Abstract
Objectives
To evaluate the ocular surface, meibomian glands and corneal structural changes using in vivo confocal microscopy (IVCM) in patients receiving aromatase inhibitor (AI) therapy due to the breast cancer.
Methods
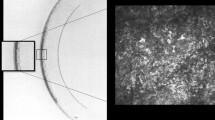
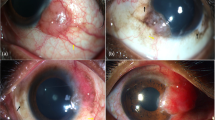
This prospective observational study included 13 patients undergoing AI therapy. The patients were evaluated before the treatment, at 3- and 6-month timepoints of AI therapy. To examine the ocular surface and tear film, corneal sensitivity (CS) measurement with Cochet–Bonnet Aesthesiometer, tear film break-up time (TBUT), lissamine green (LG) staining, Schirmer I test with anaesthesia (ST) and the ocular-surface disease index (OSDI) questionnaire were performed consecutively. Corneal cell densities and sub-basal nerve plexus were evaluated with IVCM (ConfoScan 4, Nidek, Japan). Finally, quantitative MG drop-out assessment was made using infrared meibography. Shapiro Wilk, Friedman’s and Post-hoc Dunn tests were used for the statistical analysis.
Results
TBUT, ST scores, basal epithelium, anterior and posterior keratocytes and endothelial cell densities, long and total sub-basal nerve densities were found to be decreased (p < 0.001, p = 0.023, p < 0.001, p = 0.01, p = 0.002, p = 0.004, p < 0.001, p < 0.001), and meiboscore, CS, OSDI scores and sub-basal nerve tortuosity values were increased (p < 0.001, p = 0.015, p = 0.001, p = 0.004) during the treatment. Endothelial pleomorphism rates were lower at the 3- and 6-month timepoints compared to before the treatment (p = 0.04).
Conclusion
This study showed that aromatase inhibitor therapy causes deteriorations in many of the ocular-surface parameters and corneal structural changes in relation with the duration of treatment. These patients should be observed during the therapy in terms of the ocular-surface side effects.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Lonning PE. The potency and clinical efficacy of aromatase inhibitors across the breast cancer continuum. Ann Oncol. 2011;22:503–14.
Tomao F, Spinelli G, Vici P, Pisanelli GC, Cascialli G, Frati L, et al. Current role and safety profile of aromatase inhibitors in early breast cancer. Expert Rev Anticancer Ther. 2011;11:1253–63.
Chatziralli I, Sergentanis T, Zagouri F, Chrysikos D, Ladas I, Zografos GC, et al. Ocular surface disease in breast cancer patients using aromatase inhibitors. Breast J. 2016;22:561–3.
Ogueta SB, Schwartz SD, Yamashita CK, Farber DB. Estrogen receptor in the human eye: influence of gender and age on gene expression. Invest Ophthalmol Vis Sci. 1999;40:1906–11.
Munaut C, Lambert V, Noel A, Frankenne F, Deprez M, Foidart JM, et al. Presence of oestrogen receptor type beta in human retina. Br J Ophthalmol. 2001;85:877–82.
Elliot SJ, Catanuto P, Espinosa-Heidmann DG, Fernandez P, Hernandez E, Saloupis P, et al. Estrogen receptor beta protects against in vivo injury in RPE cells. Exp Eye Res. 2010;90:10–16.
Eisner A, Falardeau J, Toomey MD, Vetto JT. Retinal hemorrhages in anastrozole users. Optom Vis Sci. 2008;85:301–8.
Karagoz B, Ayata A, Bilgi O, Uzun G, Unal M, Kandemir EG, et al. Hemicentral retinal artery occlusion in a breast cancer patient using anastrozole. Onkologie. 2009;32:421–3.
Eisner A, Thielman EJ, Falardeau J, Vetto JT. Vitreo-retinal traction and anastrozole use. Breast Cancer Res Treat. 2009;117:9–16.
Sathiamoorthi S, Ruddy KJ, Bakri SJ. Association of uveitis and macular edema with anastrozole therapy. JAMA Ophthalmol. 2018;136:837–9.
Schaumberg DA, Buring JE, Sullivan DA, Dana MR. Hormone replacement therapy and dry eye syndrome. JAMA. 2001;286:2114–9.
Affinito P, Di Spiezio Sardo A, Di Carlo C, Sammartino A, Tommaselli GA, Bifulco G, et al. Effects of hormone replacement therapy on ocular function in postmenopause. Menopause. 2003;10:482–7.
Berman ER. Tears. In: Biochemistry of the Eye. Boston: Springer US; 1991. p. 63–88.
Davison SL, Bell R, Donath S, Montalto JG, Davis SR. Androgen levels in adult females: changes with age, menopause, and oophorectomy. J Clin Endocrinol Metab. 2005;90:3847–53.
Rizner TL, Thalhammer T, Ozvegy-Laczka C. The importance of steroid uptake and intracrine action in endometrial and ovarian cancers. Front Pharmacol. 2017;8:346.
Labrie F, Belanger A, Luu-The V, Labrie C, Simard J, Cusan L, et al. DHEA and the intracrine formation of androgens and estrogens in peripheral target tissues: its role during aging. Steroids. 1998;63:322–8.
Sullivan DA, Rocha EM, Aragona P, Clayton JA, Ding J, Golebiowski B, et al. TFOS DEWS II Sex, Gender, and Hormones Report. Ocul Surf. 2017;15:284–333.
Versura P, Giannaccare G, Campos EC. Sex-steroid imbalance in females and dry eye. Curr Eye Res. 2015;40:162–75.
Sullivan DA, Sullivan BD, Ullman MD, Rocha EM, Krenzer KL, Cermak JM, et al. Androgen influence on the meibomian gland. Invest Ophthalmol Vis Sci. 2000;41:3732–42.
Sullivan DA, Rocha EM, Ullman MD, Kreuzer KL, Gao J, Toda I et al. Androgen Regulation of the Meibomian Gland. In: Sullivan DA, Dartt DA, Meneray MA (eds). Lacrimal Gland, Tear Film, and Dry Eye Syndromes 2: Basic Science and Clinical Relevance. Boston: Springer US; 1998. p. 327–31.
Liu M, Richards SM, Schirra F, Yamagami H, Sullivan BD, Sullivan DA. Identification of androgen-regulated genes in the lacrimal gland. Adv Exp Med Biol. 2002;506:129–35.
Smith RE. The tear film complex: pathogenesis and emerging therapies for dry eyes. Cornea. 2005;24:1–7.
Inglis H, Boyle FM, Friedlander ML, Watson SL. Dry eyes and AIs: If you don’t ask you won’t find out. Breast. 2015;24:694–8.
Turaka K, Nottage JM, Hammersmith KM, Nagra PK, Rapuano CJ. Dry eye syndrome in aromatase inhibitor users. Clin Exp Ophthalmol. 2013;41:239–43.
Methodologies to diagnose and monitor dry eye disease: report of the Diagnostic Methodology Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007;5:108–52.
Irkec MT, Group TOS. Reliability and validity of Turkish translation of the ocular surface disease index (OSDI) in dry eye syndrome. Invest Ophthalmol Vis Sci. 2007;48:408–408.
Pult H, Riede-Pult B. Comparison of subjective grading and objective assessment in meibography. Cont Lens Anterior Eye. 2013;36:22–27.
Burstein HJ, Prestrud AA, Seidenfeld J, Anderson H, Buchholz TA, Davidson NE, et al. American Society of Clinical Oncology clinical practice guideline: update on adjuvant endocrine therapy for women with hormone receptor-positive breast cancer. J Clin Oncol. 2010;28:3784–96.
Spelsberg H, Klueppel M, Reinhard T, Glaeser M, Niederacher D, Beckmann MW, et al. Detection of oestrogen receptors (ER) alpha and beta in conjunctiva, lacrimal gland, and tarsal plates. Eye (Lond). 2004;18:729–33.
Song X, Zhao P, Wang G, Zhao X. The effects of estrogen and androgen on tear secretion and matrix metalloproteinase-2 expression in lacrimal glands of ovariectomized rats. Invest Ophthalmol Vis Sci. 2014;55:745–51.
Krenzer KL, Dana MR, Ullman MD, Cermak JM, Tolls DB, Evans JE, et al. Effect of androgen deficiency on the human meibomian gland and ocular surface. J Clin Endocrinol Metab. 2000;85:4874–82.
Cuzick J, Sestak I, Forbes JF, Dowsett M, Knox J, Cawthorn S, et al. Anastrozole for prevention of breast cancer in high-risk postmenopausal women (IBIS-II): an international, double-blind, randomised placebo-controlled trial. Lancet. 2014;383:1041–8.
Gibson E, Stapleton F, Dear R, Wolffsohn JS, Golebiowski B. Dry eye signs and symptoms in aromatase inhibitor treatment and the relationship with pain. Ocul Surf. 2020;18:108–13.
Suzuki T, Schirra F, Richards SM, Jensen RV, Sullivan DA. Estrogen and progesterone control of gene expression in the mouse meibomian gland. Invest Ophthalmol Vis Sci. 2008;49:1797–808.
Kam W, Sullivan D. Suppressive effects of 17β-estradiol on immortalized human meibomian gland epithelial cells. Invest Ophthalmol Vis Sci. 2013;54:4316–4316.
Darabad RR, Suzuki T, Richards SM, Jensen RV, Jakobiec FA, Zakka FR, et al. Influence of aromatase absence on the gene expression and histology of the mouse meibomian gland. Invest Ophthalmol Vis Sci. 2013;54:987–98.
Tong L, Gupta PK. Need for animal models of meibomian gland dysfunction. Ophthalmol Ther. 2016;5:129–34.
Sacchetti M, Lambiase A. Diagnosis and management of neurotrophic keratitis. Clin Ophthalmol. 2014;8:571–9.
Cai D, Zhu M, Petroll WM, Koppaka V, Robertson DM. The impact of type 1 diabetes mellitus on corneal epithelial nerve morphology and the corneal epithelium. Am J Pathol. 2014;184:2662–70.
Benitez-Del-Castillo JM, Acosta MC, Wassfi MA, Diaz-Valle D, Gegundez JA, Fernandez C, et al. Relation between corneal innervation with confocal microscopy and corneal sensitivity with noncontact esthesiometry in patients with dry eye. Invest Ophthalmol Vis Sci. 2007;48:173–81.
Labbe A, Alalwani H, Van Went C, Brasnu E, Georgescu D, Baudouin C. The relationship between subbasal nerve morphology and corneal sensation in ocular surface disease. Invest Ophthalmol Vis Sci. 2012;53:4926–31.
Steger B, Speicher L, Philipp W, Bechrakis NE. In vivo confocal microscopic characterisation of the cornea in chronic graft-versus-host disease related severe dry eye disease. Br J Ophthalmol. 2015;99:160–5.
Zhang X, Chen Q, Chen W, Cui L, Ma H, Lu F. Tear dynamics and corneal confocal microscopy of subjects with mild self-reported office dry eye. Ophthalmology. 2011;118:902–7.
Belmonte C, Nichols JJ, Cox SM, Brock JA, Begley CG, Bereiter DA, et al. TFOS DEWS II pain and sensation report. Ocul Surf. 2017;15:404–37.
Tachibana M, Kasukabe T, Kobayashi Y, Suzuki T, Kinoshita S, Matsushima Y. Expression of estrogen receptor alpha and beta in the mouse cornea. Invest Ophthalmol Vis Sci. 2000;41:668–70.
Tachibana M, Kobayashi Y, Kasukabe T, Kawajiri K, Matsushima Y. Expression of androgen receptor in mouse eye tissues. Invest Ophthalmol Vis Sci. 2000;41:64–66.
Suzuki T, Kinoshita Y, Tachibana M, Matsushima Y, Kobayashi Y, Adachi W, et al. Expression of sex steroid hormone receptors in human cornea. Curr Eye Res. 2001;22:28–33.
Hadeyama T, Nakayasu K, Ha NT, Nakamura S. Expression of estrogen receptors alpha and beta, androgen receptors and progesterone receptors in human cornea. Nippon Ganka Gakkai Zasshi. 2002;106:557–64.
Wickham LA, Gao J, Toda I, Rocha EM, Ono M, Sullivan DA. Identification of androgen, estrogen and progesterone receptor mRNAs in the eye. Acta Ophthalmol Scand. 2000;78:146–53.
Acknowledgements
This work was presented in part at the 52nd Turkish Ophthalmological Association National Congress (November,13-18,2018, Antalya, Turkey).
Funding
This study was funded by the authors and did not receive any grant from finance agencies in the public or commercial sectors.
Author information
Authors and Affiliations
Contributions
Design of the study: SK, MI; data collection: AA, AYG, SA; analysis and interpretation: AA, SK, JK, MI; manuscript preparation: AA, SK, MI; critical appraisal of the manuscript: SK, MI
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ağın, A., Kocabeyoglu, S., Yucel Gencoglu, A. et al. The effects of systemic aromatase inhibitors on meibomian glands and corneal structure. Eye 36, 1185–1193 (2022). https://doi.org/10.1038/s41433-021-01612-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-021-01612-z
This article is cited by
-
Corneal changes in estrogen-dependent breast cancer after hormonal treatment
Scientific Reports (2025)