Abstract
Background
Timely management of aphakic children is critical for the rehabilitation of adequate visual gain. This study aims to evaluate the long-term efficacy of scleral contact lenses in terms of visual outcomes, complications, and compliance in aphakic children.
Methods
Retrospective data review of children with congenital or acquired cataract, or subluxated crystalline lenses, who underwent lensectomy from 2004 to 2018 and who used scleral contact lenses for refractive correction. Collected data from the follow up period included recorded aphakic refraction and visual acuity, complications following scleral contact lens wear documented in the clinic and ophthalmic emergency room and compliance to lens wear according to parental feedback on every visit in the clinic.
Results
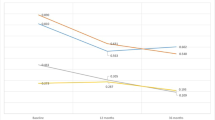
76% of cases, with final best corrected visual acuity (BCVA) of 20/40 or better achieved in seventeen eyes (34%). The rate of amblyopia was 50%. Strabismus developed in 56% of children, and those had less favourable visual outcomes (0.43 ± 0.4 LogMAR without strabismus and 0.8 ± 0.5 LogMAR with strabismus, p = 0.015). No corneal infections were documented during the follow up. Main adverse effect on the ocular surface was superficial punctate keratopathy (n = 16). Compliance was good in 48 children (96%)- except for two cases, the scleral lenses were tolerated well by all children.
Conclusion
Scleral contact lenses are an effective means of visual rehabilitation in aphakic children after lensectomy and may be used long-term with good compliance of wear, excellent visual outcomes, and tolerable adverse events.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Ceyhan D, Schnall BM, Breckenridge A, Fontanarosa J, Lehman SS, Calhoun JC. Risk factors for amblyopia in congenital anterior lens opacities. J AAPOS. 2005;9:537–41. https://doi.org/10.1016/j.jaapos.2005.09.001.
Mohammadpour M, Shaabani A, Sahraian A, Momenaei B, Tayebi F, Bayat R, et al. Updates on managements of pediatric cataract. J Curr Ophthalmol. 2018;31:118–26. https://doi.org/10.1016/j.joco.2018.11.005.
Wilson ME,Jr, Trivedi RH, Buckley EG, Granet DB, Lambert SR, Plager DA, et al. ASCRS white paper. Hydrophobic acrylic intraocular lenses in children. J Cataract Refract Surg. 2007;33:1966–73. https://doi.org/10.1016/j.jcrs.2007.06.047.
Birch EE, Cheng C, Stager DR,Jr, Felius J. Visual acuity development after the implantation of unilateral intraocular lenses in infants and young children. J AAPOS. 2005;9:527–32. https://doi.org/10.1016/j.jaapos.2005.07.008.
Plager DA, Lynn MJ, Buckley EG, Wilson ME, Lambert SR.Infant Aphakia Treatment Study Group. Complications, adverse events, and additional intraocular surgery 1 year after cataract surgery in the infant Aphakia Treatment Study. Ophthalmology. 2011;118:2330–4. https://doi.org/10.1016/j.ophtha.2011.06.017.
Plager DA, Yang S, Neely D, Sprunger D, Sondhi N. Complications in the first year following cataract surgery with and without IOL in infants and older children. J AAPOS. 2002;6:9–14. https://doi.org/10.1067/mpa.2002.121169.
Lambert SR, Lynn MJ, DuBois LG, Cotsonis GA, Hartmann EE, Wilson ME, Infant Aphakia Treatment Study G. Axial elongation following cataract surgery during the first year of life in the infant Aphakia Treatment Study. Invest Ophthalmol Vis Sci. 2012;53:7539–45. https://doi.org/10.1167/iovs.12-10285.
Autrata R, Rehurek J, Vodicková K. Visual results after primary intraocular lens implantation or contact lens correction for aphakia in the first year of age. Ophthalmologica. 2005;219:72–79. https://doi.org/10.1159/000083264.
Lambert SR, Lynn M, Drews-Botsch C, DuBois L, Wilson ME, Plager DA, et al. Intraocular lens implantation during infancy: perceptions of parents and the American Association for Pediatric Ophthalmology and Strabismus members. J AAPOS. 2003;7:400–5. https://doi.org/10.1016/j.jaapos.2003.08.004.
Lambert SR, Lynn MJ, Hartmann EE, DuBois L, Drews-Botsch C, Freedman SF.Infant Aphakia Treatment Study Group, et al. Comparison of contact lens and intraocular lens correction of monocular aphakia during infancy: a randomized clinical trial of HOTV optotype acuity at age 4.5 years and clinical findings at age 5 years. JAMA Ophthalmol. 2014;132:676–82. https://doi.org/10.1001/jamaophthalmol.2014.531.
Lambert SR, Kraker RT, Pineles SL, Hutchinson AK, Wilson LB, Galvin JA, et al. Contact lens correction of aphakia in children: a report by the American academy of ophthalmology. Ophthalmology. 2018;125:1452–8. https://doi.org/10.1016/j.ophtha.2018.03.014.
van der Worp E, Bornman D, Ferreira DL, Faria-Ribeiro M, Garcia-Porta N, González-Meijome JM. Modern scleral contact lenses: A review. Cont Lens Anterior Eye. 2014;37:240–50. https://doi.org/10.1016/j.clae.2014.02.002.
Saltarelli DP. Hyper oxygen-permeable rigid contact lenses as an alternative for the treatment of pediatric aphakia. Eye Contact Lens. 2008;34:84–93. https://doi.org/10.1097/ICL.0b013e31811eadaa.
Chen YC, Hu AC, Rosenbaum A, Spooner S, Weissman BA. Long-term results of early contact lens use in pediatric unilateral aphakia. Eye Contact Lens. 2010;36:19–25. https://doi.org/10.1097/ICL.0b013e3181c6dfdc.
Russell B, Ward MA, Lynn M, Dubois L, Lambert SR.Infant Aphakia Treatment Study Group. The infant aphakia treatment study contact lens experience: one-year outcomes. Eye Contact Lens. 2012;38:234–9. https://doi.org/10.1097/ICL.0b013e3182562dc0.
Mutti DO, Mitchell GL, Jones LA, Friedman NE, Frane SL, Lin WK, et al. Refractive astigmatism and the toricity of ocular components in human infants. Optom Vis Sci. 2004;81:753–61. https://doi.org/10.1097/00006324-200410000-00007.
Russell B, DuBois L, Lynn M, Ward MA, Lambert SR.Infant Aphakia Treatment Study Group. The infant aphakia treatment study contact lens experience to age 5 years. Eye Contact Lens. 2017;43:352–7. https://doi.org/10.1097/ICL.0000000000000291.
Chak M, Wade A, Rahi JS.British Congenital Cataract Interest Group. Long-term visual acuity and its predictors after surgery for congenital cataract: findings of the British congenital cataract study. Invest Ophthalmol Vis Sci. 2006;47:4262–9. https://doi.org/10.1167/iovs.05-1160.
Borisovsky G, Silberberg G, Wygnanski-Jaffe T, Spierer A. Results of congenital cataract surgery with and without intraocular lens implantation in infants and children. Graefes Arch Clin Exp Ophthalmol. 2013;251:2205–11. https://doi.org/10.1007/s00417-013-2327-2.
Lu Y, Ji YH, Luo Y, Jiang YX, Wang M, Chen X. Visual results and complications of primary intraocular lens implantation in infants aged 6 to 12 months. Graefes Arch Clin Exp Ophthalmol. 2010;248:681–6. https://doi.org/10.1007/s00417-010-1310-4.
Louison S, Blanc J, Pallot C, Alassane S, Praudel A, Bron AM, et al. Visual outcomes and complications of congenital cataract surgery. J Fr Ophtalmol. 2019;42:368–74. https://doi.org/10.1016/j.jfo.2018.10.007.
Mittelviefhaus H, Mittelviefhaus K, Gerling J. Ursachen des Kontaktlinsen-Abbruchs bei kindlichen Aphakien. Indikation für Intraokularlinsen? [Etiology of contact lens failure in pediatric aphakia. Indications for intraocular lenses?]. Ophthalmologe. 1998;95:207–12. https://doi.org/10.1007/s003470050263.
Schornack M. “Adverse events associated with scleral lens wear”. J Contact lens Res Sci. 2018;2.SP 1:e13–e17.
Zimmerman AB, Marks A. Microbial keratitis secondary to unintended poor compliance with scleral gas-permeable contact lenses. Eye Contact Lens. 2014;40:e1–e4. https://doi.org/10.1097/ICL.0b013e318273420f.
Fernandes M, Sharma S. Polymicrobial and microsporidial keratitis in a patient using Boston scleral contact lens for Sjogren’s syndrome and ocular cicatricial pemphigoid. Cont Lens Anterior Eye. 2013;36:95–97. https://doi.org/10.1016/j.clae.2012.10.082.
Bruce AS, Nguyen LM. Acute red eye (non-ulcerative keratitis) associated with mini-scleral contact lens wear for keratoconus. Clin Exp Optom. 2013;96:245–8. https://doi.org/10.1111/cxo.12033.
Severinsky B, Behrman S, Frucht-Pery J, Solomon A. Scleral contact lenses for visual rehabilitation after penetrating keratoplasty: long term outcomes. Cont Lens Anterior Eye. 2014;37:196–202. https://doi.org/10.1016/j.clae.2013.11.001.
Vishwanath M, Cheong-Leen R, Taylor D, Russell-Eggitt I, Rahi J. Is early surgery for congenital cataract a risk factor for glaucoma?. Br J Ophthalmol. 2004;88:905–10. https://doi.org/10.1136/bjo.2003.040378.
Magnusson G, Abrahamsson M, Sjöstrand J. Glaucoma following congenital cataract surgery: an 18-year longitudinal follow-up. Acta Ophthalmol Scand. 2000;78:65–70. https://doi.org/10.1034/j.1600-0420.2000.078001065.x.
Solebo AL, Cumberland P, Rahi JS.British Isles Congenital Cataract Interest Group. 5-year outcomes after primary intraocular lens implantation in children aged 2 years or younger with congenital or infantile cataract: findings from the IoLunder2 prospective inception cohort study. Lancet Child Adolesc Health. 2018;2:863–71. https://doi.org/10.1016/S2352-4642(18)30317-1.
Acknowledgements
The abstract of the article has not been presented previously. None of the authors have any proprietary interest in this study. No funds or grants were received for this study. The authors have declared that no competing interests exist. None of the authors has a potential source of conflict of interest - financial or otherwise that might be perceived as influencing an author’s objectivity. VY was responsible for designing the review protocol, writing the protocol and report, conducting the search, screening potentially eligible studies, extracting and analysing data, interpreting results, updating reference lists. IH was responsible for designing the review protocol, the orthoptist who fitted and prescribed the scleral contact lenses, was interpreting results and contributed to writing the report. EM contributed to the design of the review protocol, helped in writing the report, EIA was the surgeon of most of the paediatric patients and provided feedback on the report, IC was extracting and analysing data and interpreting results. NED contributed to designing the review protocol, was the main paediatric ophthalmologist doing a follow up on the patients and provided feedback on the report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yehezkeli, V., Hare, I., Moisseiev, E. et al. Assessment of long-term visual outcomes in aphakic children wearing scleral contact lenses. Eye 37, 421–426 (2023). https://doi.org/10.1038/s41433-022-01942-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-022-01942-6