Abstract
Introduction
As gonococcal infections continue to increase, we wanted to review the number and clinical course of recent ocular gonococcal cases presenting to ophthalmology departments in NHS Greater Glasgow and Clyde.
Methods
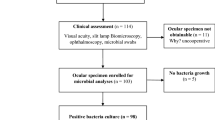
A 5-year retrospective review of adult ocular gonococcal cases, where the diagnosis of Neisseria gonorrhoeae was made on microbiological culture, was undertaken.
Results
Fifteen cases were identified (80% male). Average age was 26 years (range 17–42; median 24). Most common presenting features included purulent discharge (14/15; 93%), haemorrhagic conjunctivitis (10/15; 67%) and pre-septal cellulitis (9/15; 60%). Corneal involvement was documented in 5 (33%), with marginal ulceration in 1 (7%) but none had corneal perforation. Most common systemic treatment was IV ceftriaxone, alone or in combination with another antibiotic (6/15; 40%), followed by IM ceftriaxone, alone or in combination with another antibiotic (5/15; 33%). Median time from presentation to treatment was 1 day (0–23). All patients were referred or recommended to attend sexual health services. Seven patients (47%) attended and received complete sexually transmitted infection (STI) testing and contact tracing: 3 patients had systemic treatment initiated or changed at this visit and 1 patient had concurrent syphilis identified.
Conclusions
This series confirms purulent conjunctivitis and cellulitis as the main presenting features of ocular gonococcal infection requiring hospital review. Early identification with appropriate systemic antibiotic treatment avoided corneal melting in this cohort. As concurrent STIs were identified and/or treatments changed in 4/7 (57%) following sexual health review, we recommend a shared care approach between ophthalmology, microbiology and sexual health services to effectively address all management issues.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Health Protection Scotland. Diagnosis of STIs continues to rise in Scotland. 2019. https://www.hps.scot.nhs.uk/publications/hps-weekly-report/volume-53/issue-21/diagnoses-of-stis-continue-to-rise-in-scotland/#:~:text=Two%20reports%20published%20by%20Health%20Protection%20Scotland%20%28HPS%29,2018%2C%20specifically%20genital%20chlamydia%2C%20gonorrhoea%20and%20infectious%20syphilis. Accessed 18 September 2020.
Public Health England. Heath matters: preventing STIs. 2019. https://www.gov.uk/government/publications/health-matters-preventing-stis/health-matters-preventing-stis. Accessed 18 September 2020.
Public Health England. STI diagnoses and rates in England by gender, 2010–2019. 2020. https://www.gov.uk/government/statistics/sexually-transmitted-infections-stis-annual-data-tables. Accessed 18 September 2020.
Health Protection Scotland. Genital chlamydia and gonorrhoea infections in Scotland: laboratory diagnosis in Scotland 2010–2019. https://hpspubsrepo.blob.core.windows.net/hps-website/nss/3073/documents/1_genital-chlamydia-gonorrhoea-scotland-2010-2019-summary.pdf. Accessed 18 September 2020.
Miller K.E. Diagnosis and treatment of Neisseria gonorrhoeae infections. Am Fam Physician. 2006;73:1779–784.
Centers for Disease Control and Prevention. Gonorrhoea – CDC Factsheet. 2019. https://www.cdc.gov/std/gonorrhea/stdfact-gonorrhea-detailed.htm. Accessed 18 September 2020.
Stenberg K, Mardh PA. Chlamydial conjunctivitis in neonates and adults. History, clinical findings, and follow-up. Acta Ophthalmol 1990;68:651–7.
Lee JS, Choi HY, Lee JE, Lee SH, Oum BS. Gonococcal keratoconjunctivitis in adults. Eye 2002;16:646–9.
McElnea E, Stapleton P, Kahn S, Stokes J, Higgins G. Challenges in the management of Neisseria gonorrhoeae keratitis. Int Ophthalmol 2015;35:135–40.
Wan WL, Farkas GC, May WN, Robin JB. The clinical characteristics and course of adult gonococcal conjunctivitis. Am J Ophthalmol 1986;102:575–83.
McAnena L, Knowels SJ, Curry A, Cassidy L. Prevelance of gonococcal conjunctivitis in adults and neonates. Eye 2015;29:875–80.
Kawashima M, Kawakita T, Den S, Tomita M, Shimazaki J. Surgical management of corneal perforation secondary to gonococcal keratoconjunctivitis. Eye 2009;23:339–44.
Tipple C, Smith A, Bakowska E, Corbett MC. Corneal perforation requiring corneal grafting: a rare complication of gonococcal eye infection. Sex Transm Infect 2010;86:447–8.
Centers for Disease Control and Prevention. 2015 Sexually transmitted diseases treatment guidelines. 2015. https://www.cdc.gov/std/tg2015/gonorrhea.htm. Accessed 24 September 2020.
BASHH. Coordinated response to restrain further spread of azithromycin resistant gonorrhoea. 2016. https://www.bashh.org/news/news/bashh-calls-for-coordinated-response-to-restrain-further-spread-of-azithromycin-resistant-gonorrhoea/. Accessed 24 September 2020.
Fifer H, Saunders J, Soni S, Sadiq ST, FitzGerald M. 2018 National UK guideline for management of infection with Neisseria gonorrhoeae. Int J STD AIDS 2020;31:4–15.
Day AC, Ramkissoon YD, George S, Corbett MC. Don’t forget Gonococcus! Eye 2006;20:1400–2.
Sevilla N, Martin S, Serr-Pladevall J, Kirkegaard E, Bisbe L, Puig JJ. Delay in diagnosis resulting in corneal perforation: nucleic acid amplification tests for a rapid identification of ocular Neisseria gonorrhoeae infection. Sex Transm Infect 2020;96:562.
Public Health England. SMIB2: investigations of bacterial eye infections. 2017. https://www.gov.uk/government/publications/smi-b-2-investigation-of-eye-swabs-and-canalicular-pus. Accessed 6 December 2020.
Nusbaum MRH, Wallace RR, Slatt LM, Kondrad EC. Sexually transmitted infections and increased risk of co-infection with human immunodeficiency virus. J Am Osteopath Assoc 2004;104:527–35.
Rothschild P, Sherwin J, Chen Y, Wells K, Crock C. Has the increasing incidence of chlamydia and gonorrhoea resulted in increased chlamydial and gonococcal conjunctivitis presentations? Results from Melbourne, Australia, from 2000 to 2017. Clin Exp Ophthalmol 2019;47:289–91.
Hegde V, Smith G, Choi J, Pagliarini S. A case of gonococcal kerato-conjunctivitis mimicking orbital cellulitis. Acta Ophthalmol Scand 2005;83:511–2.
Ullman S, Roussel TJ, Culbertson WW, Forster RK, Alfonso E, Mendelsohn AD, et al. Neisseria gonorrhoeae keratoconjunctivitis. Ophthalmology 1987;94:525–31.
Duke-Elder S, editor. System of ophthalmology. Vol. 8. Part 1. Diseases of the outer eye. CV Mosby Co.; 1965. p. 167–74.
Tong L, Tan DT, Abańo JM, Lim L. Deep anterior lamellar keratoplasty in a patient with descemetocele following gonococcal keratitis. Am J Ophthalmol 2004;138:506–7.
Samira N, Bani AP, Susiyanti M. Rare case of bilateral perforated corneal ulcer due to gonococcal infection, managed with temporary periosteal graft. BMJ Case Rep. 2016. https://doi.org/10.1136/bcr-2015-213547
Bastion ML, Prakash K, Siow YC, Loh SS. Bilateral corneal perforation in a sexually active adult male with gonococcal conjunctivitis. Med J Malaysia 2006;61:366–8.
Lockington D, MacDonald R, King S, Weir C, Winter A, Aitken C. Multiplex PCR testing requires a robust multi-disciplinary strategy to effectively manage identified cases of chlamydial conjunctivitis. Scott Med J 2013;58:77–82.
Shah M, Gishkori S, Edington M, King S, Winter A, Lockington D. Ten-year review of a shared care approach in the management of ocular Chlamydia trachomatis infections. Eye . 2021;35:1614–9. https://doi.org/10.1038/s41433-020-01128-y.
Acknowledgements
A version of this paper was an oral presentation at the UK Bowman Club meeting in March 2021 and a poster at the Virtual Annual Congress of the Royal College of Ophthalmologists in May 2021.
Author information
Authors and Affiliations
Contributions
D.L. had the original idea. L.B. and M.S. performed the data collection, initial literature review and drafted the article. L.C., A.W. and D.L. provided direction and senior support, additional literature input and revised the article into the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Permission for image publication: Granted and consent obtained
Rights and permissions
About this article
Cite this article
Butler, L., Shah, M., Cottom, L. et al. Five-year review of ocular Neisseria gonorrhoeae infections presenting to ophthalmology departments in Greater Glasgow & Clyde, Scotland. Eye 36, 1442–1447 (2022). https://doi.org/10.1038/s41433-021-01658-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-021-01658-z