Abstract
Background
X-linked retinitis pigmentosa (XLRP) is the most severe form of retinitis pigmentosa (RP) and accounts for 15–20% of all RP cases. In this study, we investigated the progression of visual acuity loss across age groups in female carriers and compared it to affected males.
Methods
A PubMed literature search was conducted, and RP2 cases were included based on specific inclusion criteria. Visual acuity (VA), refractive error spherical equivalent (SE), and retinal findings were recorded. Cross-sectional analyses investigated the relationship between VA and age in carrier females and affected males. Genotype-phenotype VA correlations were studied using t-tests.
Results
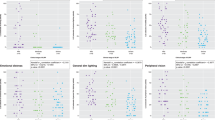
35 carrier females and 28 affected males with confirmed RP2 mutations were collected from 13 studies. The mean age and logMAR VA of carrier females were 44.2 ± 17.4 years, and 0.5 ± 0.5, respectively. 78.8% of carrier females showed abnormal XLRP-related fundus findings and had significantly reduced VA compared to those with normal fundi (0.6 ± 0.5 vs. 0.1 ± 0.1; p = 0.03). Compared to affected males, no statistical correlation was found between logMAR VA and advancing age in carrier females (p = 0.75). Statistically significant linear correlations were found between logMAR VA and SE in each of carrier females (p = 0.01). There were no observed differences in logMAR VA based on mutation type (p = 0.97) or mutation location (p = 0.83). Anisometropia was observed in 38% of carrier females and 68% of affected males; these prevalence numbers are statistically significant between the two groups (1.7 ± 0.3 vs. 3.9 ± 10.9 dioptres; p = 0.03).
Conclusions
RP2 carrier females generally maintain good VA throughout their lifetime, as opposed to affected males, whose vision progressively declines. Our study provides important VA prognostic data that is crucial for patient counseling.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Daiger SP, Bowne SJ, Sullivan LS. Perspective on genes and mutations causing retinitis pigmentosa. Arch Ophthalmol. 2007;125:151–8.
RetNet: Disease Table. Accessed 3 March 2021. https://sph.uth.edu/retnet/disease.htm#23.115d
Fishman GA. Retinitis pigmentosa. Genetic percentages. Arch Ophthalmol. 1978;96:822–6.
Boughman JA, Conneally PM, Nance WE. Population genetic studies of retinitis pigmentosa. Am J Hum Genet. 1980;32:223–35.
Pelletier V, Jambou M, Delphin N, Zinovieva E, Stum M, Gigarel N, et al. Comprehensive survey of mutations in RP2 and RPGR in patients affected with distinct retinal dystrophies: genotype-phenotype correlations and impact on genetic counseling. Hum Mutat. 2007;28:81–91.
Hardcastle AJ, Thiselton DL, Van Maldergem L, Saha BK, Jay M, Plant C, et al. Mutations in the RP2 gene cause disease in 10% of families with familial X-linked retinitis pigmentosa assessed in this study. Am J Hum Genet. 1994;64:1210–5.
Vorster AA, Rebello MT, Coutts N, Ehrenreich L, Gama AD, Roberts LJ, et al. Arg120stop nonsense mutation in the RP2 gene: mutational hotspot and germ line mosaicism? Clin Genet. 2004;65:7–10.
De Silva SR, Arno G, Robson AG, Fakin A, Pontikos N, Mohamed MD, et al. The X-linked retinopathies: physiological insights, pathogenic mechanisms, phenotypic features and novel therapies. Prog Retin Eye Res. 2021;82:100898.
Sharon D, Sandberg MA, Rabe VW, Stillberger M, Dryja TP, Berson EL. RP2 and RPGR mutations and clinical correlations in patients with X-linked retinitis pigmentosa. Am J Hum Genet. 2003;73:1131–46.
Jayasundera T, Branham KE, Othman M, Rhoades WR, Karoukis AJ, Khanna H, et al. The RP2 phenotype and pathogenetic correlations in X-linked retinitis pigmentosa. Arch Ophthalmol. 2010;128:915–23.
Rosenberg T, Schwahn U, Feil S, Berger W. Genotype-phenotype correlation in X-linked retinitis pigmentosa 2 (RP2). Ophthalmic Genet. 1999;20:161–72.
Comander J, Weigel-DiFranco C, Sandberg MA, Berson EL. Visual function in carriers of X-linked retinitis pigmentosa. Ophthalmology 2015;122:1899–906.
Grover S, Fishman GA, Anderson RJ, Lindeman M. A longitudinal study of visual function in carriers of X-linked recessive retinitis pigmentosa. Ophthalmology 2000;107:386–96.
Roberts MF, Fishman GA, Roberts DK, Heckenlively JR, Weleber RG, Anderson RJ, et al. Retrospective, longitudinal, and cross sectional study of visual acuity impairment in choroideraemia. Br J Ophthalmol. 2002;86:658–62.
World Health Organization. Consultation on development of standards for characterization of vision loss and visual functioning: Geneva, 4-5 September 2003. Published online 2003. Accessed 13 March 2021. https://apps.who.int/iris/handle/10665/68601
Friedrich U, Warburg M, Kruse TA, Andréasson S. X-linked retinitis pigmentosa: new map studies of XLRP2, and a possible human centromere effect. Hum Genet. 1992;88:683–7.
Fishman GA, Weinberg AB, McMahon TT. X-linked recessive retinitis pigmentosa. Clinical characteristics of carriers. Arch Ophthalmol. 1986;104:1329–35.
Lyon MF. Gene action in the X-chromosome of the mouse (Mus musculus L.). Nature. 1961;190:372–3.
Wu H, Luo J, Yu H, Rattner A, Mo A, Wang Y, et al. Cellular resolution maps of X chromosome inactivation: implications for neural development, function, and disease. Neuron 2014;81:103–19.
Bax NM, Valkenburg D, Lambertus S, Klevering BJ, Boon CJF, Holz FG, et al. Foveal sparing in central retinal dystrophies. Invest Ophthalmol Vis Sci. 2019;60:3456–67.
Neidhardt J, Glaus E, Lorenz B, Netzer C, Li Y, Schambeck M, et al. Identification of novel mutations in X-linked retinitis pigmentosa families and implications for diagnostic testing. Mol Vis. 2008;14:1081–93.
Jin Z-B, Liu X-Q, Hayakawa M, Murakami A, Nao-i N. Mutational analysis of RPGR and RP2 genes in Japanese patients with retinitis pigmentosa: identification of four mutations. Mol Vis. 2006;12:1167–74.
Prokisch H, Hartig M, Hellinger R, Meitinger T, Rosenberg T. A population-based epidemiological and genetic study of X-linked retinitis pigmentosa. Invest Ophthalmol Vis Sci. 2007;48:4012–8.
Kurata K, Hosono K, Hayashi T, Mizobuchi K, Katagiri S, Miyamichi D, et al. X-linked retinitis pigmentosa in Japan: clinical and genetic findings in male patients and female carriers. Int J Mol Sci. 2019;20:1518.
Ji Y, Wang J, Xiao X, Li S, Guo X, Zhang Q. Mutations in RPGR and RP2 of Chinese patients with X-linked retinitis pigmentosa. Curr Eye Res. 2010;35:73–79.
Flaxel C, Jay M, Thiselton D, Nayudu M, Hardcastle A, Wright A, et al. Difference between RP2 and RP3 phenotypes in X linked retinitis pigmentosa. Br J Ophthalmol. 1999;83:1144–8.
Kühnel K, Veltel S, Schlichting I, Wittinghofer A. Crystal structure of the human retinitis pigmentosa 2 protein and its interaction with Arl3. Structure 2006;14:367–78.
Li H-P, Yuan S-Q, Wang X-G, Sheng X-L, Li X-R. Myopia with X-linked retinitis pigmentosa results from a novel gross deletion of RPGR gene. Int J Ophthalmol. 2020;13:1306–11.
Miano MG, Testa F, Filippini F, Trujillo M, Conte I, Lanzara C, et al. Identification of novel RP2 mutations in a subset of X-linked retinitis pigmentosa families and prediction of new domains. Hum Mutat. 2001;18:109–19.
Acknowledgements
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
OBS, and RGC, participated in study design, data collection, data analysis, manuscript writing, as well as manuscript review and editing. EIT participated in study design, data analysis, manuscript writing, as well as manuscript review editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Saeed, O.B., Traboulsi, E.I. & Coussa, R.G. Profiling of visual acuity and genotype correlations in RP2 patients: a cross-sectional comparative meta-analysis between carrier females and affected males. Eye 37, 350–355 (2023). https://doi.org/10.1038/s41433-022-01954-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-022-01954-2