Abstract
Purpose
To compare the progression of posterior vitreous detachment (PVD) between eyes that underwent cataract surgery and eyes that did not undergo surgery in non-highly myopic patients.
Methods
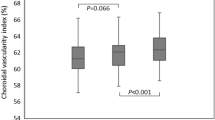
One-hundred twenty-five eyes of 125 patients scheduled for phacoemulsification and 125 eyes of 125 age-matched patients who did not undergo surgery were enrolled. PVD status was evaluated using swept-source optical coherence tomography at 2 days (baseline), and 1, 3, 6, and 12 months postoperatively, and classified into five stages: 0 (no), 1 (paramacular), 2 (perifoveal), 3 (peripapillary), and 4 (complete). The PVD stage and incidence of progression to complete PVD were compared between groups.
Results
The mean PVD stage significantly progressed over the 12 months in the surgery group (P = 0.0004), but did not change significantly in the non-surgery group. The PVD stage did not differ significantly between groups at 2 days, or 1, 3, and 6 months postoperatively, but was significantly more progressed in the surgery group than in the non-surgery group at 12 months (P = 0.0390). After adjusting for age, sex, axial length, and baseline PVD stage, the relative risk for progression to complete PVD was 7.1-fold higher in the surgery group than in the non-surgery group (P < 0.0001, 95% confidence interval 2.9–17.3).
Conclusion
PVD progressed significantly faster in eyes after cataract surgery compared with eyes that did not undergo surgery, and the relative risk of progression to complete PVD was approximately seven-fold higher within 1 year, indicating that the risk for PVD-related diseases is high after cataract surgery.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Bond-Taylor M, Jakobsson G, Zetterberg M. Posterior vitreous detachment – prevalence of and risk factors for retinal tears. Clin Ophthalmol. 2017;11:1689–95.
Gishti O, van den Nieuwenhof R, Verhoekx J, van Overdam K. Symptoms related to posterior vitreous detachment and the risk of developing retinal tears: a systematic review. Acta Ophthalmol. 2019;97:347–52.
Sarrafizadeh R, Hassan TS, Ruby AJ, Williams GA, Garretson BR, Capone A Jr, et al. Incidence of retinal detachment and visual outcome in eyes presenting with posterior vitreous separation and dense fundus-obscuring vitreous hemorrhage. Ophthalmology. 2001;108:2273–8.
Byer NE. Natural history of posterior vitreous detachment with early management as the premier line of defense against retinal detachment. Ophthalmology. 1994;101:1503–14.
Mitry D, Singh J, Yorston D, Siddiqui MA, Wright A, Fleck BW, et al. The predisposing pathology and clinical characteristics in the Scottish retinal detachment study. Ophthalmology. 2011;118:1429–34.
Johnson MW, Van Newkirk MR, Meyer KA. Perifoveal vitreous detachment is the primary pathogenic event in idiopathic macular hole formation. Arch Ophthalmol. 2001;119:215–22.
La Cour M, Friis J. Macular holes: classification, epidemiology, natural history and treatment. Acta Ophthalmol Scand. 2002;80:579–87.
Yamada N, Kishi S. Tomographic features and surgical outcomes of vitreomacular traction syndrome. Am J Ophthalmol. 2005;139:112–7.
Ripandelli G, Coppé AM, Parisi V, Olzi D, Scassa C, Chiaravalloti A, et al. Posterior vitreous detachment and retinal detachment after cataract surgery. Ophthalmology. 2007;114:692–7.
Mirshahi A, Höhn F, Lorenz K, Hattenbach LO. Incidence of posterior vitreous detachment after cataract surgery. J Cataract Refract Surg. 2009;35:987–91.
Ivastinovic D, Schwab C, Borkenstein A, Lackner EM, Wedrich A, Velikay-Parel M. Evolution of early changes at the vitreoretinal interface after cataract surgery determined by optical coherence tomography and ultrasonography. Am J Ophthalmol. 2012;153:705–9.
Degirmenci C, Afrashi F, Mentes J, Oztas Z, Nalcaci S, Akkin C. Evaluation of posterior vitreous detachment after uneventful phacoemulsification surgery by optical coherence tomography and ultrasonography. Clin Exp Optom. 2017;100:49–53.
Otsuka Y, Ooto S, Yoshimura N. Changes in the posterior vitreous after cataract surgery assessed by swept-source optical coherence tomography. Retin Cases Brief Rep. 2019;13:227–31.
Park JH, Yang H, Kwon H, Jeon S. Risk factors for onset or progression of posterior vitreous detachment at the vitreomacular interface after cataract surgery. Ophthalmol Retin. 2021;5:270–8.
Hayashi K, Yoshida M, Hayashi S, Yoshimura K. Short-term changes in prediction error after cataract surgery in eyes receiving 1 of 3 types of single-piece acrylic intraocular lenses. Am J Ophthalmol. 2020;219:12–20.
Hayashi K, Sato T, Manabe SI, Hirata A. Sex-related differences in the progression of posterior vitreous detachment with age. Ophthalmol Retin. 2019;3:237–43.
Hayashi K, Manabe SI, Hirata A, Yoshimura K. Posterior vitreous detachment in highly myopic patients. Invest Ophthalmol Vis Sci. 2020;61:33.
Itakura H, Kishi S. Evolution of vitreomacular detachment in healthy subjects. JAMA Ophthalmol. 2013;131:1348–52.
Kakehashi A, Takezawa M, Akiba J. Classification of posterior vitreous detachment. Clin Ophthalmol. 2014;8:1–10.
Tsukahara M, Mori K, Gehlbach PL, Mori K. Posterior vitreous detachment as observed by wide-angle OCT imaging. Ophthalmology. 2018;125:1372–83.
Stirpe M, Heimann K. Vitreous changes and retinal detachment in highly myopic eyes. Eur J Ophthalmol. 1996;6:50–58.
Arevalo JF, Ramirez E, Suarez E, Morales-Stopello J, Cortez R, Ramirez G, et al. Incidence of vitreoretinal pathologic conditions within 24 months after laser in situ keratomileusis. Ophthalmology. 2000;107:258–62.
Chan CK, Lawrence FC. Macular hole after laser in situ keratomileusis and photorefractive keratectomy. Am J Ophthalmol. 2001;131:666–7.
Crim N, Esposito E, Monti R, Correa LJ, Serra HM, Urrets-Zavalia JA. Myopia as a risk factor for subsequent retinal tears in the course of a symptomatic posterior vitreous detachment. BMC Ophthalmol. 2017;17:226.
Gaucher D, Haouchine B, Tadayoni R, Massin P, Erginay A, Benhamou N, et al. Long-term follow-up of high myopic foveoschisis: natural course and surgical outcome. Am J Ophthalmol. 2007;143:455–62.
Shimada N, Tanaka Y, Tokoro T, Ohno-Matsui K. Natural course of myopic traction maculopathy and factors associated with progression or resolution. Am J Ophthalmol. 2013;156:948–57.
Acknowledgements
The authors thank Koji Yonemoto, PhD (Ryukyu University, Naha, Japan) for statistical assistance.
Author information
Authors and Affiliations
Contributions
SH: study conception, study design, data analysis/interpretation of data, and writing and revising of the manuscript. MY: data acquisition and final approval. KH: study conception, study design, data acquisition, data analysis/interpretation of data, and writing and revising of the manuscript, and final approval. KT: study conception, study design, data analysis/interpretation of data, and final approval.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The Institutional Review Board of Hayashi Eye Hospital approved the study protocol.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Hayashi, S., Yoshida, M., Hayashi, K. et al. Progression of posterior vitreous detachment after cataract surgery. Eye 36, 1872–1877 (2022). https://doi.org/10.1038/s41433-021-01732-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-021-01732-6
This article is cited by
-
An applied study of phacoemulsification cataract surgery with the mortise and tenon limbal incision
Scientific Reports (2025)
-
Posterior vitreous detachment rates post-uncomplicated phacoemulsification surgery: a systematic review
International Ophthalmology (2024)
-
Posterior vitreous detachment after cataract surgery in eyes with high myopia: an optical coherence tomography study
Japanese Journal of Ophthalmology (2022)