Abstract
Purpose
The study aimed to test whether symptomatic dry eye in aromatase inhibitor (AI) patients is associated with the clinical features of evaporative dry eye.
Methods
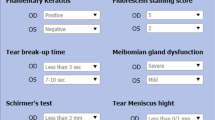
A cross-sectional, observational study of postmenopausal women treated with AI was conducted. Clinical information was gathered from their treating clinician. Ocular and treatment symptoms were assessed using validated questionnaires. Clinical assessments were performed to assess for dry eye. The primary outcome measure for this study was dry eye symptoms measured via questionnaire. The secondary outcome measures were clinical signs of dry eye and hormone levels.
Results
A total of 25 women on AI were recruited. 64% of women reported symptoms of dry eye (ocular surface disease index ≥ 13). Higher tear osmolarity (323 vs 307 mOsm/L, p = 0.002) and increased meibomian gland dropout (4 vs 1, p = 0.002) were observed in patients with symptomatic dry eye when compared to asymptomatic patients. Multivariate logistic regression identified that longer duration of AI use and higher tear osmolarity increased the likelihood of a patient experiencing dry eye symptoms.
Conclusion
Our study found increased tear osmolarity and meibomian gland drop out in women on AI with symptomatic dry eye. Longer duration of AI therapy and higher tear osmolarity may increase the risk of developing dry eye.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Feuer EJ, Wun L-M, Boring CC, Tong T, Flanders WD, Timmel MJ. The Lifetime Risk of Developing Breast Cancer. JNCI: J Natl Cancer Inst. 1993;85:892–7.
Chu KC, Anderson WF, Fritz A, Ries LAG, Brawley OW. Frequency distributions of breast cancer characteristics classified by estrogen receptor and progesterone receptor status for eight racial/ethnic groups. Cancer. 2001;92:37–45.
Garreau JR, DeLaMelena T, Walts D, Karamlou K, Johnson N. Side effects of aromatase inhibitors versus tamoxifen: the patients’ perspective. Am J Surg. 2006;192:496–8.
Turaka K, Nottage JM, Hammersmith KM, Nagra PK, Rapuano CJ. Dry eye syndrome in aromatase inhibitor users. Clin Exp Ophthalmol. 2013;41:239–43.
Cuzick J, Sestak I, Forbes JF, Dowsett M, Knox J, Cawthorn S, et al. Anastrozole for prevention of breast cancer in high-risk postmenopausal women (IBIS-II): an international, double-blind, randomised placebo-controlled trial. Lancet. 2014;383:1041–8.
Inglis H, Boyle FM, Friedlander ML, Watson SL. Dry eyes and AIs: if you don’t ask you won’t find out. Breast. 2015;24:694–8.
Gibson E, Stapleton F, Dear R, Wolffsohn JS, Golebiowski B. Dry eye signs and symptoms in aromatase inhibitor treatment and the relationship with pain. Ocul Surf. 2020;18:108–13.
Esmaeli B, Harvey JT, Hewlett B. Immunohistochemical evidence for estrogen receptors in meibomian glands. Ophthalmology. 2000;107:180–4.
Azzarolo AM, Eihausen H, Schechter J. Estrogen prevention of lacrimal gland cell death and lymphocytic infiltration. Exp Eye Res. 2003;77:347–54.
Coksuer H, Ozcura F, Oghan F, Haliloglu B, Coksuer C. Effects of estradiol–drospirenone on ocular and nasal functions in postmenopausal women. Climacteric. 2011;14:482–7.
Cohen J. Statistical power analysis. Curr Dir Psychol Sci. 1992;1:98–101.
Wolffsohn JS, Arita R, Chalmers R, Djalilian A, Dogru M, Dumbleton K, et al. TFOS DEWS II Diagnostic Methodology report. Ocul Surf. 2017;15:539–74.
Geisler J, Ekse D, Helle H, Duong NK, Lønning PE. An optimised, highly sensitive radioimmunoassay for the simultaneous measurement of estrone, estradiol and estrone sulfate in the ultra-low range in human plasma samples. J Steroid Biochem Mol Biol. 2008;109:90–5.
Willcox MDP, Argueso P, Georgiev GA, Holopainen JM, Laurie GW, Millar TJ, et al. TFOS DEWS II Tear Film Report. Ocul Surf. 2017;15:366–403.
Keech A, Senchyna M, Jones L. Impact of time between collection and collection method on human tear fluid osmolarity. Curr Eye Res. 2013;38:428–36.
Tomlinson A, Khanal S, Ramaesh K, Diaper C, McFadyen A. Tear Film Osmolarity: determination of a Referent for Dry Eye Diagnosis. Investig Ophthalmol Vis Sci. 2006;47:4309–15.
Golebiowski B, Badarudin N, Eden J, You J, Hampel U, Stapleton F. Does endogenous serum oestrogen play a role in meibomian gland dysfunction in postmenopausal women with dry eye? Br J Ophthalmol. 2017;101:218–22.
Koh S, Ikeda C, Watanabe S, Oie Y, Soma T, Watanabe H, et al. Effect of non‐invasive tear stability assessment on tear meniscus height. Acta Ophthalmologica. 2015;93:e135–e9.
Kim J, Kim JY, Seo KY, Kim TI, Chin HS, Jung JW. Location and pattern of non‐invasive keratographic tear film break‐up according to dry eye disease subtypes. Acta Ophthalmologica. 2019;97:e1089–e97.
Arita R, Morishige N, Koh S, Shirakawa R, Kawashima M, Sakimoto T, et al. Increased tear fluid production as a compensatory response to meibomian gland loss: a multicenter cross-sectional study. Ophthalmology. 2015;122:925–33.
Lee KW, Kim JY, Chin HS, Seo KY, Kim T-i, Jung JW. Assessment of the tear meniscus by strip meniscometry and keratograph in patients with dry eye disease according to the presence of meibomian gland dysfunction. Cornea. 2016;36:189–95.
Sullivan DA, Rocha EM, Aragona P, Clayton JA, Ding J, Golebiowski B, et al. TFOS DEWS II Sex, Gender, and Hormones Report. Ocul Surf. 2017;15:284–333.
Gagliano C, Caruso S, Napolitano G, Malaguarnera G, Cicinelli MV, Amato R, et al. Low levels of 17-β-oestradiol, oestrone and testosterone correlate with severe evaporative dysfunctional tear syndrome in postmenopausal women: a case–control study. Br J Ophthalmol. 2014;98:371–6.
Health Pathology N. Fact Sheet: Sensitive Oestradiol 2018. [http://www.seals.health.nsw.gov.au/SiteFiles/sesiahshealthnswgovau/Sensitive_Oestradiol_Fact_Sheet_Jan_2018_-_01.pdf.
Peck T, Olsakovsky L, Aggarwal S. Dry eye syndrome in menopause and perimenopausal age group. J Life Health. 2017;8:51.
Ablamowicz AF, Nichols JJ, Nichols KK. Association between serum levels of testosterone and estradiol with meibomian gland assessments in postmenopausal women. Investig Ophthalmol Vis Sci. 2016;57:295–300.
Labrie F, Luu-The V, Labrie C, Bélanger A, Simard J, Lin S-X, et al. Endocrine and intracrine sources of androgens in women: inhibition of breast cancer and other roles of androgens and their precursor dehydroepiandrosterone. Endocr Rev. 2003;24:152–82.
Acknowledgements
The authors acknowledge Hannah Ahern and Mittra Rahimi-Oztan for their assistance in the study.
Funding
Pauline Khoo is supported by an Australian Government Training Program Scholarship and the Ophthalmology and Vision Science PhD Scholarship from the University of Sydney, Australia. Frances Boyle and Benjamin Forster are supported by the Friends of the Mater Foundation. The study was supported by the Ophthalmic Research Institute of Australia.
Author information
Authors and Affiliations
Contributions
PK was responsible for designing the study protocol, obtaining ethics approval, writing the protocol, patient recruitment, performing clinical assessments, data collection and analysing data, interpreting results and writing the paper. TG was responsible for performing clinical assessment on patients. FB was responsible for providing feedback on the study protocol, patient recruitment, data collection and providing feedback on the paper. SO and BF were responsible for patient recruitment, data collection and providing feedback on paper. SLW was responsible for designing the study protocol, interpreting results and providing feedback on the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khoo, P., Groeneveld, T., Boyle, F. et al. Dry eye signs and symptoms in patients on aromatase inhibitor therapy. Eye 36, 766–772 (2022). https://doi.org/10.1038/s41433-021-01538-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-021-01538-6