Abstract
Background
Patients with ocular hypertension (OHT) and glaucoma are increasingly reviewed in virtual clinics. As the clinician is not present during the patient’s visit it is important that measurements obtained are reliable. The aim of this study was to examine agreement between Goldmann Applanation Tonometry (GAT) intraocular pressure (IOP) measurements (obtained by ophthalmologists and ophthalmic nurses) and a newer automated tonometer—the Ocular Response Analyzer (ORA).
Methods
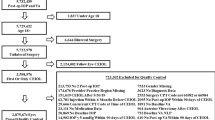
A prospective study was conducted including 116 eyes of 116 patients with glaucoma and OHT. All subjects had GAT IOP obtained by a nurse and ophthalmologist and ORA IOP by a technician. The order of testing was randomised and previous measurements were masked. Agreement was examined using Bland–Altman plots and 95% limits of agreement (LoA). Intraclass correlation coefficients (ICC) of repeat GAT and ORA measurements were calculated.
Results
Patients had a mean age of 70 ± 13 years. The 95% LoA between ophthalmologist (mean: 14.6 ± 4.3 mmHg) and nurse (mean: 15.0 ± 4.0 mmHg) GAT measurements was ±5.21 mmHg, whereas the 95% LoA between repeat ORA IOPg (mean: 13.8 ± 4.7 mmHg) was ±2.52 mmHg. There was no proportional bias. The ICC was 0.972 for repeat IOPg compared with 0.863 for repeat GAT.
Conclusions
There was only moderate agreement between GAT IOP measurements obtained by nurses working in the virtual clinic and ophthalmologists. Agreement between ORA IOP and ophthalmologists’ GAT IOP was better and ORA produced more repeatable measurements, providing evidence it may be a more reliable tool for IOP assessment in virtual clinics.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Tham Y-C, Li X, Wong TY, Quigley HA, Aung T, Cheng C-Y. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081–90.
Kotecha A, Longstaff S, Azuara-Blanco A, Kirwan JF, Morgan JE, Spencer AF, et al. Developing standards for the development of glaucoma virtual clinics using a modified Delphi approach. Br J Ophthalmol. 2018;102:531–4.
Clarke J, Puertas R, Kotecha A, Foster PJ, Barton K. Virtual clinics in glaucoma care: face-to-face versus remote decision-making. Br J Ophthalmol. 2017;101:892–5.
Kotecha A, Baldwin A, Brookes J, Foster PJ. Experiences with developing and implementing a virtual clinic for glaucoma care in an NHS setting. Clin Ophthalmol. 2015;9:1915–23.
Gunn PJG, Marks JR, Au L, Waterman H, Spry PGD, Harper RA. Acceptability and use of glaucoma virtual clinics in the UK: a national survey of clinical leads. BMJ Open Ophthalmol. 2018;3:e000127.
Court JH, Austin MW. Virtual glaucoma clinics: patient acceptance and quality of patient education compared to standard clinics. Clin Ophthalmol. 2015;9:745–9.
Wang AS, Alencar LM, Weinreb RN, Tafreshi A, Deokule S, Vizzeri G, et al. Repeatability and reproducibility of Goldmann applanation, dynamic contour, and ocular response analyzer tonometry. J Glaucoma. 2013;22:127–32.
Dielemans I, Vingerling JR, Hofman A, Grobbee DE, de Jong PT. Reliability of intraocular pressure measurement with the Goldmann applanation tonometer in epidemiological studies. Graefes Arch Clin Exp Ophthalmol. 1994;232:141–4.
Valero B, Fénolland J-R, Rosenberg R, Sendon D, Mesnard C, Sigaux M, et al. Reliability and reproducibility of introcular pressure (IOP) measurement with the Icare® Home rebound tonometer (model TA022) and comparison with Goldmann applanation tonometer in glaucoma patients. J Fr Ophtalmol. 2017;40:865–75.
Kim KN, Jeoung JW, Park KH, Yang MK, Kim DM. Comparison of the new rebound tonometer with Goldmann applanation tonometer in a clinical setting. Acta Ophthalmol. 2013;91:e392–6.
Salvetat ML, Zeppieri M, Tosoni C, Brusini P. Repeatability and accuracy of applanation resonance tonometry in healthy subjects and patients with glaucoma. Acta Ophthalmol. 2014;92:e66–73.
Maino AP, Uddin HJ, Tullo AB. A comparison of clinical performance between disposable and Goldmann tonometers. Eye. 2006;20:574–8.
Tejwani S, Dinakaran S, Joshi A, Shetty R, Sinha Roy A. A cross-sectional study to compare intraocular pressure measurement by sequential use of Goldman applanation tonometry, dynamic contour tonometry, ocular response analyzer, and Corvis ST. Indian J Ophthalmol. 2015;63:815–20.
Grolman B, Myers KJ, Lalle P. How reliable is the Goldmann tonometer as a standard? J Am Optom Assoc. 1990;61:857–62.
Rüfer F. Sources of error in Goldmann applanation tonometry. Ophthalmologe. 2011;108:546–52.
Ragan A, Cote SL, Huang JT. Disinfection of the Goldman applanation tonometer: a systematic review. Can J Ophthalmol. 2018;53:252–9.
Kaushik S, Pandav SS. Ocular response analyzer. J Curr Glaucoma Pract. 2012;6:17–9.
Reichert Technologies. Ocular Response Analyzer® G3—user’s guide English. 2018. p. 26–7. http://doclibrary.com/MSC167/PRM/16170-101-Rev-J-UG-ORAG31553.pdf.
Renier C, Zeyen T, Fieuws S, Vandenbroeck S, Stalmans I. Comparison of ocular response analyzer, dynamic contour tonometer and Goldmann applanation tonometer. Int Ophthalmol. 2010;30:651–9.
Martinez-de-la-Casa JM, Garcia-Feijoo J, Fernandez-Vidal A, Mendez-Hernandez C, Garcia-Sanchez J. Ocular response analyzer versus Goldmann applanation tonometry for intraocular pressure measurements. Investig Ophthalmol Vis Sci. 2006;47:4410–4.
Zareei A, Razeghinejad MR, Nowroozzadeh MH, Mehrabi Y, Aghazadeh-Amiri M. Intraocular pressure measurement by three different tonometers in primary congenital glaucoma. J Ophthalmic Vis Res. 2015;10:43–8.
Wasielica-Poslednik J, Politino G, Schmidtmann I, Lorenz K, Bell K, Pfeiffer N, et al. Influence of corneal opacity on intraocular pressure assessment in patients with lysosomal storage diseases. PLoS ONE. 2017;12:e0168698.
Kouchaki B, Hashemi H, Yekta A, Khabazkhoob M. Comparison of current tonometry techniques in measurement of intraocular pressure. J Curr Ophthalmol. 2017;29:92–7.
World Medical Association. World Medical Association Declaration of Helsinki. JAMA 2013;310:2191.
Kotecha A, Elkarmouty A, Ajtony C, Barton K. Interobserver agreement using Goldmann applanation tonometry and dynamic contour tonometry: comparing ophthalmologists, nurses and technicians. Br J Ophthalmol. 2016;100:854–9.
Bland J. How can I decide the sample size for a study of agreement between two methods of measurement? University of York; 2004. http://www-users.york.ac.uk/~mb55/meas/sizemeth.htm.
Ajtony C, Elkarmouty A, Barton K, Kotecha A. Applanation tonometry: interobserver and prism agreement using the reusable Goldmann applanation prism and the Tonosafe disposable prism. Br J Ophthalmol. 2016;100:848–53.
Leske MC, Heijl A, Hussein M, Bengtsson B, Hyman L, Komaroff E, et al. Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial. Arch Ophthalmol. 2003;121:48–56.
Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ, Johnson CA, et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120:714–20.
Medeiros FA, Weinreb RN. Evaluation of the influence of corneal biomechanical properties on intraocular pressure measurements using the ocular response analyzer. J Glaucoma. 2006;15:364–70.
Lascaratos G, Garway-Heath DF, Russell RA, Crabb DP, Zhu H, Hirn C, et al. Intraocular pressure (IOP) measured with the ocular response analyzer is a better predictor of glaucoma progression than Goldmann IOP in the United Kingdom Glaucoma Treatment Study (UKGTS). Investig Ophthalmol Vis Sci. 2014;55:128.
Acknowledgements
We would like to thanks all the ophthalmologists and nurses in the Princess Alexandra Eye Pavilion who agreed to participate in the study and provide Goldmann Applanation Tonometer IOP data.
Funding
AJT receives funding from a National Health Service Scotland Career Research Fellowship. The funder had no role in the study design, result analysis, conclusions or decision to submit for publication. The other authors declare no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mostafa, I., Bianchi, E., Brown, L. et al. What is the best way to measure intraocular pressure (IOP) in a virtual clinic?. Eye 35, 448–454 (2021). https://doi.org/10.1038/s41433-020-0868-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-020-0868-2
This article is cited by
-
Closed-eye intraocular pressure and eye movement monitoring via a stretchable bimodal contact lens
Microsystems & Nanoengineering (2025)
-
Smart soft contact lenses for continuous 24-hour monitoring of intraocular pressure in glaucoma care
Nature Communications (2022)
-
Audit of outcomes following attendance at the City West drive-through IOP glaucoma clinic during the COVID-19 pandemic
Irish Journal of Medical Science (1971 -) (2022)
-
Comment on: ‘What is the best way to measure intraocular pressure (IOP) in a virtual clinic?’
Eye (2021)