Abstract
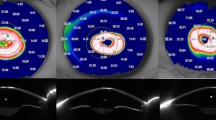
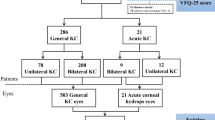
Our aim is to review current and significant articles on contact lens wear in keratoconus patients. A comprehensive literature search of PubMed was performed for the following topics on contact lens wear in keratoconus patients: (1) characteristics of contact lens wearers, (2) safety and efficacy, (3) complications, (4) fitting techniques, (5) contact lens wear after procedures/surgeries, (6) patient satisfaction. A total of 104 studies were finally selected and reviewed. Gas permeable (GP) lens wear provided significantly better vision than glasses. Special cone design lenses had better patient comfort levels though there was no difference in best corrected visual acuity among the GP lenses. Soft lenses showed good efficacy for the treatment of mild-to-moderate keratoconus with newer designs improving visual performance such as customised hydrogel and novel pinhole lenses. Scleral and hybrid lenses provide good visual acuity and comfort for keratoconic patients previously intolerant to RGP lenses. RGP lens wear post-cross linking (CXL) is relatively well-tolerated. Contact lenses may still be required post intrastromal corneal ring procedures and post keratoplasty. Scheimpflug imaging and anterior segment optical coherent tomography (ASOCT) are useful in contact lens fitting. Computerized contact lens fitting techniques could reduce the chair time of lens fitting as well as improve comfort and visual performance. Contact lenses play an important role in the visual rehabilitation of keratoconus patients. New contact lens designs and materials have significantly expanded the available fitting options for keratoconus patients. Imaging technology can be utilized to guide contact lens fitting.
摘要
当前关于接触镜治疗圆锥角膜的观点
本文旨在对圆锥角膜患者佩戴角膜接触镜的重要文献进行回顾。我们于PubMed进行了全面的文献检索, 聚焦于圆锥角膜患者佩戴接触镜的问题: (1) 接触镜佩戴者的特点 (2) 安全性和有效性 (3) 并发症 (4) 适配技术 (5) 手术后的接触镜的佩戴 (6) 患者满意度。文中最终纳入并回顾了104项研究。
佩戴透气性 (Gas permeable, GP) 镜片比眼镜具有更好的视野。特殊设计的锥形镜片使病人拥有更佳的舒适度, 尽管最佳矫正视力与GP镜片之间并没有差异。软性镜片在治疗轻中度圆锥角膜方面显示出良好疗效, 新设计的如定制水凝胶和新型针孔镜片改善了视觉性能。巩膜和混合镜片为不能耐受RGP镜片的圆锥角膜患者提供了良好的视力和舒适度。佩戴RGP镜片后交联 (post-cross linking, CXL) 相对耐受性较好。角膜基质环术和角膜成形术后仍需佩戴接触镜。
Scheimpflug成像和眼前节光学相干断层扫描 (anterior segment optical coherent tomography, ASOCT) 有助于接触镜的适配。计算机化的接触镜适配技术可以减少镜片配戴的占用时间, 提高舒适度和视觉性能。
角膜接触镜在圆锥角膜患者的视觉康复中起着重要作用。新接触镜的设计和材料极大地扩展了圆锥角膜患者可用的适配选择。成像技术的利用有助于指导接触镜的配戴。
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42:297–319.
Kennedy RH, Bourne WM, Dyer JA. A 48-year clinical and epidemiologic study of keratoconus. Am J Ophthalmol. 1986;101:267–73.
Godefrooij DA, de Wit GA, Uiterwaal CS, Imhof SM, Wisse RP. Age-specific incidence and prevalence of keratoconus: a nationwide registration study. Am J Ophthalmol. 2017;175:169–72.
Gordon-Shaag A, Millodot M, Shneor E, Liu Y. The genetic and environmental factors for keratoconus. Biomed Res Int. 2015;2015:795738.
Kymes SM, Walline JJ, Zadnik K, Gordon MO. Collaborative longitudinal evaluation of keratoconus study G. Quality of life in keratoconus. Am J Ophthalmol. 2004;138:527–35.
Garcia-Ferrer FJ, Akpek EK, Amescua G, Farid M, Lin A, Rhee MK, et al. Corneal ectasia preferred practice pattern(R). Ophthalmology. 2019;126:P170–P215.
Mannis MJ, Zadnik K. Contact lens fitting in keratoconus. CLAO J. 1989;15:282–9.
Gomes JA, Tan D, Rapuano CJ, Belin MW, Ambrosio R Jr., Guell JL, et al. Global consensus on keratoconus and ectatic diseases. Cornea. 2015;34:359–69.
Weed KH, Macewen CJ, McGhee CN. The Dundee University Scottish Keratoconus Study II: a prospective study of optical and surgical correction. Ophthalmic Physiol Opt. 2007;27:561–7.
Zadnik K, Barr JT, Edrington TB, Everett DF, Jameson M, McMahon TT, et al. Baseline findings in the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study. Investig Ophthalmol Vis Sci. 1998;39:2537–46.
Wagner H, Barr JT, Zadnik K. Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study: methods and findings to date. Cont Lens Anterior Eye. 2007;30:223–32.
Lim N, Vogt U. Characteristics and functional outcomes of 130 patients with keratoconus attending a specialist contact lens clinic. Eye. 2002;16:54–59.
Fatima T, Acharya MC, Mathur U, Barua P. Demographic profile and visual rehabilitation of patients with keratoconus attending contact lens clinic at a tertiary eye care centre. Cont Lens Anterior Eye. 2010;33:19–22.
Shneor E, Millodot M, Blumberg S, Ortenberg I, Behrman S, Gordon-Shaag A. Characteristics of 244 patients with keratoconus seen in an optometric contact lens practice. Clin Exp Optom. 2013;96:219–24.
Wei RH, Khor WB, Lim L, Tan DT. Contact lens characteristics and contrast sensitivity of patients with keratoconus. Eye Contact Lens. 2011;37:307–11.
Szczotka LB, Barr JT, Zadnik K. A summary of the findings from the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study. CLEK Study Group. Optometry. 2001;72:574–84.
Bilgin LK, Yilmaz S, Araz B, Yuksel SB, Sezen T. 30 years of contact lens prescribing for keratoconic patients in Turkey. Cont Lens Anterior Eye. 2009;32:16–21.
Pullum KW, Whiting MA, Buckley RJ. Scleral contact lenses: the expanding role. Cornea. 2005;24:269–77.
Gupta R, Sinha R, Singh P, Sharma N, Tandon R, Titiyal JS. Rose-K versus Soper contact lens in keratoconus: a randomized comparative trial. Middle East Afr J Ophthalmol. 2014;21:50–55.
Kazanci B, Ozek D, Anayol A, Balikci A, Ileri D, Yilmazbas P. Applications of different types of gas-permeable contact lenses in keratoconus and their visual results. Eur J Ophthalmol. 2014;24:835–41.
Nilagiri VK, Metlapally S, Kalaiselvan P, Schor CM, Bharadwaj SR. LogMAR and stereoacuity in keratoconus corrected with spectacles and rigid gas-permeable contact lenses. Optom Vis Sci. 2018;95:391–8.
Fernandez-Velazquez FJ. Kerasoft IC compared to Rose-K in the management of corneal ectasias. Cont Lens Anterior Eye. 2012;35:175–9.
Betts AM, Mitchell GL, Zadnik K. Visual performance and comfort with the Rose K lens for keratoconus. Optom Vis Sci. 2002;79:493–501.
Levit A, Benwell M, Evans BJW. Randomised controlled trial of corneal vs. scleral rigid gas permeable contact lenses for keratoconus and other ectatic corneal disorders. Cont Lens Anterior Eye. 2020;S1367-0484(19)30268-1.
Hassani M, Jafarzadehpur E, Mirzajani A, Yekta A, Khabazkhoob M. A comparison of the visual acuity outcome between Clearkone and RGP lenses. J Curr Ophthalmol. 2018;30:85–86.
Carracedo G, Gonzalez-Meijome JM, Lopes-Ferreira D, Carballo J, Batres L. Clinical performance of a new hybrid contact lens for keratoconus. Eye Contact Lens. 2014;40:2–6.
Hashemi H, Shaygan N, Asgari S, Rezvan F, Asgari S. ClearKone-Synergeyes or rigid gas-permeable contact lens in keratoconic patients: a clinical decision. Eye Contact Lens. 2014;40:95–98.
Pilskalns B, Fink BA, Hill RM. Oxygen demands with hybrid contact lenses. Optom Vis Sci. 2007;84:334–42.
Sultan P, Dogan C, Iskeleli G. A retrospective analysis of vision correction and safety in keratoconus patients wearing Toris K soft contact lenses. Int Ophthalmol. 2016;36:799–805.
Katsoulos C, Karageorgiadis L, Vasileiou N, Mousafeiropoulos T, Asimellis G. Customized hydrogel contact lenses for keratoconus incorporating correction for vertical coma aberration. Ophthalmic Physiol Opt. 2009;29:321–9.
Kalikivayi L, Ajitha Vilasendran J, Chettupuzha Lonappan A, Cherian Jacob S, Kalikivayi V. A novel method in correcting aberropia using pin hole soft contact lenses: a case report. Cont Lens Anterior Eye. 2018;42:334–8.
Lunardi LH, Arroyo D, Andrade Sobrinho MV, Lipener C, Rosa JM. Descriptive analysis of the type and design of contact lenses fitted according to keratoconus severity and morphology. Arq Bras Oftalmol. 2016;79:82–84.
Szczotka-Flynn LB, Patel S. Menicon Z rigid gas permeable lenses for keratoconus and irregular corneas: a retrospective case series. Eye Contact Lens. 2008;34:254–60.
Kang YS, Park YK, Lee JS, Lee SU, Shin JH, Han YS, et al. The effect of the YK lens in keratoconus. Ophthalmic Physiol Opt. 2010;30:267–73.
Lee JL, Kim MK. Clinical performance and fitting characteristics with a multicurve lens for keratoconus. Eye Contact Lens. 2004;30:20–24.
van der Worp E. A guide to scleral lens fitting. 2nd ed. Books and Monographs. United States of America: Pacific University Common Knowledge; 2015.
Romero-Jimenez M, Flores-Rodriguez P. Utility of a semi-scleral contact lens design in the management of the irregular cornea. Cont Lens Anterior Eye. 2013;36:146–50.
Looi AL, Lim L, Tan DT. Visual rehabilitation with new-age rigid gas-permeable scleral contact lenses—a case series. Ann Acad Med Singap. 2002;31:234–7.
Baran I, Bradley JA, Alipour F, Rosenthal P, Le HG, Jacobs DS. PROSE treatment of corneal ectasia. Cont Lens Anterior Eye. 2012;35:222–7.
Pecego M, Barnett M, Mannis MJ, Durbin-Johnson B. Jupiter Scleral Lenses: the UC Davis Eye Center experience. Eye Contact Lens. 2012;38:179–82.
Kim S, Lee JS, Park YK, Lee SU, Park YM, Lee JH, et al. Fitting miniscleral contact lenses in Korean patients with keratoconus. Clin Exp Optom. 2017;100:375–9.
Visser ES, Van der Linden BJ, Otten HM, Van der Lelij A, Visser R. Medical applications and outcomes of bitangential scleral lenses. Optom Vis Sci. 2013;90:1078–85.
Otten HM, van der Linden B, Visser ES. Clinical performance of a new bitangential mini-scleral Lens. Optom Vis Sci. 2018;95:515–22.
Koppen C, Kreps EO, Anthonissen L, Van Hoey M, Dhubhghaill SN, Vermeulen L. Scleral Lenses reduce the need for corneal transplants in severe keratoconus. Am J Ophthalmol. 2018;185:43–47.
Ozkurt Y, Oral Y, Karaman A, Ozgur O, Dogan OK. A retrospective case series: use of SoftPerm contact lenses in patients with keratoconus. Eye Contact Lens. 2007;33:103–5.
Unlu M, Yuksel E, Bilgihan K. Effect of corneal cross-linking on contact lens tolerance in keratoconus. Clin Exp Optom. 2017;100:369–74.
Sehra SV, Titiyal JS, Sharma N, Tandon R, Sinha R. Change in corneal microstructure with rigid gas permeable contact lens use following collagen cross-linking: an in vivo confocal microscopy study. Br J Ophthalmol. 2014;98:442–7.
Visser ES, Soeters N, Tahzib NG. Scleral lens tolerance after corneal cross-linking for keratoconus. Optom Vis Sci. 2015;92:318–23.
Singh K, Bhattacharyya M, Arora R, Dangda S, Mutreja A. Alterations in contact lens fitting parameters following cross-linking in keratoconus patients of Indian ethnicity. Int Ophthalmol. 2018;38:1521–30.
Serramito-Blanco M, Carpena-Torres C, Carballo J, Pinero D, Lipson M, Carracedo G. Anterior corneal curvature and aberration changes after scleral lens wear in keratoconus patients with and without ring segments. Eye Contact Lens. 2018;45:141–8.
Fernandez-Velazquez FJ, Fernandez-Fidalgo MJ. Feasibility of custom-made hydrogel contact lenses in keratoconus with previous implantation of intracorneal ring segments. Cont Lens Anterior Eye. 2015;38:351–6.
Carracedo G, Canales J, Gonzalez P, Recchioni A, Carpena-Torres C, Carballo-Alvarez J. The effect of soft contact lens thickness in visual function after intracorneal ring segments surgery. Cont Lens Anterior Eye. 2018;41:180–6.
Montalt JC, Porcar E, Espana-Gregori E, Peris-Martinez C. Visual quality with corneo-scleral contact lenses after intracorneal ring segment (ICRS) implantation for keratoconus management. Cont Lens Anterior Eye. 2019;42:111–6.
Rocha GA, Miziara PO, Castro AC, Rocha AA. Visual rehabilitation using mini-scleral contact lenses after penetrating keratoplasty. Arq Bras Oftalmol. 2017;80:17–20.
Barnett M, Lien V, Li JY, Durbin-Johnson B, Mannis MJ. Use of scleral lenses and miniscleral lenses after penetrating keratoplasty. Eye Contact Lens. 2016;42:185–9.
Geerards AJ, Vreugdenhil W, Khazen A. Incidence of rigid gas-permeable contact lens wear after keratoplasty for keratoconus. Eye Contact Lens. 2006;32:207–10.
Edrington TB, Gundel RE, Libassi DP, Wagner H, Pierce GE, Walline JJ, et al. Variables affecting rigid contact lens comfort in the collaborative longitudinal evaluation of keratoconus (CLEK) study. Optom Vis Sci. 2004;81:182–8.
Wu Y, Tan Q, Zhang W, Wang J, Yang B, Ma W, et al. Rigid gas-permeable contact lens related life quality in keratoconic patients with different grades of severity. Clin Exp Optom. 2015;98:150–4.
Erdurmus M, Yildiz EH, Abdalla YF, Hammersmith KM, Rapuano CJ, Cohen EJ. Contact lens related quality of life in patients with keratoconus. Eye Contact Lens. 2009;35:123–7.
Yildiz EH, Erdurmus M, Elibol ES, Acar B, Vural ET. Contact lens impact on quality of life in keratoconus patients: rigid gas permeable versus soft silicone-hydrogel keratoconus lenses. Int J Ophthalmol. 2015;8:1074–7.
Bergmanson JP, Walker MK, Johnson LA. Assessing scleral contact lens satisfaction in a keratoconus population. Optom Vis Sci. 2016;93:855–60.
Kandel H, Pesudovs K, Watson SL. Measurement of quality of life in keratoconus. Cornea. 2020;39:386–93.
Niederer RL, Perumal D, Sherwin T, McGhee CN. Laser scanning in vivo confocal microscopy reveals reduced innervation and reduction in cell density in all layers of the keratoconic cornea. Investig Ophthalmol Vis Sci. 2008;49:2964–70.
Weed KH, MacEwen CJ, Cox A, McGhee CN. Quantitative analysis of corneal microstructure in keratoconus utilising in vivo confocal microscopy. Eye. 2007;21:614–23.
Mocan MC, Yilmaz PT, Irkec M, Orhan M. In vivo confocal microscopy for the evaluation of corneal microstructure in keratoconus. Curr Eye Res. 2008;33:933–9.
Bitirgen G, Ozkagnici A, Malik RA, Oltulu R. Evaluation of contact lens-induced changes in keratoconic corneas using in vivo confocal microscopy. Invest Ophthalmol Vis Sci. 2013;54:5385–91.
Yeniad B, Yilmaz S, Bilgin LK. Evaluation of the microstructure of cornea by in vivo confocal microscopy in contact lens wearing and non-contact lens wearing keratoconus patients. Cont Lens Anterior Eye. 2010;33:167–70.
Patel DV, Ku JY, Johnson R, McGhee CN. Laser scanning in vivo confocal microscopy and quantitative aesthesiometry reveal decreased corneal innervation and sensation in keratoconus. Eye. 2009;23:586–92.
Erie JC, Patel SV, McLaren JW, Nau CB, Hodge DO, Bourne WM. Keratocyte density in keratoconus. A confocal microscopy study(a). Am J Ophthalmol. 2002;134:689–95.
Edmonds CR, Wung SF, Husz MJ, Pemberton B. Corneal endothelial cell count in keratoconus patients after contact lens wear. Eye Contact Lens. 2004;30:54–58.
Hollingsworth JG, Efron N, Tullo AB. In vivo corneal confocal microscopy in keratoconus. Ophthalmic Physiol Opt. 2005;25:254–60.
Acar BT, Vural ET, Acar S. Effects of contact lenses on the ocular surface in patients with keratoconus: piggyback versus ClearKone hybrid lenses. Eye Contact Lens. 2012;38:43–48.
Dogan C, Hagverdiyeva S, Mergen B, Iskeleli G. Effect of the rigid gas-permeable contact lens use on the endothelial cells in patients with keratoconus. Eye Contact Lens. 2018;44(Suppl 2):S314–S317.
Owens H, Watters G, Gamble G. Effect of softperm lens wear on corneal thickness and topography: a comparison between keratoconic and normal corneae. CLAO J. 2002;28:83–87.
Fernandez-Velazquez FJ. Severe epithelial edema in Clearkone SynergEyes contact lens wear for keratoconus. Eye Contact Lens. 2011;37:381–5.
Dogru M, Karakaya H, Ozcetin H, Erturk H, Yucel A, Ozmen A, et al. Tear function and ocular surface changes in keratoconus. Ophthalmology. 2003;110:1110–8.
Cho KJ, Mok JW, Choi MY, Kim JY, Joo CK. Changes in corneal sensation and ocular surface in patients with asymmetrical keratoconus. Cornea. 2013;32:205–10.
Carracedo G, Recchioni A, Alejandre-Alba N, Martin-Gil A, Crooke A, Morote IJ, et al. Signs and symptoms of dry eye in keratoconus patients: a pilot study. Curr Eye Res. 2015;40:1088–94.
Carracedo G, Gonzalez-Meijome JM, Martin-Gil A, Carballo J, Pintor J. The influence of rigid gas permeable lens wear on the concentrations of dinucleotides in tears and the effect on dry eye signs and symptoms in keratoconus. Cont Lens Anterior Eye. 2016;39:375–9.
Moon JW, Shin KC, Lee HJ, Wee WR, Lee JH, Kim MK. The effect of contact lens wear on the ocular surface changes in keratoconus. Eye Contact Lens. 2006;32:96–101.
Carracedo G, Blanco MS, Martin-Gil A, Zicheng W, Alvarez JC, Pintor J. Short-term effect of scleral lens on the dry eye biomarkers in keratoconus. Optom Vis Sci. 2016;93:150–7.
McMonnies CW. Mechanisms of rubbing-related corneal trauma in keratoconus. Cornea. 2009;28:607–15.
Yeniad B, Alparslan N, Akarcay K. Eye rubbing as an apparent cause of recurrent keratoconus. Cornea. 2009;28:477–9.
Stapleton F, Keay L, Edwards K, Naduvilath T, Dart JK, Brian G, et al. The incidence of contact lens-related microbial keratitis in Australia. Ophthalmology. 2008;115:1655–62.
Sticca MP, Carrijo-Carvalho LC, Silva IMB, Vieira LA, Souza LB, Junior RB, et al. Acanthamoeba keratitis in patients wearing scleral contact lenses. Cont Lens Anterior Eye. 2018;41:307–10.
Bruce AS, Nguyen LM. Acute red eye (non-ulcerative keratitis) associated with mini-scleral contact lens wear for keratoconus. Clin Exp Optom. 2013;96:245–8.
Zadnik K, Barr JT, Steger-May K, Edrington TB, McMahon TT, Gordon MO, et al. Comparison of flat and steep rigid contact lens fitting methods in keratoconus. Optom Vis Sci. 2005;82:1014–21.
Romero-Jimenez M, Santodomingo-Rubido J, Gonzalez-Meijome JM. An assessment of the optimal lens fit rate in keratoconus subjects using three-point-touch and apical touch fitting approaches with the rose K2 lens. Eye Contact Lens. 2013;39:269–72.
Sorbara L, Dalton K. The use of video-keratoscopy in predicting contact lens parameters for keratoconic fitting. Cont Lens Anterior Eye. 2010;33:112–8.
Ramdas WD, Vervaet CJ, Bleyen I. Corneal topography for pancorneal toric edge rigid gas-permeable contact lens fitting in patients with keratoconus, and differences in age and gender. Cont Lens Anterior Eye. 2014;37:20–25.
Mandathara Sudharman P, Rathi V, Dumapati S. Rose K lenses for keratoconus—an Indian experience. Eye Contact Lens. 2010;36:220–2.
Weber SL, Ambrosio R Jr., Lipener C, Coral-Ghanem C, Hofling-Lima AL. The use of ocular anatomical measurements using a rotating Scheimpflug camera to assist in the Esclera(R) scleral contact lens fitting process. Cont Lens Anterior Eye. 2016;39:148–53.
Downie LE. Predictive value of corneal topography for ClearKone hybrid contact lenses. Optom Vis Sci. 2013;90:e191–197.
Ortiz-Toquero S, Rodriguez G, de Juan V, Martin R. New web-based algorithm to improve rigid gas permeable contact lens fitting in keratoconus. Cont Lens Anterior Eye. 2017;40:143–50.
Mandathara PS, Fatima M, Taureen S, Dumpati S, Ali MH, Rathi V. RGP contact lens fitting in keratoconus using FITSCAN technology. Cont Lens Anterior Eye. 2013;36:126–9.
Bhatoa NS, Hau S, Ehrlich DP. A comparison of a topography-based rigid gas permeable contact lens design with a conventionally fitted lens in patients with keratoconus. Cont Lens Anterior Eye. 2010;33:128–35.
Marsack JD, Ravikumar A, Nguyen C, Ticak A, Koenig DE, Elswick JD, et al. Wavefront-guided scleral lens correction in keratoconus. Optom Vis Sci. 2014;91:1221–30.
Nguyen MTB, Thakrar V, Chan CC. EyePrintPRO therapeutic scleral contact lens: indications and outcomes. Can J Ophthalmol. 2018;53:66–70.
Romero-Jimenez M, Santodomingo-Rubido J, Flores-Rodriguez P, Gonzalez-Meijome JM. Which soft contact lens power is better for piggyback fitting in keratoconus? Cont Lens Anterior Eye. 2013;36:45–48.
Otchere H, Jones L, Sorbara L. The impact of scleral contact lens vault on visual acuity and comfort. Eye Contact Lens.2018;44 Suppl 2:S54–S59.
Rathi VM, Mandathara PS, Dumpati S, Sangwan VS. Change in vault during scleral lens trials assessed with anterior segment optical coherence tomography. Cont Lens Anterior Eye. 2017;40:157–61.
Otchere H, Jones LW, Sorbara L. Effect of time on scleral lens settling and change in corneal clearance. Optom Vis Sci. 2017;94:908–13.
Esen F, Toker E. Influence of apical clearance on mini-scleral lens settling, clinical performance, and corneal thickness changes. Eye Contact Lens. 2017;43:230–5.
Elbendary AM, Abou Samra W. Evaluation of rigid gas permeable lens fitting in keratoconic patients with optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. 2013;251:1565–70.
Rashid ZA, Millodot M, Evans KS. Characteristics of keratoconic patients attending a specialist contact lens clinic in Kenya. Middle East Afr J Ophthalmol. 2016;23:283–7.
Gumus K, Kahraman N. A new fitting approach for providing adequate comfort and visual performance in keratoconus: soft HydroCone (Toris K) lenses. Eye Contact Lens 2016;42:225–30.
Nejabat M, Khalili MR, Dehghani C. Cone location and correction of keratoconus with rigid gas-permeable contact lenses. Cont Lens Anterior Eye. 2012;35:17–21.
Kamar S, Vervaet C, Luyten GP, Jager MJ. Pancorneal contact lens with a toric edge: a new concept in keratoconus. Eur J Ophthalmol. 2011;21:685–90.
Yanai R, Ueda K, Nishida T. Retrospective analysis of vision correction and lens tolerance in keratoconus patients prescribed a contact lens with dual aspherical curves. Eye Contact Lens. 2010;36:86–89.
Jain AK, Sukhija J. Rose-K contact lens for keratoconus. Indian J Ophthalmol. 2007;55:121–5.
Arumugam AO, Rajan R, Subramanian M, Mahadevan R. PROSE for irregular corneas at a tertiary eye care center. Eye Contact Lens. 2014;40:71–73.
Rathi VM, Dumpati S, Mandathara PS, Taneja MM, Sangwan VS. Scleral contact lenses in the management of pellucid marginal degeneration. Cont Lens Anterior Eye. 2016;39:217–20.
Montalt JC, Porcar E, Espana-Gregori E, Peris-Martinez C. Visual quality with corneo-scleral contact lenses for keratoconus management. Cont Lens Anterior Eye. 2018;S1367-0484(17)30270-9.
van der Worp E. A Guide to Scleral Lens Fitting. Books and Monographs. United States of America: Pacific University Common Knowledge; 2010.
Carballo-Alvarez J, Puell MC, Cuina R, Diaz-Valle D, Vazquez JM, Benitez-Del-Castillo JM. Soft contact lens fitting after intrastromal corneal ring segment implantation to treat keratoconus. Cont Lens Anterior Eye. 2014;37:377–81.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lim, L., Lim, E.W.L. Current perspectives in the management of keratoconus with contact lenses. Eye 34, 2175–2196 (2020). https://doi.org/10.1038/s41433-020-1065-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-020-1065-z
This article is cited by
-
Comparative analysis of large language models in providing patient information about keratoconus and contact lenses
International Ophthalmology (2025)
-
Analyzing the changing trend of corneal biomechanical properties under different influencing factors in T2DM patients
Scientific Reports (2024)
-
Bioinformatics analysis of signature genes related to cell death in keratoconus
Scientific Reports (2024)
-
Accelerated corneal cross-linking (18mW/cm2 for 5 min) with HPMC-riboflavin in progressive keratoconus – 5 years follow-up
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
Higher order aberrations in keratoconus
International Ophthalmology (2024)