Abstract
Background
Hormonal contraceptives (HCs) are a known risk factor for dry eye disease (DED), yet the relationship between HCs use and DED in women of child-bearing age remains debatable. The aim of this study was to determine the association between HCs and DED in females of reproductive age.
Methods
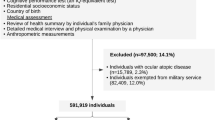
This was a retrospective cohort study using data from IQVIA’s electronic medical record (IQVIA, USA). 4,871,504 women (age 15–45) between 2008 and 2018 were followed to the first diagnosis of DED as defined by an ICD-9/10 code. DED cases also required at least two prescriptions of cyclosporine or lifitegrast topical drops within 60 days of the first code. The date of the first code was designated as the index date. Regular HCs users needed to have at least two prescriptions in both the first year and second year prior to the index date. For each case, five controls were selected and matched to cases by age and follow-up time. A conditional logistic regression model was used to adjust for confounders of DED and to calculate odds ratios (ORs).
Results
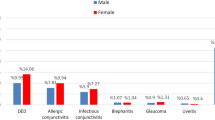
HCs users were at a higher risk for DED than non-users. Regular users of HCs were more likely to develop DED (ORs = 2.73, 95% CI [2.21–3.73]) than irregular users. Those who used a greater number of HCs were at a higher risk for DED.
Conclusions
This study indicates an increased risk of DED with HCs use in women of child-bearing age.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Stapleton F, Alves M, Bunya VY, Jalbert I, Lekhanont K, Malet F, et al. TFOS DEWS II Epidemiology Report. Ocul Surf. 2017;15:334–65.
Schaumberg DA, Sullivan DA, Buring JE, Dana MR. Prevalence of dry eye syndrome among US women. Am J Ophthalmol. 2003;136:318–26.
Schaumberg DA, Uchino M, Christen WG, Semba RD, Buring JE, Li JZ. Patient reported differences in dry eye disease between men and women: impact, management, and patient satisfaction. PLoS ONE. 2013;8:e76121.
Pflugfelder SC, de Paiva CS. The Pathophysiology of Dry Eye Disease: what We Know and Future Directions for Research. Ophthalmology. 2017;124:S4–S13.
Wan KH, Chen LJ, Young AL. Depression and anxiety in dry eye disease: a systematic review and meta-analysis. Eye. 2016;30:1558–67.
McDonald M, Patel DA, Keith MS, Snedecor SJ. Economic and Humanistic Burden of Dry Eye Disease in Europe, North America, and Asia: a Systematic Literature Review. Ocul Surf. 2016;14:144–67.
Yu J, Asche CV, Fairchild CJ. The economic burden of dry eye disease in the United States: a decision tree analysis. Cornea. 2011;30:379–87.
Schaumberg DA, Buring JE, Sullivan DA, Dana MR. Hormone Replacement Therapy and Dry Eye Syndrome. JAMA. 2001;286:2114–9.
United Nations Department of Economic and Social Affairs, Population Division. Contraceptive Use by Method 2019: Data Booklet. United Nations. 2019;435.
Schaumberg DA, Buring JE, Sullivan DA, Dana MR. Hormone Replacement Therapy and Dry Eye Syndrome. JAMA. 2001;286:2114–9.
Fraunfelder FT, Sciubba JJ, Mathers WD. The role of medications in causing dry eye. J Ophthalmol. 2012;2012:285851.
Neudorfer M, Goldshtein I, Shamai-Lubovitz O, Chodick G, Dadon Y, Shalev V. Ocular Adverse Effects of Systemic Treatment With Isotretinoin. Arch Dermatol. 2012;148:803–8.
Kassan SS, Moutsopoulos HM. Clinical Manifestations and Early Diagnosis of Sjögren Syndrome. Arch Intern Med. 2004;164:1275–84.
Alanazi SA, Alomran AA, Abusharha A, Fagehi R, Al-Johani N, El-Hiti G, et al. An assessment of the ocular tear film in patients with thyroid disorders. Clin Ophthalmol (Auckl, N. Z). 2019;13:1019–26.
Suissa S. The Quasi-cohort approach in pharmacoepidemiology: upgrading the nested case-control. Epidemiology. 2015;26:242–6.
Hernán MA, Robins JM. Causal Inference: What If. Boca Raton: Chapman & Hall/CRC; 2020.
Chen SP, Massaro-Giordano G, Pistilli M, Schreiber CA, Bunya VY. Tear osmolarity and dry eye symptoms in women using oral contraception and contact lenses. Cornea. 2013;32:423–8.
Khanal S, Millar TJ. Barriers to clinical uptake of tear osmolarity measurements. Br J Ophthalmol. 2012;96:341–4.
Frankel SH, Ellis PP. Effect of oral contraceptives on tear production. Ann Ophthalmol. 1978;10:1585–8.
Tomlinson A, Pearce EI, Simmons PA, Blades K. Effect of oral contraceptives on tear physiology. Ophthalmic Physiol Opt. 2001;21:9–16.
Sharma A, Porwal S, Tyagi M. Effect of oral contraceptives on tear film in reproductive age group women. Int J Reprod, Contracept, Obstet Gynecol. 2018;7:861.
Uncu G, Avci R, Uncu Y, Kaymaz C, Develioğlu O. The effects of different hormone replacement therapy regimens on tear function, intraocular pressure and lens opacity. Gynecol Endocrinol. 2006;22:501–5.
Saif MYS, Sayed MA, Saif ATS. Effect of hormonal contraception on lacrimal gland function. Guoji Yanke Zazhi (Int Eye Sci). 2016;16:1207–11.
Feng Y, Feng G, Peng S, Li H. The effects of hormone replacement therapy on dry eye syndromes evaluated by Schirmer test depend on patient age. Contact Lens and Anterior. Eye. 2016;39:124–7.
Feng Y, Feng G, Peng S, Li H. The Effect of Hormone Replacement Therapy on Dry Eye Syndrome Evaluated with Schirmer Test and Break-Up Time. J Ophthalmol. 2015;2015:420302.
Clayton JA. Dry Eye. N Engl J Med. 2018;378:2212–23.
Truong S, Cole N, Stapleton F, Golebiowski B. Sex hormones and the dry eye. Clin Exp Optom. 2014;97:324–36.
Esmaeli B, Harvey JT, Hewlett B. Immunohistochemical evidence for estrogen receptors in meibomian glands. Ophthalmology. 2000;107:180–4.
Suzuki T, Schirra F, Richards SM, Jensen RV, Sullivan DA. Estrogen and Progesterone Control of Gene Expression in the Mouse Meibomian Gland. Investig Ophthalmol Vis Sci. 2008;49:1797–808.
Sullivan DA, Yamagami H, Liu M, Steagall RJ, Schirra F, Suzuki T, et al. Sex Steroids, the Meibomian Gland and Evaporative Dry Eye. In: Sullivan DA, Stern ME, Tsubota K, Dartt DA, Sullivan RM, Bromberg BB, editors. Lacrimal Gland, Tear Film, and Dry Eye Syndromes 3: Basic Science and Clinical Relevance Part A and B. Boston, MA: Springer US; 2002. p. 389–99.
Suzuki T, Schirra F, Richards SM, Treister NS, Lombardi MJ, Rowley P, et al. Estrogen’s and Progesterone’s Impact on Gene Expression in the Mouse Lacrimal Gland. Investig Ophthalmol Vis Sci. 2006;47:158–68.
Sun M, Moreno IY, Dang M, Coulson-Thomas V. Meibomian Gland Dysfunction: what Have Animal Models Taught Us? Int J Mol Sci. 2020;21:8822.
Driver PJ, Lemp MA. Meibomian gland dysfunction. Surv Ophthalmol. 1996;40:343–67.
Sullivan BD, Evans JE, Dana MR, Sullivan DA. Impact of androgen deficiency on the lipid profiles in human meibomian gland secretions. Adv Exp Med Biol. 2002;506:449–58.
Sullivan BD, Evans JE, Krenzer KL, Reza Dana M, Sullivan DA. Impact of Antiandrogen Treatment on the Fatty Acid Profile of Neutral Lipids in Human Meibomian Gland Secretions1. J Clin Endocrinol Metab. 2000;85:4866–73.
Richards SM, Liu M, Jensen RV, Schirra F, Yamagami H, Lombardi MJ, et al. Androgen regulation of gene expression in the mouse lacrimal gland. J Steroid Biochem Mol Biol. 2005;96:401–13.
Sullivan DA, Bélanger A, Cermak JM, Bérubé R, Papas AS, Sullivan RM, et al. Are women with Sjögren’s syndrome androgen-deficient? J Rheumatol. 2003;30:2413–9.
Sullivan DA, Allansmith MR. Hormonal modulation of tear volume in the rat. Exp Eye Res. 1986;42:131–9.
Azzarolo AM, Wood RL, Mircheff AK, Richters A, Olsen E, Berkowitz M, et al. Androgen influence on lacrimal gland apoptosis, necrosis, and lymphocytic infiltration. Investig Ophthalmol Vis Sci. 1999;40:592–602.
Luo F, Zhang H, Sun X. The change of tear secretion and tear film stability in castrated male rabbits. Zhonghua Yan Ke Za Zhi. 2001;37:458–61.
Acknowledgements
This study was funded partly by the Canadian Institute for Health Research (CIHR) Project Grant and by the Department of Ophthalmology and Visual Sciences, University of British Columbia.
Author information
Authors and Affiliations
Contributions
S.Y.: Conceptualisation, Methodology, Validation, Writing—Review & Editing, Supervision. A.K.: Methodology, Data curation, Formal analysis. M.E.: Methodology, Data curation, Formal analysis, Writing—Original Draft, Writing—Review & Editing. A.I.: Conceptualisation, Methodology, Validation, Writing—Review & Editing. B.H.: Investigation, Data curation, Writing—Original Draft, Writing—Review & Editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
He, B., Iovieno, A., Etminan, M. et al. Effects of hormonal contraceptives on dry eye disease: a population-based study. Eye 36, 634–638 (2022). https://doi.org/10.1038/s41433-021-01517-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-021-01517-x
This article is cited by
-
Dry Eye Disease: From Causes to Patient Care and Clinical Collaboration—A Narrative Review
Ophthalmology and Therapy (2025)
-
Assessment of the prevalence and risk factors for dry eye symptoms among Romanian medical students using the ocular surface disease index – a cross-sectional study
BMC Ophthalmology (2024)