Abstract
Objectives
To analyse the longitudinal changes in visual acuity and risk factors for recurrence or development of choroidal neovascularisation (CNV) in eyes with acute or chronic central serous chorioretinopathy (CSCR).
Methods
This was a retrospective, multicentric, longitudinal, observational study done in patients with a diagnosis of unilateral or bilateral CSCR and having at least 4 years of follow-up between the years 1999 and 2020. Kaplan–Meier curves were used for assessing cumulative risks. Multivariate logistic, linear and cox regression models were used for risk factor analyses. The trend in visual acuity, cumulative risks of recurrence and CNV formation was analysed.
Results
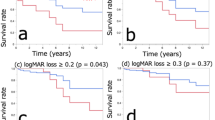
A total of 117 out of 175 eyes (66.8%) had stable or improvement in vision at last follow-up, while 24 eyes had more than/equal to 3 line loss of vision. Four eyes (7.7%) with acute CSCR at initial presentation developed features of chronic CSCR at the final presentation. Thirty-seven eyes had recurrence during the follow-up with a 10-year cumulative recurrence rate of around 30%. On Cox proportional hazard regression analysis, history of previous treatment and male gender (p = 0.03) were associated with a lower risk of recurrence. Twenty-four developed de novo CNV by the end of follow-up and higher age (p = 0.001) and a higher number of recurrences (p = 0.05) were associated with a higher risk of early de novo CNV formation. The cumulative 10-year CNV development rate was 17.4%.
Conclusion
A non-temporal relationship between acute and chronic CSCR was seen. Previous treatment, smoking and baseline RPE abnormality affected recurrence of SRF or CNV formation.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated during and/or analysed during the study are available from the corresponding author on reasonable request.
References
Von Graefe A. Ueber centrale recidivierende retinitis. Graefes Arch Clin Exp Ophthalmol. 1866;12:211–5.
Mrejen S, Spaide RF. Optical coherence tomography: imaging of the choroid and beyond. Surv Ophthalmol. 2013;58:387–429.
Yang L, Jonas JB, Wei W. Optical coherence tomography–assisted enhanced depth imaging of central serous chorioretinopathy. Inv Ophthalmol Vis Sci. 2013;54:4659–65.
Jirarattanasopa P, Ooto S, Tsujikawa A, Yamashiro K, Hangai M, Hirata M, et al. Assessment of macular choroidal thickness by optical coherence tomography and angiographic changes in central serous chorioretinopathy. Ophthalmology. 2012;119:1666–78.
Wang M, Munch IC, Hasler PW, Prünte C, Larsen M. Central serous chorioretinopathy. Act Ophthalmol. 2008;86:126–45.
Ross A, Ross AH, Mohamed Q. Review and update of central serous chorioretinopathy. Curr Opin Ophthalmol. 2011;22:166–73.
Klein ML, Van Buskirk EM, Friedman E, Gragoudas E, Chandra S. Experience with nontreatment of central serous choroidopathy. Arch Ophthalmol. 1974;91:247–50.
Gilbert CM, Owens SL, Smith PD, Fine SL. Long-term follow-up of central serous chorioretinopathy. Br J Ophthalmol. 1984;68:815–20.
Sartini F, Figus M, Nardi M, Casini G, Posarelli C. Non-resolving, recurrent and chronic central serous chorioretinopathy: available treatment options. Eye. 2019;33:1035–43.
Kanyange M, De Laey J. Long-term follow-up of central serous chorioretinopathy (CSCR). Bull Soc Belg Ophtalmol. 2002;284:39–44.
Ferrara D, Mohler KJ, Waheed N, Adhi M, Liu JJ, Grulkowski I, et al. En face enhanced-depth swept-source optical coherence tomography features of chronic central serous chorioretinopathy. Ophthalmology. 2014;121:719–26.
Zola M, Chatziralli I, Menon D, Schwartz R, Hykin P, Sivaprasad S. Evolution of fundus autofluorescence patterns over time in patients with chronic central serous chorioretinopathy. Act Ophthalmol. 2018;96:e835–e9.
Daruich A, Matet A, Dirani A, Bousquet E, Zhao M, Farman N, et al. Central serous chorioretinopathy: recent findings and new physiopathology hypothesis. Prog Retin Eye Res. 2015;48:82–118.
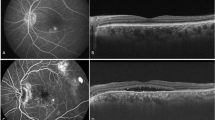
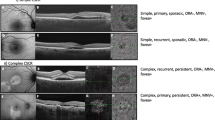
Chhablani J, Cohen FB, Aymard P, Beydoun T, Bousquet E, Daruich-Matet A, et al. Multimodal imaging-based central serous chorioretinopathy classification. Ophthalmol Retin. 2020;4:1043–6.
Mrejen S, Balaratnasingam C, Kaden TR, Bottini A, Dansingani K, Bhavsar KV, et al. Long-term visual outcomes and causes of vision loss in chronic central serous chorioretinopathy. Ophthalmology. 2019;126:576–88.
Haimovici R, Koh S, Gagnon DR, Lehrfeld T, Wellik S, Central Serous Chorioretinopathy Case-Control Study Group. Risk factors for central serous chorioretinopathy: a case–control study. Ophthalmology. 2004;111:244–9.
Yu J, Xu G, Chang Q, Ye X, Li L, Jiang C, et al. Risk factors for persistent or recurrent central serous chorioretinopathy. J Ophthalmol. 2019;2019:5970659.
Lai TYY, Wong RLM, Chan W-M. Long-term outcome of half-dose verteporfin photodynamic therapy for the treatment of central serous chorioretinopathy (an American Ophthalmological Society Thesis). Trans Am Ophthalmol Soc. 2015;113:T8.
Doyle J, Gupta B, Tahir I. Long term outcomes for patients treated with half-fluence photodynamic therapy for chronic central serous chorioretinopathy: a case series. Int J Ophthalmol. 2018;11:333.
Lai FH, Ng DS, Bakthavatsalam M, Chan VC, Young AL, Luk FO, et al. A multicenter study on the long-term outcomes of half-dose photodynamic therapy in chronic central serous chorioretinopathy. Am J Ophthalmol. 2016;170:91–9.
Chan W, Lam D, Lai T, Tam B, Liu D, Chan C. Choroidal vascular remodelling in central serous chorioretinopathy after indocyanine green guided photodynamic therapy with verteporfin: a novel treatment at the primary disease level. Br J Ophthalmol. 2003;87:1453–8.
Türkcü FM, Yüksel H, Şahin A, Cinar Y, Cingü K, Arı Ş, et al. Effects of smoking on visual acuity of central serous chorioretinopathy patients. Cutan Ocul Toxicol. 2014;33:115–9.
Gerzanich V, Zhang F, West GA, Simard JM. Chronic nicotine alters NO signaling of Ca2+ channels in cerebral arterioles. Circ Res. 2001;88:359–65.
Yannuzzi LA. Central serous chorioretinopathy: a personal perspective. Am J Ophthalmol. 2010;149:361–3. e1
Stattin M, Ahmed D, Forster J, Glittenberg C, Herrmann M, Krebs I, et al. Detection of secondary choroidal neovascularization in chronic central serous chorioretinopathy by swept source‐optical coherence tomography angiography. Act Ophthalmol. 2019;97:e135–e6.
Sahoo NK, Mishra SB, Iovino C, Singh SR, Munk MR, Berger L, et al. Optical coherence tomography angiography findings in cystoid macular degeneration associated with central serous chorioretinopathy. Br J Ophthalmol. 2019;103:1615–8.
Spaide RF, Campeas L, Haas A, Yannuzzi LA, Fisher YL, Guyer DR, et al. Central serous chorioretinopathy in younger and older adults. Ophthalmology. 1996;103:2070–80.
Ergun E, Tittl M, Stur M. Photodynamic therapy with verteporfin in subfoveal choroidal neovascularizationsecondary to central serous chorioretinopathy. Arch Ophthalmol. 2004;122:37–41.
Chhablani J, Kozak I, Pichi F, Chenworth M, Berrocal MH, Bedi R, et al. Outcomes of treatment of choroidal neovascularization associated with central serous chorioretinopathy with intravitreal antiangiogenic agents. Retina. 2015;35:2489–97.
Sacconi R, Tomasso L, Corbelli E, Carnevali A, Querques L, Casati S, et al. Early response to the treatment of choroidal neovascularization complicating central serous chorioretinopathy: a OCT-angiography study. Eye. 2019;33:1809–17.
Piccolino FC, De La Longrais RR, Manea M, Cicinelli S, Ravera G. Risk factors for posterior cystoid retinal degeneration in central serous chorioretinopathy. Retina. 2008;28:1146–50.
Iida T, Yannuzzi LA, Spaide RF, Borodoker N, Carvalho CA, Negrao S. Cystoid macular degeneration in chronic central serous chorioretinopathy. Retina. 2003;23:1–7.
Sheth J, Anantharaman G, Chandra S, Sivaprasad S. “Double-layer sign” on spectral domain optical coherence tomography in pachychoroid spectrum disease. Ind J Ophthalmol. 2018;66:1796.
Hagag AM, Rasheed R, Sivaprasad S. The significance of double layer sign in eyes with choroidal neovascularization secondary to central serous chorioretinopathy. Inv Ophthalmol Vis Sci. 2021;62:1922.
Chhablani J, Mandadi SK. Commentary: “double-layer sign” on spectral domain optical coherence tomography in pachychoroid spectrum disease. Ind J Ophthalmol. 2019;67:171.
Author information
Authors and Affiliations
Contributions
JC: design; NKS, JO, AS, DM, NGR, SM: conduct of the study; JO, AS, DM, NGR, SM: collection; RS, RV, BT, LHL, VP, GA, AMC, GL-G, NW, EB, GQ: management; NKS, JO, AS, DM, NGR: analysis; NKS, JO: interpretation of the data; NKS, JO: preparation; RS, RV, BT, LHL, VP, GA, AMC, GL-G, NW, EB, GQ, JC: review; RS, RV, BT, LHL, VP, GA, AMC, GL-G, NW, EB, GQ, JC: approval of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sahoo, N.K., Ong, J., Selvam, A. et al. Longitudinal follow-up and outcome analysis in central serous chorioretinopathy. Eye 37, 732–738 (2023). https://doi.org/10.1038/s41433-022-02044-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-022-02044-z
This article is cited by
-
Photobiomodulation Therapy with Low-Level Light in Chronic Central Serous Chorioretinopathy: A Pilot Study
Ophthalmology and Therapy (2026)
-
Importance of OCT-derived biomarkers for the recurrence of central serous chorioretinopathy using statistics and predictive modelling
Scientific Reports (2024)
-
Pathomechanisms in central serous chorioretinopathy: A recent update
International Journal of Retina and Vitreous (2023)
-
Ten-year follow-up and sequential evaluation of multifocal retinal pigment epithelium abnormalities in central serous chorioretinopathy
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)