Abstract
Purpose
The purpose of this study is to examine the seasonal patterns of incidence, demographic factors and microbiological profiles of infectious keratitis (IK) in Nottingham, UK.
Methods
A retrospective study of all patients who were diagnosed with IK and underwent corneal scraping during 2008–2019 at a UK tertiary referral centre. Seasonal patterns of incidence (in per 100,000 population-year), demographic factors, culture positivity rate and microbiological profiles of IK were analysed.
Results
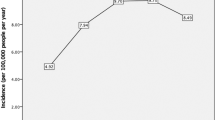
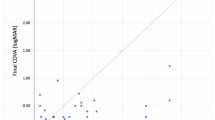
A total of 1272 IK cases were included. The overall incidence of IK was highest during summer (37.7, 95% confidence interval (CI): 31.3–44.1), followed by autumn (36.7, 95% CI: 31.0–42.4), winter (36.4, 95% CI: 32.1–40.8) and spring (30.6, 95% CI: 26.8–34.3), though not statistically significant (p = 0.14). The incidence of IK during summer increased significantly over the 12 years of study (r = 0.58, p = 0.049), but the incidence of IK in other seasons remained relatively stable throughout the study period. Significant seasonal variations were observed in patients’ age (younger age in summer) and causative organisms, including Pseudomonas aeruginosa (32.9% in summer vs. 14.8% in winter; p < 0.001) and gram-positive bacilli (16.1% in summer vs. 4.7% in winter; p = 0.014).
Conclusion
The incidence of IK in Nottingham was similar among four seasons. No temporal trend in the annual incidence of IK was observed, as reported previously, but there was a significant yearly increase in the incidence of IK during summer in Nottingham over the past decade. The association of younger age, P. aeruginosa and gram-positive bacilli infection with summer was likely attributed to contact lens wear, increased outdoor/water activity and warmer temperature conducive for microbial growth.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Ung L, Bispo PJM, Shanbhag SS, Gilmore MS, Chodosh J. The persistent dilemma of microbial keratitis: global burden, diagnosis, and antimicrobial resistance. Surv Ophthalmol. 2019;64:255–71.
Khor WB, Prajna VN, Garg P, Mehta JS, Xie L, Liu Z, et al. The Asia Cornea Society Infectious Keratitis Study: a prospective multicenter study of infectious keratitis in Asia. Am J Ophthalmol. 2018;195:161–70.
Ting DSJ, Settle C, Morgan SJ, Baylis O, Ghosh S. A 10-year analysis of microbiological profiles of microbial keratitis: the North East England Study. Eye. 2018;32:1416–7.
Austin A, Lietman T, Rose-Nussbaumer J. Update on the management of infectious keratitis. Ophthalmology. 2017;124:1678–89.
Srinivasan M, Mascarenhas J, Rajaraman R, Ravindran M, Lalitha P, Glidden DV, et al. Corticosteroids for bacterial keratitis: the Steroids for Corneal Ulcers Trial (SCUT). Arch Ophthalmol. 2012;130:143–50.
Ting DSJ, Henein C, Said DG, Dua HS. Photoactivated chromophore for infectious keratitis—Corneal cross-linking (PACK-CXL): a systematic review and meta-analysis. Ocul Surf. 2019;17:624–34.
Fernandes M, Vira D, Dey M, Tanzin T, Kumar N, Sharma S. Comparison between polymicrobial and fungal keratitis: clinical features, risk factors, and outcome. Am J Ophthalmol. 2015;160:873–81.e2.
Ting DSJ, Bignardi G, Koerner R, Irion LD, Johnson E, Morgan SJ, et al. Polymicrobial keratitis with Cryptococcus curvatus, Candida parapsilosis, and Stenotrophomonas maltophilia after penetrating keratoplasty: a rare case report with literature review. Eye Contact Lens. 2019;45:e5–10.
Shah A, Sachdev A, Coggon D, Hossain P. Geographic variations in microbial keratitis: an analysis of the peer-reviewed literature. Br J Ophthalmol. 2011;95:762–7.
Green M, Apel A, Stapleton F. A longitudinal study of trends in keratitis in Australia. Cornea. 2008;27:33–9.
Ibrahim YW, Boase DL, Cree IA. Epidemiological characteristics, predisposing factors and microbiological profiles of infectious corneal ulcers: the Portsmouth corneal ulcer study. Br J Ophthalmol. 2009;93:1319–24.
Lin CC, Lalitha P, Srinivasan M, Prajna NV, McLeod SD, Acharya NR, et al. Seasonal trends of microbial keratitis in South India. Cornea. 2012;31:1123–7.
Otri AM, Fares U, Al-Aqaba MA, Miri A, Faraj LA, Said DG, et al. Profile of sight-threatening infectious keratitis: a prospective study. Acta Ophthalmol. 2013;91:643–51.
Ni N, Nam EM, Hammersmith KM, Nagra PK, Azari AA, Leiby BE, et al. Seasonal, geographic, and antimicrobial resistance patterns in microbial keratitis: 4-year experience in eastern Pennsylvania. Cornea. 2015;34:296–302.
Gorski M, Genis A, Yushvayev S, Awwad A, Lazzaro DR. Seasonal variation in the presentation of infectious keratitis. Eye Contact Lens. 2016;42:295–7.
Walkden A, Fullwood C, Tan SZ, Au L, Armstrong M, Brahma AK, et al. Association between season, temperature and causative organism in microbial keratitis in the UK. Cornea. 2018;37:1555–60.
Ting DSJ, Ho CS, Cairns J, Elsahn A, Al-Aqaba MA, Boswell T, et al. 12-year analysis of incidence, microbiological profiles, and in vitro antimicrobial susceptibility of infectious keratitis: the Nottingham Infectious Keratitis Study. Br J Ophthalmol. 2020. https://doi.org/10.1136/bjophthalmol-2020-316128.
Chew HF, Yildiz EH, Hammersmith KM, Eagle RC Jr., Rapuano CJ, Laibson PR, et al. Clinical outcomes and prognostic factors associated with Acanthamoeba keratitis. Cornea. 2011;30:435–41.
Schober P, Boer C, Schwarte LA. Correlation coefficients: appropriate use and interpretation. Anesth Analg. 2018;126:1763–8.
Armstrong RA. When to use the Bonferroni correction. Ophthalmic Physiol Opt. 2014;34:502–8.
Martinez ME. The calendar of epidemics: seasonal cycles of infectious diseases. PLoS Pathog. 2018;14:e1007327.
Dowell SF. Seasonal variation in host susceptibility and cycles of certain infectious diseases. Emerg Infect Dis. 2001;7:369–74.
Cook SM, Glass RI, LeBaron CW, Ho MS. Global seasonality of rotavirus infections. Bull World Health Organ. 1990;68:171–7.
Koh GC, Hawthorne G, Turner AM, Kunst H, Dedicoat M. Tuberculosis incidence correlates with sunshine: an ecological 28-year time series study. PLoS ONE. 2013;8:e57752.
Suzuki T, Sutani T, Nakai H, Shirahige K, Kinoshita S. The microbiome of the meibum and ocular surface in healthy subjects. Invest Ophthalmol Vis Sci. 2020;61:18.
Zhang SD, He JN, Niu TT, Chan CY, Ren CY, Liu SS, et al. Bacteriological profile of ocular surface flora in meibomian gland dysfunction. Ocul Surf. 2017;15:242–7.
Achermann Y, Goldstein EJ, Coenye T, Shirtliff ME. Propionibacterium acnes: from commensal to opportunistic biofilm-associated implant pathogen. Clin Microbiol Rev. 2014;27:419–40.
Anthony CA, Peterson RA, Sewell DK, Polgreen LA, Simmering JE, Callaghan JJ, et al. The seasonal variability of surgical site infections in knee and hip arthroplasty. J Arthroplast. 2018;33:510–4.e1.
Chidambaram JD, Prajna NV, Palepu S, Lanjewar S, Shah M, Elakkiya S, et al. In vivo confocal microscopy cellular features of host and organism in bacterial, fungal, and Acanthamoeba keratitis. Am J Ophthalmol. 2018;190:24–33.
Ting DSJ, Said DG, Dua HS. Interface haze after Descemet stripping automated endothelial keratoplasty. JAMA Ophthalmol. 2019;137:1201–2.
Singhal N, Kumar M, Kanaujia PK, Virdi JS. MALDI-TOF mass spectrometry: an emerging technology for microbial identification and diagnosis. Front Microbiol. 2015;6:791.
Ting DSJ, McKenna M, Saidq SN, Martin J, Mudhar HS, Meeney A, et al. Arthrographis kalrae keratitis complicated by endophthalmitis: a case report with literature review. Eye Contact Lens. 2020. https://doi.org/10.1097/ICL.0000000000000713.
Ung L, Bispo PJM, Doan T, Van Gelder RN, Gilmore MS, Lietman T, et al. Clinical metagenomics for infectious corneal ulcers: rags to riches? Ocul Surf. 2020;18:1–12.
Ting DSJ, Foo VH, Yang LWY, Sia JT, Ang M, Lin H, et al. Artificial intelligence for anterior segment diseases: emerging applications in ophthalmology. Br J Ophthalmol. 2020. https://doi.org/10.1136/bjophthalmol-2019-315651.
Acknowledgements
Funding
DSJT acknowledges support from the Medical Research Council/Fight for Sight Clinical Research Fellowship (MR/T001674/1) and the Fight for Sight/John Lee, Royal College of Ophthalmologists Primer Fellowship (24CO4).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ting, D.S.J., Ho, C.S., Cairns, J. et al. Seasonal patterns of incidence, demographic factors and microbiological profiles of infectious keratitis: the Nottingham Infectious Keratitis Study. Eye 35, 2543–2549 (2021). https://doi.org/10.1038/s41433-020-01272-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-020-01272-5
This article is cited by
-
Vision rehabilitation of post-Descemet membrane endothelial keratoplasty Pseudomonas keratitis utilizing losartan ophthalmic solution and scleral contact lens: a case report
Journal of Medical Case Reports (2025)
-
Biosynthetic ε-poly-L-lysine for the treatment of extensively- and pan-drug-resistant Pseudomonas aeruginosa
npj Antimicrobials and Resistance (2025)
-
Shifting trends in bacterial keratitis in a referral center
International Ophthalmology (2025)
-
Clinical features, risk factors and outcomes of contact lens-related bacterial keratitis in Nottingham, UK: a 7-year study
Eye (2024)
-
Microbiological profile of infectious keratitis in the Newcastle and Gateshead region: a 10-year analysis
Eye (2024)