Abstract
Objective
To determine visual outcomes and prevalence of amblyogenic risk factors in children with Apert, Crouzon, Pfeiffer and Saethre-Chotzen syndromes.
Methods
We conducted a single-centre, retrospective chart review of patients assessed at our unit between October 2000 and May 2017. Our outcome measures were as follows: age at first and last examination, refraction, horizontal ocular alignment, alphabet pattern deviations, anterior segment appearance, fundus examination findings, visual evoked potentials (VEPs) and genetics. The study’s primary endpoint was the proportion of children achieving best-corrected visual acuity (BCVA) ≥ 6/12 in the better eye at final visit, as per UK driving standards.
Results
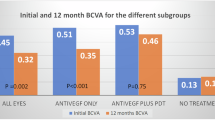
165 patients were included in this study. Breakdown of diagnoses was as follows: Crouzon (n = 60), Apert (n = 57), Pfeiffer (n = 14) and Saethre-Chotzen (n = 34). 98 patients were male. Of 133 patients with full BCVA data available, 76.7% achieved BCVA ≥ 6/12 in the better eye. Of 122 patients, anisometropia >1.00 dioptre sphere (DS) affected 18.9% and astigmatism ≥1.00DS in at least one eye affected 67.2%. Of 246 eyes, 48.4% had oblique astigmatism. Of 165 patients, 60 had exotropia and 12 had esotropia. 48 of 99 patients demonstrated ‘V’ pattern. On multivariable logistic regression, nystagmus (p = 0.009) and ON involvement (p = 0.001) were associated with decreased vision in the worse eye. Normal VEPs were associated with better BCVA (p = 0.036).
Conclusion
There was a high prevalence of amblyogenic factors, however, the majority achieved BCVA ≥ 6/12 in their better eye. Optic neuropathy and nystagmus had the most significant impact on vision. VEPs can help the in overall assessment of visual function.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Cohen MM Jr. Apert, crouzon, and pfeiffer syndromes. In: Muenke M, Kress W, Collmann H, Solomon BD, editors. Monographs in human genetics. Basel: Karger; 2011. vol. 19, pp 67–88. https://doi.org/10.1159/isbn.978-3-8055-9595-7
Kressa W, Collmann H. Saethre-chotzen syndrome: clinical and molecular genetic aspects. In: Muenke M, Kress W, Collmann H, Solomon BD, editors. Monographs in human genetics. Basel: Karger; 2011. vol. 19, pp. 98–106. https://doi.org/10.1159/isbn.978-3-8055-9595-7
Muenke M, Kress W, Collman H, Solomon BD. Craniosynostoses: molecular genetics, principles of diagnosis, and treatment. Basel, Switzerland: S. Karger; 2011
Khan SH, Nischal KK, F Dean F, Hayward RD, Walker J. Visual outcomes and amblyogenic risk factors in craniosynostotic syndromes: a review of 141 cases. Br J Ophthalmol. 2003;87:999–1003.
Liasis A, Thompson DA, Hayward R, Nischal KK. Sustained raised intracranial pressure implicated only by pattern reversal visual evoked potentials after cranial vault expansion surgery. Pediatr Neurosurg. 2003;39:75–80.
Liasis A, Nischal KK, Leighton S, Yap S, Hayward R, Dunaway D. Adenoid-tonsillectomy to treat visual dysfunction in a child with craniosynostosis. Pediatr Neurosurg. 2005;4:197–200.
Thompson DA, Liasis A, Hardy S, Hagan R, Hayward RD, Evans RD, et al. Prevalence of abnormal pattern reversal visual evoked potentials in craniosynostosis. Plast Reconstr Surg. 2006;118:184–92.
Liasis A, Nischal KK, Walters B, Thompson D, Hardy S, Towell A, et al. Monitoring visual function in children with syndromic craniosynostosis: a comparison of 3 methods. Arch Ophthalmol. 2006;124:1119–26.
GOV.UK. Driving eyesight rules. 2020. https://www.gov.uk/driving-eyesight-rules. Accessed 12 Feb 2020.
Denis D, Genitori L, Bolufer A, Lena G, Saracco JB, Choux M. Refractive error and ocular motility in plagiocephaly. Child’s Nerv Syst. 1994;10:210–16.
Abrahamsson M, Sjostrand J. Astigmatic axis and amblyopia in childhood. Acta Ophthalmologica Scandinavica. 2003;81:33–37.
Tay T, Martin F, Rowe N, Johnson K, Poole M, Tan K, et al. Prevalence and causes of visual impairment in craniosynostotic syndromes. Clin Exp Ophthalmol. 2006;34:434–40.
de Jong T, Bannink N, Bredero-Boelhouwer HH, van Veelen MLC, Bartels MC, Hoeve LJ, et al. Long-term functional outcome in 167 patients with syndromic craniosynostosis; defining a syndrome-specific risk profile. J Plast Reconstr Aesthet Surg. 2010;63:1635–41. https://doi.org/10.1016/j.bjps.2009.10.029
Khong JJ, Anderson P, Gray TL, Hammerton M, Selva D, David D. Ophthalmic findings in Apert’s syndrome prior to craniofacial surgery. Am J Ophthalmol 2006;142:328–30.
Khong JJ, Anderson P, Gray TL, Hammerton M, Selva D, David D. Ophthalmic findings in Apert’s syndrome after craniofacial surgery twenty-nine years’ experience. Ophthalmology. 2006;113:347–52. https://doi.org/10.1016/j.ophtha.2005.10.011
Sjöstrand J, Abrahamsson M. Risk factors in amblyopia. Eye. 1990;4:787–93.
Jadico SK, Young DA, Huebner A, Edmond JC, Pollock AN, McDonald-McGinn DM, et al. Ocular abnormalities in Apert syndrome: genotype/phenotype correlations with fibroblast growth factor receptor type 2 mutations. J Aapos. 2006;10:521–7.
Khong JJ, Anderson PJ, Hammerton M, Roscioli T, Selva D, David DJ. Differential effects of FGFR2 mutation in ophthalmic findings in apert syndrome. J Craniofac Surg. 2007;18:39–42.
Mathijssen IMJ. Guideline for care of patients with the diagnoses of craniosynostosis: working group on craniosynostosis. J Craniofacial Surg. 2015;26:1735–807. https://doi.org/10.1097/SCS.0000000000002016
Cornelissen M, den Ottelander B, Rizopoulos D, van der Hulst R, van der Molen AM, van der Horst C, et al. Increase of prevalence of craniosynostosis. J Craniomaxillofac Surg. 2016;44:1273–9. https://doi.org/10.1016/j.jcms.2016.07.007
Di Rocco F, Arnaud E, Renier D. Evolution in the frequency of nonsyndromic craniosynostosis. J Neurosurg Pediatrics. 2009;4:21–25.
Acknowledgements
The authors would like to thank Andrea White for assistance with case identification and data collection. SRR’s post is funded by a National Institute for Health Research (NIHR) Doctoral Fellowship. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
AMH: methodology, formal analysis, investigation, data curation, writing—original draft, visualization. DAT: methodology, formal analysis, investigation, writing—original draft, writing—review and editing, visualization. SRR: formal analysis, writing—review and editing, visualization. KW: investigation, writing—review and editing. KS: investigation, writing—review and editing. VP: investigation. GJ: writing—review and editing. RB: Conceptualization, methodology, formal analysis, investigation, writing—review and editing, supervision, project administration.
Corresponding author
Ethics declarations
Conflict of interest
The authors declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hinds, AM., Thompson, D.A., Rufai, S.R. et al. Visual outcomes in children with syndromic craniosynostosis: a review of 165 cases. Eye 36, 1005–1011 (2022). https://doi.org/10.1038/s41433-021-01458-5
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-021-01458-5
This article is cited by
-
Surgical management of raised ICP in craniosynostosis: experience-based selection of posterior vault expansion techniques
Child's Nervous System (2025)
-
Utility of invasive intracranial pressure monitoring in children with craniosynostosis: relationship to clinical assessment, syndrome and surgical treatment
Child's Nervous System (2025)
-
The awareness of treatment plans of craniosynostosis: guideline for patient and family version
Egyptian Pediatric Association Gazette (2024)
-
Ocular manifestations and treatment progress of Crouzon syndrome
International Ophthalmology (2024)
-
Electrophysiological and fundoscopic detection of intracranial hypertension in craniosynostosis
Eye (2023)