Abstract
Objectives
To investigate the results of partial lamellar sclerouvectomy (PLSU) for anteriorly located uveal tumours.
Methods
We reviewed the tumour features, histopathologic findings, complications, visual acuity outcomes, eye preservation, metastasis, and mortality data of 56 cases with uveal tumours who underwent PLSU between February 1999 and February 2019.
Results
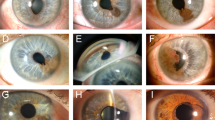
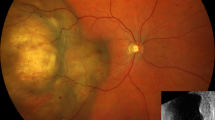
The mean largest tumour base diameters were 5.8 × 3.4 mm and the mean tumour thickness was 3.3 mm. Histopathologically, 30 (53.6%) eyes had malignant melanoma, 13 (23.2%) had nevus, 5 (8.9%) had iris stromal cyst, 4 (7.1%) had melanocytoma, 2 (3.6%) had Fuchs’ adenoma, 1 (1.8%) had iris pigment epithelial cyst, and 1 (1.8%) had invasive breast cancer metastasis. The most common postoperative complications included cataract in 21 (37.5%) eyes, vitreous haemorrhage in 15 (26.8%), scleral thinning in 10 (17.9%), and hyphema in 6 (10.7%). At a mean follow-up of 40.4 (range: 10–201) months, tumour recurrence was observed in 2/30 (6.7%) eyes with melanoma and 1/5 (20.0%) eye with iris stromal cyst. Eyes with recurrent melanoma were treated with enucleation. Liver metastasis developed in only 1 (3.3%) melanoma case. All patients were alive at the end of follow-up.
Conclusions
PLSU is a successful treatment method for many anteriorly located uveal tumours. In our series, the overall tumour recurrence and globe salvage rates were 5.4% and 96.4% respectively. Among melanoma cases, the metastasis rate was 3.3% and survival rate was 100%.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Gündüz K, Bechrakis NE. Exoresection and endoresection for uveal melanoma. Middle East Afr J Ophthalmol. 2010;17:210–6.
Damato BE. Local resection of uveal melanoma. Dev Ophthalmol. 2012;49:66–80.
Konstantinidis L, Groenewald C, Coupland SE, Damato B. Trans-scleral local resection of toxic choroidal melanoma after proton beam radiotherapy. Br J Ophthalmol. 2014;98:775–9.
Shields JA, Shields CL, Shah P, Sivalingam V. Partial lamellar sclerouvectomy for ciliary body and choroidal tumours. Ophthalmology. 1991;98:971–83.
Damato BE. Local resection of uveal melanoma. Bull Soc Belg Ophtalmol. 1993;248:11–7.
Peyman GA, Juarez CP, Diamond JG, Raichand M. Ten years experience with eye wall resection for uveal malignant melanomas. Ophthalmology. 1984;91:1720–5.
Naumann GO, Rummelt V. Block excision of tumours of the anterior uvea. Report on 68 consecutive patients. Ophthalmology. 1996;103:2017–27. 2027–8 discussion.
Shields JA, Shields CL. Surgical approach to lamellar sclerouvectomy for posterior uveal melanomas: the 1986 Schoenberg lecture. Ophthalmic Surg. 1988;19:774–80.
Kurt RA, Gündüz K. Exoresection via partial lamellar sclerouvectomy approach for uveal tumours: a successful performance by a novice surgeon. Clin Ophthalmol. 2010;4:59–65.
Damato B, Foulds WS. Indications for trans-scleral local resection of uveal melanoma. Br J Ophthalmol. 1996;80:1029–30.
Lee CS, Rim TH, Kwon HJ, Yi JH, Lee SC. Partial lamellar sclerouvectomy of ciliary body tumours in a Korean population. Am J Ophthalmol. 2013;156:36–42.e1.
Ramasubramanian A, Shields CL, Kytasty C, Mahmood Z, Shah SU, Shields JA. Resection of intraocular tumours (partial lamellar sclerouvectomy) in the pediatric age group. Ophthalmology. 2012;119:2507–13.
Char DH, Miller T, Crawford JB. Uveal tumour resection. Br J Ophthalmol. 2001;85:1213–9.
Elizalde J, Ubia S, Barraquer RI. Adenoma of the nonpigmented ciliary epithelium. Eur J Ophthalmol. 2006;16:630–3.
Ishiahara K, Hashida N, Asao K, Usui S, Maruyama K, Nishida K. Rare histological type of adenoma of the nonpigmented ciliary epithelium. Case Rep Ophthalmol. 2019;10:75–80.
Biswas J, Kumar SK, Gopal L, Bhende MP. Leiomyoma of the ciliary body extending to the anterior chamber: clinicopathologic and ultrasound biomicroscopic correlation. Surv Ophthalmol. 2000;44:336–42.
Palamar M, Shields CL, Marr BP, Eagle RC Jr, Shields JA. Retinal pigment epithelial tumour in a young Asian female. Eur J Ophthalmol. 2009;19:487–9.
Yan J, Liu X, Zhang P, Li Y. Acquired adenoma of the nonpigmented ciliary epithelium: analysis of five cases. Graefes Arch Clin Exp Ophthalmol. 2015;253:637–44.
Kaliki S, Shields CL, Eagle RC Jr, Vemuganti GK, Almeida A, Manjandavida FP, et al. Ciliary body medulloepithelioma: analysis of 41 cases. Ophthalmology. 2013;120:2552–9.
Lindquist TD. Capsulorhexis, phacoemulsification, and posterior chamber lens placement following iridocyclectomy. Ophthalmic Surg. 1992;23:44–6.
Histopathologic characteristics of uveal melanomas in eyes enucleated from the Collaborative Ocular Melanoma Study. COMS report no. 6. Am J Ophthalmol. 1998;125:745–66.
Kim JW, Damato BE, Hiscott P. Noncontiguous tumour recurrence of posterior uveal melanoma after transscleral local resection. Arch Ophthalmol. 2002;120:1659–64.
Damato BE, Paul J, Foulds WS. Risk factors for residual and recurrent uveal melanoma after trans-scleral local resection. Br J Ophthalmol. 1996;80:102–8.
Fabian ID, Thaung C, AlHarby L, Sisley K, Mudhar HS, Doherty RE, et al. Late solitary extraocular recurrence from previously resected ıris melanoma. Am J Ophthalmol. 2017;181:97–105.
Damato B. Adjunctive plaque radiotherapy after local resection of uveal melanoma. Front Radiat Ther Oncol. 1997;30:123–32.
Willerding GD, Cordini D, Moser L, Krause L, Foerster MH, Bechrakis NE. Neoadjuvant proton beam irradiation followed by transscleral resection of uveal melanoma in 106 cases. Br J Ophthalmol. 2016;100:463–7.
Damato BE, Paul J, Foulds WS. Risk factors for metastatic uveal melanoma after trans-scleral local resection. Br J Ophthalmol. 1996;80:109–16.
Bechrakis NE, Petousis V, Willerding G, Krause L, Wachtlin J, Stroux A, et al. Ten-year results of transscleral resection of large uveal melanomas: local tumour control and metastatic rate. Br J Ophthalmol. 2010;94:460–6.
Augsburger JJ, Lauritzen K, Gamel JW, DeBrakeleer DJ, Lowry JC, Eisenman R. Matched group study of surgical resection versus cobalt-60 plaque radiotherapy for primary choroidal or ciliary body melanoma. Ophthalmic Surg. 1990;21:682–8.
Acknowledgements
The authors acknowledge Hatice Kaykusuz, MD from the Anaesthesiology Department, Ankara University Faculty of Medicine and Funda Seher Özalp Ateş, Msc from the Biostatistics Department, Ankara University Faculty of Medicine for their contributions in the preparation of the paper. There are no sources of support including sponsorship (e.g. university, charity, commercial organisation) and sources of material (e.g. novel drugs) not available commercially.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mirzayev, I., Gündüz, A.K. & Okçu Heper, A. Partial lamellar sclerouvectomy surgery for anteriorly located uveal tumour resection: a 20-year experience. Eye 36, 969–977 (2022). https://doi.org/10.1038/s41433-021-01545-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-021-01545-7
This article is cited by
-
Local resection via partial lamellar sclerouvectomy for ciliary body tumors — a case series
BMC Ophthalmology (2024)