Abstract
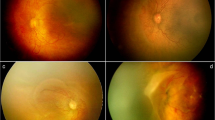
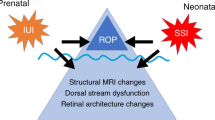
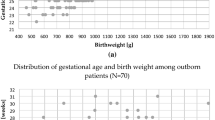
A review of literature was performed, focused on the etiopathogenesis of aggressive posterior retinopathy of prematurity (APROP), the characteristic and atypical clinical features, management strategies, anatomical and visual outcomes. Characteristically APROP has zone I/posterior zone II involvement with prominent plus disease, featureless junction, large vascular loops, flat extra-retinal fibrovascular proliferation, and a rapidly progressive course. The risk factors for APROP are extreme prematurity (birth weight ≤1000 gram and/or gestational age ≤28 weeks), dysregulated oxygen supplementation, intrauterine growth retardation, sepsis, and thrombocytopenia. The uncommon presentations include small zone I disease, a hybrid disease with additional ridge tissue, and APROP in bigger babies with birth weight greater than 1500 g. Laser photocoagulation role is limited by the resultant visual field loss and high refractive error. Although anti-vascular endothelial growth factor injection allows peripheral retinal vascularization; reactivation of disease, systemic absorption of the drug and long-term safety are the chief concerns. Early vitrectomy is required when tractional retinal detachment develops. The visual outcome depends upon the morphology and vascular development of the macula. With the limited yet emerging new understanding of the pathophysiology, a multifaceted rational and individualized treatment strategy is suggested for APROP. Best practices in neonatal intensive care may prevent the occurrence of APROP. Further studies need to be performed for the prevention and safe, effective management of APROP.
摘要
急性进展性后极部早产儿视网膜病变的最新文献综述
摘要:
本文回顾了相关文献, 着重讨论急性进展性后极部早产儿视网膜病变 (aggressive posterior retinopathy of prematurity, APROP) 的发病机制、临床特征、非典型临床特征、治疗策略、解剖及视力的临床结局。APROP的特征性表现为视网膜I区/ 后极部II区受累并且伴有显著的附加病变: 无特征性粘连、大血管袢、平的重度视网膜纤维血管增殖以及病程进展迅速。APROP的危险因素为极度早产儿 (出生体重≤1000克和/或孕周28周) 、吸氧治疗管理不佳、宫内发育迟缓、败血症和血小板减少症。不常见的临床表现包括小范围I区病变、带有额外脊状组织的融合病变, 以及出生体重大于1500克的较大婴儿的APROP。激光光凝由于会导致视野缺损和严重的屈光不正而应用受限。虽然玻璃体内抗血管内皮生长因子注射可导致周边视网膜血管化, 但疾病再度活跃、药物的全身吸收以及长期安全性是主要考虑的因素。当牵拉性视网膜脱离发生时, 需要及早行玻璃体切除术。视力结局取决于黄斑形态和血管的发育。随着我们对APROP病理生理学虽然有限但不断深入的认识, 全面且合理的个体化治疗策略已经提出。最佳的新生儿重症监护可预防APROP发生。为了预防、安全、有效地管理APROP, 需要进行进一步的研究.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol. 2005;123:991–9.
Morizane H. [Initial sign and clinical course of the most severe form of acute proliferative retrolental fibroplasia (type II) (author’s transl)]. Nippon Ganka Gakkai Zasshi. 1976;80:54–61.
Shah PK, Narendran V, Saravanan VR, Raghuram A, Chattopadhyay A, Kashyap M, et al. Fulminate retinopathy of prematurity—clinical characteristics and laser outcome. Indian J Ophthalmol. 2005;53:261–5.
Nissenkorn I, Kremer I, Gilad E, Cohen S, Ben-Sira I. ‘Rush’ type retinopathy of prematurity: report of three cases. Br J Ophthalmol. 1987;71:559–62.
Darlow B, Cust A, Donoghue D. Improved outcomes for very low birthweight infants: evidence from New Zealand national population based data. Arch Dis Child Fetal Neonatal Ed. 2003;88:F23–F28.
Harper RG, Rehman KU, Sia C, Buckwald S, Spinazzola R, Schlessel J, et al. Neonatal outcome of infants born at 500 to 800 grams from 1990 through 1998 in a tertiary care center. J Perinatol J Calif Perinat Assoc. 2002;22:555–62.
Ahn YJ, Hong KE, Yum HR, Lee JH, Kim KS, Youn YA, et al. Characteristic clinical features associated with aggressive posterior retinopathy of prematurity. Eye. 2017;31:924–30.
Holmström G, Hellström A, Jakobsson P, Lundgren P, Tornqvist K, Wallin A. Five years of treatment for retinopathy of prematurity in Sweden: results from SWEDROP, a national quality register. Br J Ophthalmol. 2016;100:1656–61.
Gunay M, Celik G, Tuten A, Karatekin G, Bardak H, Ovali F. Characteristics of severe retinopathy of prematurity in infants with birth weight above 1500 grams at a referral center in Turkey. PLoS ONE. 2016;11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4993354/. Accessed 16 Mar 2019.
Murthy KR, Murthy PR, Shah DA, Nandan MR, S NH, Benakappa N. Comparison of profile of retinopathy of prematurity in semiurban/rural and urban NICUs in Karnataka, India. Br J Ophthalmol. 2013;97:687–9.
Sivanandan S, Chandra P, Deorari AK, Agarwal R. Retinopathy of prematurity: AIIMS, New Delhi experience. Indian Pediatr. 2016;53:S123–S128.
Dwivedi A, Dwivedi D, Lakhtakia S, Chalisgaonkar C, Jain S. Prevalence, risk factors and pattern of severe retinopathy of prematurity in eastern Madhya Pradesh. Indian J Ophthalmol. 2019;67:819–23.
Hungi B, Vinekar A, Datti N, Kariyappa P, Braganza S, Chinnaiah S, et al. Retinopathy of prematurity in a rural Neonatal Intensive Care Unit in South India–a prospective study. Indian J Pediatr. 2012;79:911–5.
Wutthiworawong B, Thitiratsanont U, Saovaprut C, Subhangkasen I, Geyuraphun B, Ampornprut A, et al. Combine intravitreal bevacizumab injection with laser treatment for aggressive posterior retinopathy of prematurity (AP-ROP). J Med Assoc Thai. 2011;94:S15–21.
Padhi TR, Jain L, Behera UC, Pradhan L. Retinopathy of prematurity profile and trend over the years: experience from a two tier city in Eastern India. Indian Pediatr. 2016;53:S76–S79.
Hartnett ME. Advances in understanding and management of retinopathy of prematurity. Surv Ophthalmol. 2017;62:257–76.
Kumar P, Sankar MJ, Deorari A, Azad R, Chandra P, Agarwal R, et al. Risk factors for severe retinopathy of prematurity in preterm low birth weight neonates. Indian J Pediatr. 2011;78:812–6.
Kim SJ, Port AD, Swan R, Campbell JP, Chan RVP, Chiang MF. Retinopathy of prematurity: a review of risk factors and their clinical significance. Surv Ophthalmol. 2018;63:618–37.
Flynn JT, Chan-Ling T. Retinopathy of prematurity: two distinct mechanisms that underlie zone 1 and zone 2 disease. Am J Ophthalmol. 2006;142:46–59.
Lundgren P, Lundberg L, Hellgren G, Holmström G, Hård A-L, Smith LE, et al. Aggressive posterior retinopathy of prematurity is associated with multiple infectious episodes and thrombocytopenia. Neonatology. 2016;111:79–85.
Vinekar A, Hegde K, Gilbert C, Braganza S, Pradeep M, Shetty R, et al. Do platelets have a role in the pathogenesis of aggressive posterior retinopathy of prematurity? Retina. 2010;30:S20–S23.
Drenser KA, Trese MT, Capone A. Aggressive posterior retinopathy of prematurity. Retina. 2010;30:S37–40.
Azuma N, Ishikawa K, Hama Y, Hiraoka M, Suzuki Y, Nishina S. Early vitreous surgery for aggressive posterior retinopathy of prematurity. Am J Ophthalmol. 2006;142:636–43.
Borroni C, Carlevaro C, Morzenti S, De Ponti E, Bozzetti V, Console V, et al. Survey on retinopathy of prematurity (ROP) in Italy. Ital J Pediatr. 2013;39:43.
Shah PK, Narendran V, Kalpana N. Aggressive posterior retinopathy of prematurity in large preterm babies in South India. Arch Dis Child Fetal Neonatal Ed. 2012;97:F371–375.
Sanghi G, Dogra MR, Das P, Vinekar A, Gupta A, Dutta S. Aggressive posterior retinopathy of prematurity in Asian Indian babies: spectrum of disease and outcome after laser treatment. Retina. 2009;29:1335–9.
Nicoară SD, Ștefănuţ AC, Nascutzy C, Zaharie GC, Toader LE, Drugan TC. Regression rates following the treatment of aggressive posterior retinopathy of prematurity with bevacizumab versus laser: 8-year retrospective analysis. Med Sci Monit Int Med J Exp Clin Res. 2016;22:1192–209.
Jalali S, Kesarwani S, Hussain A. Outcomes of a protocol-based management for zone 1 retinopathy of prematurity: the Indian Twin Cities ROP Screening Program report number 2. Am J Ophthalmol. 2011;151:719–724.e2.
Silveira RC, Fortes Filho JB, Procianoy RS. Assessment of the contribution of cytokine plasma levels to detect retinopathy of prematurity in very low birth weight infants. Investig Ophthalmol Vis Sci. 2011;52:1297–301.
Chen J, Smith LEH. Retinopathy of prematurity. Angiogenesis. 2007;10:133–40.
Hellstrom A, Perruzzi C, Ju M, Engstrom E, Hard AL, Liu JL, et al. Low IGF-I suppresses VEGF-survival signaling in retinal endothelial cells: direct correlation with clinical retinopathy of prematurity. Proc Natl Acad Sci USA. 2001;98:5804–8.
Port AD, Chan RVP, Ostmo S, Choi D, Chiang MF. Risk factors for retinopathy of prematurity: insights from outlier infants. Graefes Arch Clin Exp Ophthalmol. 2014;252:1669–77.
Battinelli EM, Markens BA, Italiano JE. Release of angiogenesis regulatory proteins from platelet alpha granules: modulation of physiologic and pathologic angiogenesis. Blood. 2011;118:1359–69.
Radziwon-Balicka A, Moncada de la Rosa C, Jurasz P. Platelet-associated angiogenesis regulating factors: a pharmacological perspective. Can J Physiol Pharmacol. 2012;90:679–88.
Kondo H, Kusaka S, Yoshinaga A, Uchio E, Tawara A, Tahira T. Genetic variants of FZD4 and LRP5 genes in patients with advanced retinopathy of prematurity. Mol Vis. 2013;19:476–85.
Drenser KA, Vinikar A, Dailey W, Trese MT Jr. Aggressive posterior retinopathy of prematurity. Investig Ophthalmol Vis Sci. 2008;49:1388–1388. AC
Mora JS, Waite C, Gilbert CE, Breidenstein B, Sloper JJ. A worldwide survey of retinopathy of prematurity screening. Br J Ophthalmol. 2018;102:9–13.
Fierson WM. American Academy of Pediatrics Section on Ophthalmology, American Academy of Ophthalmology, American Association for Pediatric Ophthalmology and Strabismus, American Association of Certified Orthoptist Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 2013;131:189–95.
Wilkinson AR, Haines L, Head K, Fielder AR, Guideline Development Group of the Royal College of Paediatrics and Child Health, Royal College of Ophthalmologists. et al. UK retinopathy of prematurity guideline. Eye. 2009;23:2137–9.
Singh AK (ed). Guidelines for universal eye screening in newborns including retinopathy of prematurity. 1st Ed. (Rashtriya Bal Swasthya Karyakram, Ministry of Health & Family Welfare, Government of India, 2017).
Xu Y, Zhou X, Zhang Q, Ji X, Zhang Q, Zhu J, et al. Screening for retinopathy of prematurity in China: a neonatal units-based prospective study. Investig Ophthalmol Vis Sci. 2013;54:8229–36.
National Neonatology Forum. Evidence-based clinical practise guidelines, retinopathy of prematurity. India: National Neonatology Forum; 2010.
Sanghi G, Dogra MR, Katoch D, Gupta A. Aggressive posterior retinopathy of prematurity in infants ≥1500 g birth weight. Indian J Ophthalmol. 2014;62:254–7.
Kychenthal A, Dorta P, Katz X. Zone I retinopathy of prematurity: clinical characteristics and treatment outcomes. Retina. 2006;26:S11–15.
Yokoi T, Katagiri S, Hiraoka M, Nakayama Y, Hosono K, Hotta Y, et al. Atypical form of retinopathy of prematurity with severe fibrovascular proliferation in the optic disk region. Retina. 2018;38:1605–12.
Madan A, Penn JS. Animal models of oxygen-induced retinopathy. Front Biosci J Virtual Libr. 2003;8:d1030–1043.
Sanghi G, Dogra MR, Dogra M, Katoch D, Gupta A. A hybrid form of retinopathy of prematurity. Br J Ophthalmol. 2012;96:519–22.
Ahn SJ, Kim JH, Kim S-J, Yu YS. Capillary-free vascularized retina in patients with aggressive posterior retinopathy of prematurity and late retinal capillary formation. Korean J Ophthalmol. 2013;27:109–15.
Lorenz B, Stieger K, Jäger M, Mais C, Stieger S, Andrassi-Darida M. Retinal vascular development with 0.312 MG intravitreal bevacizumab to treat severe posterior retinopathy of prematurity: a Longitudinal Fluorescein Angiographic Study. Retina. 2017;37:97–111.
Yokoi T, Hiraoka M, Miyamoto M, Yokoi T, Kobayashi Y, Nishina S, et al. Vascular abnormalities in aggressive posterior retinopathy of prematurity detected by fluorescein angiography. Ophthalmology. 2009;116:1377–82.
Perente I, Eris E, Seymen Z, Cevik SG, Bekmez S. Aggressive posterior retinopathy of prematurity treated with intravitreal bevacizumab: late period fluorescein angiographic findings. Graefes Arch Clin Exp Ophthalmol. 2019;257:1141–6.
O’Keefe M, Kirwan C. Diode laser versus cryotherapy in treatment of ROP. Br J Ophthalmol. 2006;90:402–3.
Sanghi G, Dogra MR, Katoch D, Gupta A. Aggressive posterior retinopathy of prematurity: risk factors for retinal detachment despite confluent laser photocoagulation. Am J Ophthalmol. 2013;155:159–164.e2.
Gunn DJ, Cartwright DW, Gole GA. Prevalence and outcomes of laser treatment of aggressive posterior retinopathy of prematurity. Clin Exp Ophthalmol. 2014;42:459–65.
Vinekar A, Jayadev C, Mangalesh S, Kumar AK, Bauer N, Capone A, et al. Comparing the outcome of single versus multiple session laser photoablation of flat neovascularization in zone 1 aggressive posterior retinopathy of prematurity: a Prospective Randomized Study. Retina. 2015;35:2130–6.
Gunay M, Celik G, Gunay BO, Aktas A, Karatekin G, Ovali F. Evaluation of 2-year outcomes following intravitreal bevacizumab (IVB) for aggressive posterior retinopathy of prematurity. Arq Bras Oftalmol. 2015;78:300–4.
Pandya HK, Faia LJ, Robinson J, Drenser KA. Macular development in aggressive posterior retinopathy of prematurity. BioMed Res Int. 2015;2015:808639.
Vinekar A, Trese MT, Capone A. Photographic Screening for Retinopathy of Prematurity (PHOTO-ROP) Cooperative Group. Evolution of retinal detachment in posterior retinopathy of prematurity: impact on treatment approach. Am J Ophthalmol. 2008;145:548–55.
Naug HL, Browning J, Gole GA, Gobé G. Vitreal macrophages express vascular endothelial growth factor in oxygen-induced retinopathy. Clin Exp Ophthalmol. 2000;28:48–52.
Austeng D, Källen KBM, Ewald UW, Wallin A, Holmström GE. Treatment for retinopathy of prematurity in infants born before 27 weeks of gestation in Sweden. Br J Ophthalmol. 2010;94:1136–9.
Gunn DJ, Cartwright DW, Yuen SA, Gole GA. Treatment of retinopathy of prematurity in extremely premature infants over an 18-year period. Clin Exp Ophthalmol. 2013;41:159–66.
Trigler L, Weaver RG, O’Neil JW, Barondes MJ, Freedman SF. Case series of angle-closure glaucoma after laser treatment for retinopathy of prematurity. J AAPOS Publ Am Assoc Pediatr Ophthalmol Strabismus. 2005;9:17–21.
Quinn GE, Dobson V, Davitt BV, Wallace DK, Hardy RJ, Tung B, et al. Progression of myopia and high myopia in the Early Treatment for Retinopathy of Prematurity study: findings at 4 to 6 years of age. J AAPOS. 2013;17:124–8.
Hwang CK, Hubbard GB, Hutchinson AK, Lambert SR. Outcomes after intravitreal bevacizumab versus laser photocoagulation for retinopathy of prematurity: a 5-year retrospective analysis. Ophthalmology. 2015;122:1008–15.
Sukgen EA, Koçluk Y. The vascularization process after intravitreal ranibizumab injections for aggressive posterior retinopathy of prematurity. Arq Bras Oftalmol. 2017;80:30–34.
Dikci S, Ceylan OM, Demirel S, Yılmaz T. Which dose of bevacizumab is more effective for the treatment of aggressive posterior retinopathy of prematurity: lower or higher dose? Arq Bras Oftalmol. 2018;81:12–17.
Yetik H, Gunay M, Sirop S, Salihoglu Z. Intravitreal bevacizumab monotherapy for type-1 prethreshold, threshold, and aggressive posterior retinopathy of prematurity - 27 month follow-up results from Turkey. Graefes Arch Clin Exp Ophthalmol. 2015;253:1677–83.
Mintz-Hittner HA, Kuffel RR. Intravitreal injection of bevacizumab (avastin) for treatment of stage 3 retinopathy of prematurity in zone I or posterior zone II. Retina. 2008;28:831–8.
Travassos A, Teixeira S, Ferreira P, Regadas I, Travassos AS, Esperancinha FE, et al. Intravitreal bevacizumab in aggressive posterior retinopathy of prematurity. Ophthalmic Surg Lasers Imaging. 2007;38:233–7.
Mintz-Hittner HA, Kennedy KA, Chuang AZ. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med. 2011;364:603–15.
Harder BC, von Baltz S, Jonas JB, Schlichtenbrede FC. Intravitreal bevacizumab for retinopathy of prematurity. J Ocul Pharmacol Ther. 2011;27:623–7.
Park SW, Jung HH, Heo H. Fluorescein angiography of aggressive posterior retinopathy of prematurity treated with intravitreal anti-VEGF in large preterm babies. Acta Ophthalmol. 2014;92:810–3.
Nicoară SD, Nascutzy C, Cristian C, Irimescu I, Ștefănuț AC, Zaharie G, et al. Outcomes and prognostic factors of intravitreal bevacizumab monotherapy in zone I stage 3+ and aggressive posterior retinopathy of prematurity. J Ophthalmol. 2015;2015:102582.
Mintz-Hittner HA, Geloneck MM, Chuang AZ. Clinical management of recurrent retinopathy of prematurity after intravitreal bevacizumab monotherapy. Ophthalmology. 2016;123:1845–55.
Li X-J, Yang X-P, Sun S, Lyu X-B, Jia H. Intravitreal ranibizumab for aggressive posterior retinopathy of prematurity. Chin Med J. 2016;129:2879–81.
Tong Q, Yin H, Zhao M, Li X, Yu W. Outcomes and prognostic factors for aggressive posterior retinopathy of prematurity following initial treatment with intravitreal ranibizumab. BMC Ophthalmol. 2018;18:150.
Chen S-N, Lian I, Hwang Y-C, Chen Y-H, Chang Y-C, Lee K-H, et al. Intravitreal anti-vascular endothelial growth factor treatment for retinopathy of prematurity: comparison between Ranibizumab and Bevacizumab. Retina. 2015;35:667–74.
Erol MK, Coban DT, Sari ES, Bilgin AB, Dogan B, Ozdemir O, et al. Comparison of intravitreal ranibizumab and bevacizumab treatment for retinopathy of prematurity. Arq Bras Oftalmol. 2015;78:340–3.
Sukgen EA, Koçluk Y. Comparison of clinical outcomes of intravitreal ranibizumab and aflibercept treatment for retinopathy of prematurity. Graefes Arch Clin Exp Ophthalmol. 2019;257:49–55.
Vural A, Perente İ, Onur İU, Eriş E, Seymen Z, Hergünsel GO, et al. Efficacy of intravitreal aflibercept monotherapy in retinopathy of prematurity evaluated by periodic fluorescence angiography and optical coherence tomography. Int. Ophthalmol. 2019;39:2161–9.
Spandau U. What is the optimal dosage for intravitreal bevacizumab for retinopathy of prematurity? Acta Ophthalmol. 2013;91:e154.
Micieli JA, Surkont M, Smith AF. A systematic analysis of the off-label use of bevacizumab for severe retinopathy of prematurity. Am J Ophthalmol. 2009;148:536–543.e2.
Wallace DK, Kraker RT, Freedman SF, Crouch ER, Hutchinson AK, Bhatt AR, et al. Assessment of lower doses of intravitreous bevacizumab for retinopathy of prematurity: a phase 1 dosing study. JAMA Ophthalmol. 2017;135:654–6.
Connor AJ, Papastavrou VT, Hillier RJ, Shafiq A. Ultra-low dose of intravitreal bevacizumab in the treatment of retinopathy of prematurity. J Pediatr Ophthalmol Strabismus. 2015;52:e20–21.
Wallace DK, Dean TW, Hartnett ME, Kong L, Smith LE, Hubbard GB, et al. A dosing study of bevacizumab for retinopathy of prematurity: late recurrences and additional treatments. Ophthalmology. 2018;125:1961–6.
Kara C, Hekimoğlu E, Petriçli İS, Akıl H. Intravitreal bevacizumab as rescue therapy following treatment failure with laser photocoagulation in retinopathy of prematurity. J Curr Ophthalmol. 2018;30:80–84.
Honda S, Hirabayashi H, Tsukahara Y, Negi A. Acute contraction of the proliferative membrane after an intravitreal injection of bevacizumab for advanced retinopathy of prematurity. Graefes Arch Clin Exp Ophthalmol. 2008;246:1061–3.
Padhi TR, Das T, Rath S, Pradhan L, Sutar S, Panda KG, et al. Serial evaluation of retinal vascular changes in infants treated with intravitreal bevacizumab for aggressive posterior retinopathy of prematurity in zone I. Eye. 2016;30:392–9.
Ekinci DY, Vural AD, Bayramoglu SE, Onur IU, Hergunsel GO. Assessment of vascular leakage and its development with FFA among patients treated with intravitreal anti-VEGF due to aggressive posterior ROP. Int. Ophthalmol. 2019;39:2697–705.
Huang Q, Zhang Q, Fei P, Xu Y, Lyu J, Ji X, et al. Ranibizumab injection as primary treatment in patients with retinopathy of prematurity: anatomic outcomes and influencing factors. Ophthalmology. 2017;124:1156–64.
Scapini P, Nesi L, Morini M, Tanghetti E, Belleri M, Noonan D, et al. Generation of biologically active angiostatin kringle 1-3 by activated human neutrophils. J Immunol. 2002;168:5798–804.
Wu A-L, Wu W-C. Anti-VEGF for ROP and pediatric retinal diseases. Asia-Pac J Ophthalmol. 2018;7:145–51.
Wu W-C, Yeh P-T, Chen S-N, Yang C-M, Lai C-C, Kuo H-K. Effects and complications of bevacizumab use in patients with retinopathy of prematurity: a multicenter study in taiwan. Ophthalmology. 2011;118:176–83.
Sankar MJ, Sankar J, Chandra P. Anti-vascular endothelial growth factor (VEGF) drugs for treatment of retinopathy of prematurity. Cochrane Database Syst Rev. 2018;1:CD009734.
Khokhar S, Chandra P, Gupta Y, Kumawat D, Dhull C. Bilateral total cataract after intravitreal bevacizumab injection in aggressive posterior retinopathy of prematurity. J Pediatr Ophthalmol Strabismus. 2019;56:e28–e30.
Vanathi M, Kumawat D, Singh R, Chandra P. Iatrogenic crystalline lens injury in pediatric eyes following intravitreal injection for retinopathy of prematurity. J Pediatr Ophthalmol Strabismus. 2019;56:162–7.
Haigh JJ. Role of VEGF in organogenesis. Organogenesis. 2008;4:247–56.
Lien R, Yu M-H, Hsu K-H, Liao P-J, Chen Y-P, Lai C-C, et al. Neurodevelopmental outcomes in infants with retinopathy of prematurity and bevacizumab treatment. PLoS ONE. 2016;11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4729687/. Accessed 2 March 2019.
Morin J, Luu TM, Superstein R, Ospina LH, Lefebvre F, Simard M-N, et al. Neurodevelopmental outcomes following bevacizumab injections for retinopathy of prematurity. Pediatrics. 2016;137:e20153218.
Natarajan G, Shankaran S, Nolen TL, Sridhar A, Kennedy KA, Hintz SR, et al. Neurodevelopmental outcomes of preterm infants with retinopathy of prematurity by treatment. Pediatrics. 2019;144:e20183537.
Kennedy KA, Mintz-Hittner HA.BEAT-ROP Cooperative Group Medical and developmental outcomes of bevacizumab versus laser for retinopathy of prematurity. J AAPOS. 2018;22:61–65.e1.
Fan Y-Y, Huang Y-S, Huang C-Y, Hsu J-F, Shih C-P, Hwang Y-S, et al. Neurodevelopmental outcomes after intravitreal bevacizumab therapy for retinopathy of prematurity: a prospective case-control study. Ophthalmology. 2019;126:1567–77.
Rodriguez SH, Peyton C, Lewis K, Andrews B, Greenwald MJ, Schreiber MD, et al. Neurodevelopmental outcomes comparing bevacizumab to laser for type 1 ROP. Ophthalmic Surg Lasers Imaging Retin. 2019;50:337–43.
Chandra P, Kumawat D, Tewari R, Azimeera S. Post-ranibizumab injection endophthalmitis in aggressive posterior retinopathy of prematurity. Indian J Ophthalmol. 2019;67:967–9.
Chung EJ, Kim JH, Ahn HS, Koh HJ. Combination of laser photocoagulation and intravitreal bevacizumab (Avastin) for aggressive zone I retinopathy of prematurity. Graefes Arch Clin Exp Ophthalmol. 2007;245:1727–30.
Altinsoy HI, Mutlu FM, Güngör R, Sarici SÜ. Combination of laser photocoagulation and intravitreal bevacizumab in aggressive posterior retinopathy of prematurity. Ophthalmic Surg Lasers Imaging. 2010:42:1–5.
Law JC, Recchia FM, Morrison DG, Donahue SP, Estes RL. Intravitreal bevacizumab as adjunctive treatment for retinopathy of prematurity. J AAPOS. 2010;14:6–10.
Spandau U, Tomic Z, Ewald U, Larsson E, Akerblom H, Holmström G. Time to consider a new treatment protocol for aggressive posterior retinopathy of prematurity? Acta Ophthalmol. 2013;91:170–5.
Xu Y, Kang X, Zhang Q, Huang Q, Lv J, Zhao P. Combination of intravitreal injection of ranibizumab and photocoagulation for the treatment of aggressive posterior retinopathy of prematurity with vitreous hemorrhage. J Ophthalmol. 2016;2016:5029278.
Garcia Gonzalez JM, Snyder L, Blair M, Rohr A, Shapiro M, Greenwald M. Prophylactic peripheral laser and fluorescein angiography after bevacizumab for retinopathy of prematurity. Retina. 2018;38:764–72.
Sato T, Wada K, Arahori H, Kuno N, Imoto K, Iwahashi-Shima C, et al. Serum concentrations of bevacizumab (avastin) and vascular endothelial growth factor in infants with retinopathy of prematurity. Am J Ophthalmol. 2012;153:327–333.e1.
Shah PK, Subramanian P, Venkatapathy N, Chan RVP, Chiang MF, Campbell JP. Aggressive posterior retinopathy of prematurity in two cohorts of patients in South India: implications for primary, secondary, and tertiary prevention. J AAPOS. 2019;23:264.e1-264.e4.
Hinz BJ, de Juan E, Repka MX. Scleral buckling surgery for active stage 4A retinopathy of prematurity. Ophthalmology. 1998;105:1827–30.
Azuma N, Ito M, Yokoi T, Nakayama Y, Nishina S. Visual outcomes after early vitreous surgery for aggressive posterior retinopathy of prematurity. JAMA Ophthalmol. 2013;131:1309–13.
Yokoi T, Yokoi T, Kobayashi Y, Nishina S, Azuma N. Risk factors for recurrent fibrovascular proliferation in aggressive posterior retinopathy of prematurity after early vitreous surgery. Am J Ophthalmol. 2010;150:10–15.e1.
Micelli Ferrari T, Furino C, Lorusso VV, Dammacco R, Sborgia G, Sborgia L, et al. Three-port lens-sparing vitrectomy for aggressive posterior retinopathy of prematurity: early surgery before tractional retinal detachment appearance. Eur J Ophthalmol. 2007;17:785–9.
Nishina S, Yokoi T, Yokoi T, Kobayashi Y, Hiraoka M, Azuma N. Effect of early vitreous surgery for aggressive posterior retinopathy of prematurity detected by fundus fluorescein angiography. Ophthalmology. 2009;116:2442–7.
Tanaka S, Yokoi T, Katagiri S, Yoshida T, Nishina S, Azuma N. Severe recurrent fibrovascular proliferation after combined intravitreal bevacizumab injection and laser photocoagulation for aggressive posterior retinopathy of prematurity. Retin Cases Brief Rep. 2019 Jul 17. Epub ahead of print. PMID: 31339872.
De la Huerta I, Yonekawa Y, Thomas BJ, Capone A. A surgical technique for the management of tractional retinal detachment in aggressive posterior retinopathy of prematurity treated with intravitreal bevacizumab. Retina. 2019;39:S156–S159.
van der Griend BF, Lister NA, McKenzie IM, Martin N, Ragg PG, Sheppard SJ, et al. Postoperative mortality in children after 101,885 anesthetics at a tertiary pediatric hospital. Anesth Analg. 2011;112:1440–7.
Sinha R, Talawar P, Ramachandran R, Azad R, Mohan VK. Perioperative management and post-operative course in preterm infants undergoing vitreo-retinal surgery for retinopathy of prematurity: a retrospective study. J Anaesthesiol Clin Pharmacol. 2014;30:258–62.
Yonekawa Y, Wu W-C, Kusaka S, Robinson J, Tsujioka D, Kang KB, et al. Immediate sequential bilateral pediatric vitreoretinal surgery: an International Multicenter Study. Ophthalmology. 2016;123:1802–8.
Shah PK, Ramakrishnan M, Sadat B, Bachu S, Narendran V, Kalpana N. Long term refractive and structural outcome following laser treatment for zone 1 aggressive posterior retinopathy of prematurity. Oman J Ophthalmol. 2014;7:116–9.
Chandra P, Tewari R, Salunkhe N, Kumawat D, Kumar V. Giant retinal tear with retinal detachment in regressed aggressive posterior retinopathy of prematurity treated by laser. J Pediatr Ophthalmol Strabismus. 2017;54:e34–e36.
Chandra P, Tewari R, Jain S. The restless retina in aggressive posterior retinopathy of prematurity: prevention is better than cure. Community Eye Health. 2018;31:S27–S28.
Chow LC, Wright KW, Sola A, CSMC Oxygen Administration Study Group. Can changes in clinical practice decrease the incidence of severe retinopathy of prematurity in very low birth weight infants? Pediatrics. 2003;111:339–45.
Fang JL, Sorita A, Carey WA, Colby CE, Murad MH, Alahdab F. Interventions to prevent retinopathy of prematurity: a meta-analysis. Pediatrics. 2016;137:e20153387.
Vinekar A, Jayadev C, Kumar S, Mangalesh S, Dogra MR, Bauer NJ, et al. Impact of improved neonatal care on the profile of retinopathy of prematurity in rural neonatal centers in India over a 4-year period. Eye Brain. 2016;8:45–53.
Chen ML, Guo L, Smith LEH, Dammann CEL, Dammann O. High or low oxygen saturation and severe retinopathy of prematurity: a meta-analysis. Pediatrics. 2010;125:e1483–1492.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kumawat, D., Sachan, A., Shah, P. et al. Aggressive posterior retinopathy of prematurity: a review on current understanding. Eye 35, 1140–1158 (2021). https://doi.org/10.1038/s41433-021-01392-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-021-01392-6
This article is cited by
-
Optimised multivariable prediction model to predict treatment requirement in preterm infants with retinopathy of prematurity
Eye (2026)
-
Oxygen therapy-related risk factors for aggressive retinopathy of prematurity in low-risk preterm neonates
Pediatric Research (2025)
-
Fundus fluorescein angiography in retinopathy of prematurity
Eye (2022)
-
Analysis of a two-year independent screening effort for retinopathy of prematurity in rural Egypt
BMC Ophthalmology (2021)