Abstract
Background
Ciclo plasty using high-intensity focused ultrasound (HIFU) technology acts through the selective coagulation of the ciliary body. Our aim was to evaluate the safety and efficacy profiles of 8-s probe HIFU cyclocoagulation using the EyeOP1 device.
Methods
Prospective pragmatic trial. Inclusion criteria: adult glaucoma patients with uncontrolled IOP despite optimised medical therapy, and/or intolerant to medical therapy required to achieve target IOP. Primary outcome: surgical success defined as IOP reduction from baseline >20% with final IOP ≤21 mmHg, without adding any IOP-lowering drugs, and without loss of light perception; or decreased use of IOP-lowering drugs with stable/decreased IOP, without loss of light perception. Secondary outcomes: mean IOP, intra and postoperative complications, best-corrected visual acuity (BCVA) and number of IOP-lowering drugs at each visit. Outcome data were collected preoperatively and at postoperative day 1, and months 1, 3, 6 and 12.
Results
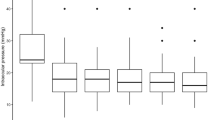
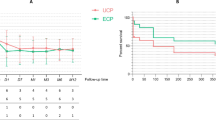
Forty-nine eyes of forty-nine patients (28 male) with a mean age of 70 ± 14 years were enroled. Pre-operative IOP was 26.9 ± 7.4 mmHg under 2.8 ± 0.9 topical medications, decreasing to 17.8 ± 6.4 mmHg under 2.3 ± 1 drugs at 12 months (p < 0.01). One-year surgical success was achieved in 71.4% of patients (IOP-reduction criteria: 59.2%; decreased use of IOP-lowering drugs: 38.8%). Eight patients were ultimately submitted to other glaucoma surgical interventions. Five patients experienced serious adverse events (loss of light perception n = 5; hypotony n = 1).
Conclusions
This innovative non-invasive technology seems to be effective in decreasing IOP and/or the number of administered drops in patients with refractory glaucoma. It seems a valuable tool to delay or preclude the need for filtering procedures in the majority of the patients.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081–90.
Blumberg D, Skaat A, Liebmann JM. Emerging risk factors for glaucoma onset and progression. Prog Brain Res. 2015;221:81–101.
Choi J, Kook MS. Systemic and ocular hemodynamic risk factors in glaucoma. Biomed Res Int. 2015;2015:141905.
Boland MV, Quigley HA. Risk factors and open-angle glaucoma: concepts and applications. J Glaucoma. 2007;16:406–18. https://doi.org/10.1097/IJG.0b013e31806540a1.
Sousa DC, Leal I, Nascimento N, Marques-Neves C, Tuulonen A, Pinto LA. Use of ocular hypotensive medications in Portugal: PEM study: a cross-sectional nationwide analysis. J Glaucoma. 2017;26:571–6.
Kolko M, Horwitz A, Thygesen J, Jeppesen J, Torp-Pedersen C. The prevalence and incidence of glaucoma in Denmark in a fifteen year period: a nationwide study. PLoS ONE. 2015;10:e0132048.
Quaranta L, Riva I, Gerardi C, Oddone F, Floriani I, Konstas AG. Quality of life in glaucoma: a review of the literature. Adv Ther. 2016;33:959–81.
Janz NK, Wren PA, Lichter PR, Musch DC, Gillespie BW, Guire KE, et al. The collaborative initial glaucoma treatment study: interim quality of life findings after initial medical or surgical treatment of glaucoma. Ophthalmology. 2001;108:1954–65.
King AJ, Fernie G, Azuara-Blanco A, Burr JM, Garway-Heath T, Sparrow JM, et al. Treatment of advanced glaucoma study: a multicentre randomised controlled trial comparing primary medical treatment with primary trabeculectomy for people with newly diagnosed advanced glaucoma—study protocol. Br J Ophthalmol. 2018;102:922–8.
Mastropasqua R, Fasanella V, Mastropasqua A, Ciancaglini M, Agnifili L. High-intensity focused ultrasound circular cyclocoagulation in glaucoma: a step forward for cyclodestruction? J Ophthalmol. 2017;2017:7136275.
De R Jr. Cryosurgery for the treatment of glaucoma. Trans Am Ophthalmol Soc. 1965;63:189–204.
Hamard P, Gayraud JM, Kopel J, Valtot F, Quesnot S, Hamard H. Treatment of refractory glaucomas by transscleral cyclophotocoagulation using semiconductor diode laser. Analysis of 50 patients followed-up over 19 months. J Fr Ophtalmol. 1997;20:125–33.
Vernon SA, Koppens JM, Menon GJ, Negi AK. Diode laser cycloablation in adult glaucoma: long-term results of a standard protocol and review of current literature. Clin Exp Ophthalmol. 2006;34:411–20.
Gazzard G, Konstantakopoulou E, Garway-Heath D, Garg A, Vickerstaff V, Hunter R, et al. Selective laser trabeculoplasty versus eye drops for first-time treatment of ocular hypertension and glaucoma (LiGHT): a multicentre randomised controlled trial. Lancet. 2019;393:1505–6.
Aptel F, Denis P, Rouland JF, Renard JP, Bron A. Multicenter clinical trial of high-intensity focused ultrasound treatment in glaucoma patients without previous filtering surgery. Acta Ophthalmol. 2016;94:e268–77.
Posarelli C, Covello G, Bendinelli A, Fogagnolo P, Nardi M, Figus M. High-intensity focused ultrasound procedure: the rise of a new noninvasive glaucoma procedure and its possible future applications. Surv Ophthalmol. 2019;64:826–834.
Lange C, Feltgen N, Junker B, Schulze-Bonsel K, Bach M. Resolving the clinical acuity categories “hand motion” and “counting fingers” using the Freiburg Visual Acuity Test (FrACT). Graefes Arch Clin Exp Ophthalmol. 2009;247:137–42.
Denis P, Aptel F, Rouland JF, Nordmann JP, Lachkar Y, Renard JP, et al. Cyclocoagulation of the ciliary bodies by high-intensity focused ultrasound: a 12-month multicenter study. Investig Ophthalmol Vis Sci. 2015;56:1089–96.
Aptel F, Dupuy C, Rouland JF. Treatment of refractory open-angle glaucoma using ultrasonic circular cyclocoagulation: a prospective case-series. Curr Med Res Opin. 2014;30:1599–605.
De Gregorio A, Pedrotti E, Stevan G, Montali M, Morselli S. Safety and efficacy of multiple cyclocoagulation of ciliary bodies by high-intensity focused ultrasound in patients with glaucoma. Graefes Arch Clin Exp Ophthalmol. 2017;255:2429–35.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Marques, R.E., Ferreira, N.P., Sousa, D.C. et al. High intensity focused ultrasound for glaucoma: 1-year results from a prospective pragmatic study. Eye 35, 484–489 (2021). https://doi.org/10.1038/s41433-020-0878-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-020-0878-0
This article is cited by
-
Ultrasonic biomicroscope-guided radiofrequency ablation of the ciliary body in a rabbit glaucoma model
Scientific Reports (2025)
-
Iris neovascularization and neurotrophic keratopathy following ultrasound cycloplasty in refractory glaucoma: case series
BMC Ophthalmology (2024)
-
Effect of high-intensity focused ultrasound (HiFU) treatment on intraocular pressure and aqueous humour dynamics: 12 -months results
Eye (2021)
-
A 2-year prospective multicenter study of ultrasound cyclo plasty for glaucoma
Scientific Reports (2021)