative age-related macular degeneration. Sci Rep. 2019;9:11906.
Matsumoto H, Mukai R, Morimoto M, Tokui S, Kishi S, Akiyama H. Clinical characteristics of pachydrusen in central serous chorioretinopathy. Graefes Arch Clin Exp. 2019;257:1127–32.
Singh SR, Chakurkar R, Goud A, Chhablani J. Low incidence of pachydrusen in central serous chorioretinopathy in an Indian cohort. Indian J Ophthalmol. 2020;68:118–22.
Takahashi A HY, Miyake M, Oishi A, Ooto S, Tsujikawa A. Clinical and genetic characteristic of pachydrusen in eyes with central serous chorioretinopathy and normal subjects. Invest Ophthalmol Vis Sci. 2019;60.5005. (ARVO abstract).
Sartini F, Figus M, Casini G, Nardi M, Posarelli C. Pachychoroid neovasculopathy: a type-1 choroidal neovascularization belonging to the pachychoroid spectrum-pathogenesis, imaging and available treatment options. International Ophthalmology. 2020;30. https://doi.org/10.1007/s10792-020-01522-1.
Zhang X, Lai TYY. Paying attention to the concept and research of pachychoroid disease spectrum. Chin J Exp Ophthalmol. 2017;35:385–90.
Klein R, Cruickshanks KJ, Nash SD, Krantz EM, Nieto FJ, Huang GH, et al. The prevalence of age-related macular degeneration and associated risk factors. Arch Ophthalmol. 2010;128:750–8.
Silvestri G, Williams MA, McAuley C, Oakes K, Sillery E, Henderson DC, et al. Drusen prevalence and pigmentary changes in Caucasians aged 18–54 years. Eye. 2012;26:1357–62.
Bressler NM, Bressler SB, West SK, Fine SL, Taylor HR. The grading and prevalence of macular degeneration in Chesapeake Bay watermen. Arch Ophthalmol. 1989;107:847–52.
Mitchell P, Smith W, Attebo K, Wang JJ. Prevalence of age-related maculopathy in Australia. The Blue Mountains Eye Study. Ophthalmology. 1995;102:1450–60.
Klein R, Klein BE, Linton KL. Prevalence of age-related maculopathy. The Beaver Dam Eye Study. Ophthalmology. 1992;99:933–43.
Buitendijk GH, Hooghart AJ, Brussee C, de Jong PT, Hofman A, Vingerling JR, et al. Epidemiology of reticular pseudodrusen in age-related macular degeneration: the Rotterdam Study. Invest Ophthalmol Vis Sci. 2016;57:5593–601.
Chan H, Cougnard-Grégoire A, Delyfer M-N, Combillet F, Rougier M-B, Schweitzer C, et al. Multimodal imaging of reticular pseudodrusen in a population-based setting: the Alienor Study. Invest Ophthalmol Vis Sci. 2016;57:3058–65.
Zarubina AV, Neely DC, Clark ME, Huisingh CE, Samuels BC, Zhang Y, et al. Prevalence of subretinal drusenoid deposits in older persons with and without age-related macular degeneration, by multimodal imaging. Ophthalmology. 2016;123:1090–100.
Alten F, Clemens CR, Milojcic C, Eter N. Subretinal drusenoid deposits associated with pigment epithelium detachment in age-related macular degeneration. Retina. 2012;32:1727–32.
Sohrab MA, Smith RT, Salehi-Had H, Sadda SR, Fawzi AA. Image registration and multimodal imaging of reticular pseudodrusen. Invest Ophthalmol Vis Sci. 2011;52:5743–8.
Smith RT, Sohrab MA, Busuioc M, Barile G. Reticular macular disease. Am J Ophthalmol. 2009;148:733–43.e2.
Spaide RF. Disease expression in nonexudative age-related macular degeneration varies with choroidal thickness. Retina. 2018;38:708–16.
Singh SR, Oli A, Mohan S, Goud A, Rasheed MA, Vupparaboina KK, et al. Pachydrusen in Indian population: a hospital-based study. Indian J Ophthalmol. 2019;67:371–5.
Dansingani KK, Perlee LT, Hamon S, Lee M, Shah VP, Spaide RF, et al. Risk alleles associated with neovascularization in a pachychoroid phenotype. Ophthalmology. 2016;123:2628–30.
Age-Related Eye Disease Study Research Group. The Age-Related Eye Disease Study system for classifying age-related macular degeneration from stereoscopic color fundus photographs: the Age-Related Eye Disease Study report number 6. Am J Ophthalmol. 2001;132:668–81.
Uchida A, Srivastava SK, Manjunath D, Singh RP, Rachitskaya AV, Kaiser PK, et al. Impact of drusen burden on incidence of subclinical MNV with OCTA. Opthalmic Surg Lasers Imaging Retina. 2019;51:22–30.
Tan AC, Pilgrim MG, Fearn S, Bertazzo S, Tsolaki E, Morrell AP, et al. Calcified nodules in retinal drusen are associated with disease progression in age-related macular degeneration. Sci Transl Med. 2018;10:eaat4544. https://doi.org/10.1126/scitranslmed.aat4544.
Klein R, Meuer SM, Knudtson MD, Iyengar SK, Klein BE. The epidemiology of retinal reticular drusen. Am J Ophthalmol. 2008;145:317–26.
Switzer DW Jr, MendonÇa LS, Saito M, Zweifel SA, Spaide RF. Segregation of ophthalmoscopic characteristics according to choroidal thickness in patients with early age-related macular degeneration. Retina. 2012;32:1265–71.
Boddu S, Lee MD, Marsiglia M, Marmor M, Freund KB, Smith RT. Risk factors associated with reticular pseudodrusen versus large soft drusen. Am J Ophthalmol. 2014;157:985–993.e2.
Wilde C, Patel M, Lakshmanan A, Morales MA, Dhar-Munshi S, Amoaku WM. Prevalence of reticular pseudodrusen in eyes with newly presenting neovascular age-related macular degeneration. Eur J Ophthalmol. 2016;26:128–34.
Hageman GS, Mullins RF. Molecular composition of drusen as related to substructural phenotype. Mol Vis. 1999;5:28.
Hogan MJ, Alvarado J. Studies on the human macula. IV. Aging changes in Bruch’s membrane. Arch Ophthalmol. 1967;77:410–20.
Booij JC, Baas DC, Beisekeeva J, Gorgels TG, Bergen AA. The dynamic nature of Bruch’s membrane. Prog Retin Eye Res. 2010;29:1–18.
Bressler SB BN, Sarks SH, Sarks JP. Age-related macular degeneration: nonneovascular early AMD, intermediate AMD, and geographic atrophy. 4th ed. Louis: Mosby; 2006.
Gass JDM. Stereoscopic atlas of macular diseases: diagnosis and treatment. 4th ed. Louis: Mosby; 1997.
Green WR, Enger C. Age-related macular degeneration histopathologic studies. The 1992 Lorenz E. Zimmerman Lecture. Ophthalmology. 1993;100:1519–35.
Curcio CA, Millican CL. Basal linear deposit and large drusen are specific for early age-related maculopathy. Arch Ophthalmol. 1999;117:329–39.
van der Schaft TL, de Bruijn WC, Mooy CM, de Jong PT. Basal laminar deposit in the aging peripheral human retina. Graefes Arch Clin Exp. 1993;231:470–5.
Loeffler K, Lee W. Terminology of sub-RPE deposits: do we all speak the same language? Br J Ophthalmol. 1998;82:1104–5.
Sarks SH. Council Lecture. Drusen and their relationship to senile macular degeneration. Aust J Ophthalmol. 1980;8:117–30.
Wang Q, Chappell RJ, Klein R, Eisner A, Klein BE, Jensen SC, et al. Pattern of age-related maculopathy in the macular area. The Beaver Dam Eye Study. Invest Ophthalmol Vis Sci. 1996;37:2234–42.
Wang JJ, Rochtchina E, Lee AJ, Chia EM, Smith W, Cumming RG, et al. Ten-year incidence and progression of age-related maculopathy: the blue Mountains Eye Study. Ophthalmology 2007;114:92–98.
Darzins P, Mitchell P, Heller RF. Sun exposure and age-related macular degeneration. An Australian case-control study. Ophthalmology. 1997;104:770–6.
Delcourt C, Cougnard-Grégoire A, Boniol M, Carrière I, Doré JF, Delyfer MN, et al. Lifetime exposure to ambient ultraviolet radiation and the risk for cataract extraction and age-related macular degeneration: the Alienor Study. Invest Ophthalmol Vis Sci. 2014;55:7619–27.
Marin-Castano ME, Csaky KG, Cousins SW. Nonlethal oxidant injury to human retinal pigment epithelium cells causes cell membrane blebbing but decreased MMP-2 activity. Invest Ophthalmol Vis Sci. 2005;46:3331–40.
Davis MD, Gangnon RE, Lee LY, Hubbard LD, Klein B, Klein R et al. The Age-Related Eye Disease Study severity scale for age-related macular degeneration: AREDS report No. 17. Arch Ophthalmol. 2005;123:1484–98.
Curcio CA. Soft drusen in age-related macular degeneration: biology and targeting via the oil spill strategies. Invest Ophthalmol Vis Sci. 2018;59:Amd160–81.
Ugarte M, Osborne NN. Recent advances in the understanding of the role of zinc in ocular tissues. Metallomics. 2014;6:189–200.
Lengyel I, Peto T. Cure or cause: opposing roles for zinc in age-related macular degeneration. Expert Rev Ophthalmol. 2018;3:1–4.
Lengyel I, Flinn JM, Pető T, Linkous DH, Cano K, Bird AC, et al. High concentration of zinc in sub-retinal pigment epithelial deposits. Exp Eye Res. 2007;84:772–80.
van Kuijk FJ, McPherson SW, Roehrich H. Enhanced detection of sub-retinal pigment epithelial cell layer deposits in human and murine tissue: imaging zinc as a biomarker for age-related macular degeneration (An American Ophthalmological Society Thesis). Trans Am Ophthalmol Soc. 2017;115:T3.
Lengyel I, Tufail A, Al Hosaini H, Luthert P, Bird AC, Jeffery G. Association of drusen deposition with choroidal intercapillary pillars in the aging human eye. Invest Ophthalmol Vis Sci. 2004;45:2886–92.
Ebrahimi KB, Handa JT. Lipids, lipoproteins, and age-related macular degeneration. J Lipids. 2011;2011:802059.
Apte RS. Targeting tissue lipids in age-related macular degeneration. EBioMedicine. 2016;5:26–27.
Mullins RF, Schoo DP, Sohn EH, Flamme-Wiese MJ, Workamelahu G, Johnston RM, et al. The membrane attack complex in aging human choriocapillaris: relationship to macular degeneration and choroidal thinning. Am J Pathol. 2014;184:3142–53.
Wang L, Clark ME, Crossman DK, Kojima K, Messinger JD, Mobley JA, et al. Abundant lipid and protein components of drusen. PLoS ONE. 2010;5:e10329.
Fernandez-Godino R, Pierce EA, Garland DL. Extracellular matrix alterations and deposit formation in AMD. Adv Exp Med Biol. 2016;854:53–8.
Aisenbrey S, Zhang M, Bacher D, Yee J, Brunken WJ, Hunter DD. Retinal pigment epithelial cells synthesize laminins, including laminin 5, and adhere to them through alpha3- and alpha6-containing integrins. Invest Ophthalmol Vis Sci. 2006;47:5537–44.
Hageman GS, Mullins RF, Russell SR, Johnson LV, Anderson DH. Vitronectin is a constituent of ocular drusen and the vitronectin gene is expressed in human retinal pigmented epithelial cells. FASEB J. 1999;13:477–84.
Johnson LV, Ozaki S, Staples MK, Erickson PA, Anderson DH. A potential role for immune complex pathogenesis in drusen formation. Exp Eye Res. 2000;70:441–9.
Mullins RF, Russell SR, Anderson DH, Hageman GS. Drusen associated with aging and age-related macular degeneration contain proteins common to extracellular deposits associated with atherosclerosis, elastosis, amyloidosis, and dense deposit disease. FASEB J. 2000;14:835–46.
Crabb JW. The proteomics of drusen. Cold Spring Harb Perspect Med. 2014;4:a017194.
Crabb JW, Miyagi M, Gu X, Shadrach K, West KA, Sakaguchi H, et al. Drusen proteome analysis: an approach to the etiology of age-related macular degeneration. Proc Natl Acad Sci U S A. 2002;99:14682–7.
Umeda S, Suzuki MT, Okamoto H, Ono F, Mizota A, Terao K, et al. Molecular composition of drusen and possible involvement of anti-retinal autoimmunity in two different forms of macular degeneration in cynomolgus monkey (Macaca fascicularis). FASEB J. 2005;19:1683–5.
Hirata C, Nakano K, Nakamura N, Kitagawa Y, Shigeta H, Hasegawa G, et al. Advanced glycation end products induce expression of vascular endothelial growth factor by retinal Muller cells. Biochem Biophys Res Commun. 1997;236:712–5.
Pauleikhoff D, Harper CA, Marshall J, Bird AC. Aging changes in Bruch’s membrane. A histochemical and morphologic study. Ophthalmology. 1990;97:171–8.
Curcio CA, Millican CL, Bailey T, Kruth HS. Accumulation of cholesterol with age in human Bruch’s membrane. Invest Ophthalmol Vis Sci. 2001;42:265–74.
Haimovici R, Gantz DL, Rumelt S, Freddo TF, Small DM. The lipid composition of drusen, Bruch’s membrane, and sclera by hot stage polarizing light microscopy. Invest Ophthalmol Vis Sci. 2001;42:1592–9.
John Wiley and Sons. Lipid histochemistry. In: Techniques of biochemical and biophysical morphology. New York: John Wiley and Sons; 1975.
Cano M, Fijalkowski N, Kondo N, Dike S, Handa J. Advanced glycation endproduct changes to Bruch’s membrane promotes lipoprotein retention by lipoprotein lipase. Am J Pathol. 2011;179:850–9.
Rudolf M, Curcio CA. Esterified cholesterol is highly localized to Bruch’s membrane, as revealed by lipid histochemistry in wholemounts of human choroid. J Histochem Cytochem. 2009;57:731–9.
Wolter JR, Falls HF. Bilateral confluent drusen. Arch Ophthalmol. 1962;68:219–26.
Wedl C. Grundzüge der pathologischen Histologie. Vienna. 1854.
Curcio CA, Presley JB, Malek G, Medeiros NE, Avery DV, Kruth HS. Esterified and unesterified cholesterol in drusen and basal deposits of eyes with age-related maculopathy. Exp Eye Res. 2005;81:731–41.
Pikuleva IA, Curcio CA. Cholesterol in the retina: the best is yet to come. Prog Retin Eye Res. 2014;41:64–89.
Sene A, Apte RS. Eyeballing cholesterol efflux and macrophage function in disease pathogenesis. Trends Endocrinol Metab. 2014;25:107–14.
Curcio CA. Antecedents of soft drusen, the specific deposits of age-related macular degeneration, in the biology of human macula. Invest Ophthalmol Vis Sci. 2018;59:Amd182–94.
Shen J, He J, Wang F. Association of lipids with age-related macular degeneration. Discov Med. 2016;22:129–45.
Malek G, Li CM, Guidry C, Medeiros NE, Curcio CA. Apolipoprotein B in cholesterol-containing drusen and basal deposits of human eyes with age-related maculopathy. Am J Pathol. 2003;162:413–25.
Zweifel SA, Spaide RF, Curcio CA, Malek G, Imamura Y. Reticular pseudodrusen are subretinal drusenoid deposits.Ophthalmology. 2010;117:303–12.e1.
Spaide RF. Age-related choroidal atrophy. Am J Ophthalmol. 2009;147:801–10.
Curcio CA, Messinger JD, Sloan KR, McGwin G, Medeiros NE, Spaide RF. Subretinal drusenoid deposits in non-neovascular age-related macular degeneration: morphology, prevalence, topography, and biogenesis model. Retina. 2013;33:265–76.
Querques G, Querques L, Martinelli D, Massamba N, Coscas G, Soubrane G, et al. Pathologic insights from integrated imaging of reticular pseudodrusen in age-related macular degeneration. Retina. 2011;31:518–26.
Neely D, Zarubina AV, Clark ME, Huisingh CE, Jackson GR, Zhang Y, et al. Association between visual function and subretinal drusenoid deposits in normal and early age-related macular degeneration eyes. Retina. 2017;37:1329–36.
Takahashi A, Ooto S, Yamashiro K, Tamura H, Oishi A, Miyata M, et al. Pachychoroid geographic atrophy: clinical and genetic characteristics. Opthalmol Retina. 2018;2:295–305.
Hosoda Y, Yoshikawa M, Miyake M, Tabara Y, Ahn J, Woo SJ, et al. CFH and VIPR2 as susceptibility loci in choroidal thickness and pachychoroid disease central serous chorioretinopathy. Proc Natl Acad Sci USA. 2018;115:6261–6.
Baek J, Lee JH, Chung BJ, Lee K, Lee WK. Choroidal morphology under pachydrusen. Clin Exp Ophthalmol. 2019;47:498–504.
Kang SW, Lee H, Bae K, Shin JY, Kim SJ, Kim JM. Investigation of precursor lesions of polypoidal choroidal vasculopathy using contralateral eye findings. Graefes Arch Clin Exp. 2017;255:281–91.
Acknowledgements
This work is supported by the National Natural Science Foundation of China [Grant 81570850; Grant 81170859] and the Ministry of Science and Technology Foundation of China [Grant 2016YFC1305604].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, X., Sivaprasad, S. Drusen and pachydrusen: the definition, pathogenesis, and clinical significance. Eye 35, 121–133 (2021). https://doi.org/10.1038/s41433-020-01265-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-020-01265-4
This article is cited by
-
Analysis of clinical features and SS-OCT findings in patients with focal choroidal excavation
Scientific Reports (2025)
-
Pachychoroid disease: review and update
Eye (2025)
-
The intersection of mitochondria, lipids, and ferroptosis: a new avenue for dry age-related macular degeneration
Apoptosis (2025)
-
Increased macular atrophy area with photodynamic therapy over intravitreal aflibercept at 2-year follow-up of pachychoroid neovasculopathy
Japanese Journal of Ophthalmology (2025)
-
Pachychoroid pigment epitheliopathy and macular venous outflow abnormalities: the effects of venous stasis
Graefe's Archive for Clinical and Experimental Ophthalmology (2025)