Abstract
Background
Little is known about the association between cataract and multimorbidity. Therefore, the aim of the present study was to examine the relationship between cataract and chronic conditions and multimorbidity in a large representative sample of Spanish adults.
Methods
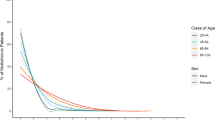
This study used data from the Spanish National Health Survey 2017, a cross-sectional sample of 23,089 adults aged ≥15 years from Spain [54.1% female; mean (standard deviation) age 53.4 (18.9) years]. Cataract and 30 other physical and mental chronic conditions were self-reported. Multimorbidity was defined as the presence of at least two physical and/or mental chronic conditions (excluding cataract). Control variables included sex, age, marital status, education, smoking, and alcohol consumption. Multivariable logistic and negative binomial regression analyzes were conducted to assess associations.
Results
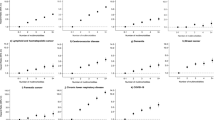
The prevalence of cataract and multimorbidity was 12.5% and 56.5%, respectively. All chronic conditions were significantly more frequent in individuals with than in those without cataract. Overall, there was a positive relationship between cataract and multimorbidity [odds ratio (OR) = 2.77; 95% confidence interval (CI): 2.39–3.21]. In addition, cataract was significantly associated with the number of chronic conditions in the whole population [incidence rate ratio (IRR) = 1.34; 95% CI: 1.29–1.38].
Conclusions
Cataract is positively associated with chronic conditions and multimorbidity in adults. Interventions specifically designed for those with cataract to reduce or manage co-occurring chronic conditions and multimorbidity are urgently required.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Mayo Clinic. Cataracts. https://www.mayoclinic.org/diseases-conditions/cataracts/symptoms-causes/syc-20353790. Accesed 5 Dec 2019.
World Health Organization. Priority eye diseases. https://www.who.int/blindness/causes/priority/en/index1.html. Accesed 5 Dec 2019.
Lou L, Ye X, Xu P, Wang J, Xu Y, Jin K, et al. Association of sex with the global burden of cataract. JAMA Ophthalmol. 2018;136:116–21. https://doi.org/10.1001/jamaophthalmol.2017.5668.
World Health Organization. Blindness and vision impairment: key activities. https://www.who.int/blindness/key-activities/en/. Accesed 5 Dec 2019.
Mercer S, Furler J, Moffat K, Fischbacher-Smith D, Sanci L, editors. Multimorbidity: technical series on safer primary care. Geneva: World Health Organization; 2016.
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380:37–43. https://doi.org/10.1016/S0140-6736(12)60240-2.
Gijsen R, Hoeymans N, Schellevis FG, Ruwaard D, Satariano WA, Van den Bos GA. Causes and consequences of comorbidity: a review. J Clin Epidemiol. 2001;54:661–74.
Kadam UT, Croft PR, North Staffordshire GP Consortium Group. Clinical multimorbidity and physical function in older adults: a record and health status linkage study in general practice. Fam Pract. 2007;24:412–9. https://doi.org/10.1093/fampra/cmm049.
Salisbury C, Johnson L, Purdy S, Valderas JM, Montgomery AA. Epidemiology and impact of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract. 2011;61:e12–21. https://doi.org/10.3399/bjgp11X548929.
Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162:2269–76. https://doi.org/10.1001/archinte.162.20.2269.
Violan C, Foguet-Boreu Q, Flores-Mateo G, Salisbury C, Blom J, Freitag M, et al. Prevalence, determinants and patterns of multimorbidity in primary care: a systematic review of observational studies. PLoS ONE. 2014;9:e102149. https://doi.org/10.1371/journal.pone.0102149.
Alimohammadian M, Majidi A, Yaseri M, Ahmadi B, Islami F, Derakhshan M, et al. Multimorbidity as an important issue among women: results of a gender difference investigation in a large population-based cross-sectional study in West Asia. BMJ Open. 2017;7:e013548. https://doi.org/10.1136/bmjopen-2016-013548.
Garin N, Olaya B, Lara E, Moneta MV, Miret M, Ayuso-Mateos JL, et al. Visual impairment and multimorbidity in a representative sample of the Spanish population. BMC Public Health. 2014;14:815. https://doi.org/10.1186/1471-2458-14-815.
Crews JE, Chou CF, Sekar S, Saaddine JB. The prevalence of chronic conditions and poor health among people with and without vision impairment, aged ≥ 65 years, 2010–2014. Am J Ophthalmol. 2017;182:18–30. https://doi.org/10.1016/j.ajo.2017.06.038.
Smith L, Timmis MA, Pardhan S, Latham K, Johnstone J, Hamer M. Physical inactivity in relation to self-rated eyesight: cross-sectional analysis from the English Longitudinal Study of Ageing. BMJ Open Ophthalmol. 2017;1:e000046. https://doi.org/10.1136/bmjophth-2016-000046.
Pham TQ, Wang JJ, Rochtchina E, Maloof A, Mitchell P. Systemic and ocular comorbidity of cataract surgical patients in a western Sydney public hospital. Clin Exp Ophthalmol. 2004;32:383–7. https://doi.org/10.1111/j.1442-9071.2004.00842.x.
Ministerio de Sanidad, Servicios Sociales e Igualdad & Instituto Nacional de Estadística. Spanish National Health Survey 2017: methodology. https://www.mscbs.gob.es/estadEstudios/estadisticas/encuestaNacional/encuestaNac2017/ENSE17_Metodologia.pdf. Accesed 5 Dec 2019.
Bergmann MM, Byers T, Freedman DS, Mokdad A. Validity of self-reported diagnoses leading to hospitalization: a comparison of self-reports with hospital records in a prospective study of American adults. Am J Epidemiol. 1998;147:969–77. https://doi.org/10.1093/oxfordjournals.aje.a009387.
Martin LM, Leff M, Calonge N, Garrett C, Nelson DE. Validation of self-reported chronic conditions and health services in a managed care population. Am J Prev Med. 2000;18:215–8. https://doi.org/10.1016/S0749-3797(99)00158-0.
Yawson AE, Ackuaku-Dogbe EM, Seneadza NA, Mensah G, Minicuci N, Naidoo N, et al. Self-reported cataracts in older adults in Ghana: sociodemographic and health related factors. BMC Public Health. 2014;14:1–8. https://doi.org/10.1186/1471-2458-14-949.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2018. https://www.R-project.org/. Accesed 5 Dec 2019.
Sayin N, Kara N, Pekel G. Ocular complications of diabetes mellitus. World J Diabetes. 2015;6:92–108. https://doi.org/10.4239/wjd.v6.i1.92.
López-Sánchez GF, Grabovac I, Pizzol D, Yang L, Smith L. The association between difficulty seeing and physical activity among 17,777 adults residing in Spain. Int J Environ Res Public Health. 2019;16:e4267. https://doi.org/10.3390/ijerph16214267.
Smith L, Jackson SE, Pardhan S, López-Sánchez GF, Hu L, Cao C, et al. Visual impairment and objectively measured physical activity and sedentary behaviour in US adolescents and adults: a cross-sectional study. BMJ Open. 2019;9:e027267. https://doi.org/10.1136/bmjopen-2018-027267.
Rao TS, Asha MR, Ramesh BN, Rao KJ. Understanding nutrition, depression and mental illnesses. Indian J Psychiatry. 2008;50:77–82. https://doi.org/10.4103/0019-5545.42391.
Hu FB. Protein, body weight, and cardiovascular health. Am J Clin Nutr. 2005;82:242S–7S. https://doi.org/10.1093/ajcn/82.1.242S.
Cumming RG, Mitchell P, Smith W. Diet and cataract: the blue mountains eye study. Ophthalmology. 2000;107:450–6. https://doi.org/10.1016/s0161-6420(99)00024-x.
Zhu M, Yu J, Zhang J, Yan Q, Liu Y. Evaluating vision-related quality of life in preoperative age-related cataract patients and analyzing its influencing factors in China: a cross-sectional study. BMC Ophthalmol. 2015;15:160. https://doi.org/10.1186/s12886-015-0150-8.
Aminisani N, Nikbakht H, Jafarabadi MA, Shamshirgaran SMDepression. anxiety, and health related quality of life among colorectal cancer survivors. J Gastrointest Oncol. 2017;8:81–8. https://doi.org/10.21037/jgo.2017.01.12.
Van Jaarsveld CH, Sanderman R, Ranchor AV, Ormel J, Van Veldhuisen DJ, Kempen GI. Gender-specific changes in quality of life following cardiovascular disease: a prospective study. J Clin Epidemiol. 2002;55:1105–12. https://doi.org/10.1016/s0895-4356(02)00506-1.
Öztürk A, Şimşek TT, Yümin ET, Sertel M, Yümin M. The relationship between physical, functional capacity and quality of life (QoL) among elderly people with a chronic disease. Arch Gerontol Geriatr. 2011;53:278–83. https://doi.org/10.1016/j.archger.2010.12.011.
Coyle CE, Steinman BA, Chen J. Visual acuity and self-reported vision status: their associations with social isolation in older adults. J Aging Health. 2017;29:128–48. https://doi.org/10.1177/0898264315624909.
Brunes A, Hansen MB, Heir T. Loneliness among adults with visual impairment: prevalence, associated factors, and relationship to life satisfaction. Health Qual Life Outcomes. 2019;17:24. https://doi.org/10.1186/s12955-019-1096-y.
Singer L, Green M, Rowe F, Ben-Shlomo Y, Morrissey K. Social determinants of multimorbidity and multiple functional limitations among the ageing population of England, 2002–2015. SSM Popul Health. 2019;8:100413. https://doi.org/10.1016/j.ssmph.2019.100413.
Jessen MAB, Pallesen AVJ, Kriegbaum M, Kristiansen M. The association between loneliness and health—a survey-based study among middle-aged and older adults in Denmark. Aging Ment Health. 2018;22:1338–43. https://doi.org/10.1080/13607863.2017.1348480.
Palagyi A, Rogers K, Meuleners L, McCluskey P, White A, Ng JQ, et al. Depressive symptoms in older adults awaiting cataract surgery. Clin Exp Ophthalmol. 2016;44:789–96. https://doi.org/10.1111/ceo.12800.
Krishnaiah S, Ramanathan RV. Impact of blindness due to cataract in elderly fallers: findings from a cross-sectional study in Andhra Pradesh, South India. BMC Res Notes. 2018;11:773. https://doi.org/10.1186/s13104-018-3883-7.
Terroso M, Rosa N, Marques AT, Simoes R. Physical consequences of falls in the elderly: a literature review from 1995 to 2010. Eur Rev Aging Phys Act. 2014;11:51–9. https://doi.org/10.1007/s11556-013-0134-8.
Hajian-Tilaki K, Heidari B, Hajian-Tilaki A. Are gender differences in health-related quality of life attributable to sociodemographic characteristics and chronic disease conditions in elderly people? Int J Prev Med. 2017;8:95. https://doi.org/10.4103/ijpvm.IJPVM_197_16.
American Optometric Association. Nutrition and cataracts. https://www.aoa.org/patients-and-public/caring-for-your-vision/nutrition/nutrition-and-cataracts. Accesed 21 Jan 2020.
Funding
GFL-S is funded by the Seneca Foundation—Agency for Science and Technology of the Region of Murcia, Spain (20390/PD/17). AK’s work is supported by the PI15/00862 project, integrated into the National R + D + I and funded by the ISCIII—General Branch Evaluation and Promotion of Health Research—and the European Regional Development Fund (ERDF-FEDER). These funders had no role in the study design, collection, analysis, and interpretation of the data; writing of the report; and the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
LJ contributed to the design of the study, managed the literature searches, undertook the statistical analysis, and contributed to the correction of the paper. GFL-S contributed to the design of the study, managed the literature searches, wrote the first draft of the paper, and contributed to the correction of the paper. LY, JMH, JIlS, NV, PS, TG, and AK contributed to the design of the study and the correction of the paper. LS contributed to the design of the study, managed the literature searches, wrote the first draft of the paper, and contributed to the correction of the paper. All authors contributed to and have approved the final paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jacob, L., López-Sánchez, G.F., Yang, L. et al. Associations between cataract and multimorbidity: a cross-sectional study of 23,089 adults from Spain. Eye 35, 791–798 (2021). https://doi.org/10.1038/s41433-020-0962-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-020-0962-5
This article is cited by
-
What makes a good survey?
Eye (2023)