Abstract
Background/Objectives
The aim of this study was to ascertain the use of ocular imaging and the updated screening criteria in the evaluation of choroidal nevus across the United States.
Methods
Sixty ophthalmologists completed an anonymous 21-question survey addressing their use of the screening criteria for evaluating choroidal nevi, as well as their use of ultrasonography (US), optical coherence tomography (OCT), and autofluorescence (AF) in daily practice.
Results
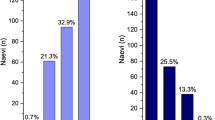
The majority of respondents were from the Northeast (55%), worked in private practice (83%), and practiced general ophthalmology (42%). The 2009 criteria TFSOM-UHHD was used by 39 (65%) respondents, while the 2019 criteria TFSOM-DIM was used by 29 (48%) respondents. Compared to anterior segment ophthalmologists, posterior segment ophthalmologists were more likely to use the TFSOM-UHHD criteria (94% vs. 53%, OR = 13.9, p = 0.014), the TFSOM-DIM criteria (88% vs. 33%, OR = 15.5, p < 0.001), fundus AF (82% vs. 19%, OR = 20.4, p < 0.001), and US (94% vs. 42%, OR = 22.2, p = 0.004) in daily practice.
Conclusions
From the survey of current practice patterns, we learned that there is a general trend of underutilization of the proper imaging modalities – and thus the criteria – in evaluating choroidal nevus. More education about ocular cancer and its screening could improve patient outcomes in the future.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request (email: JosephDDeSimone@gmail.com).
References
Shields JA, Shields CL. Intraocular tumors. An atlas and textbook. 3rd ed. Philadelphia, PA: Lippincott Wolters Kluwers; 2016. p. 69–80.
Sumich P, Mitchell P, Wang JJ. Choroidal nevi in a white population: the Blue Mountains Eye Study. Arch Ophthalmol. 1998;116:645–50.
Qiu M, Shields CL. Choroidal nevus in the United States adult population: racial disparities and associated factors in the national health and nutrition examination survey. Ophthalmology. 2015;122:2071–83.
Shields CL, Furuta M, Mashayekhi A, Berman EL, Zahler JD, Hoberman DM, et al. Clinical spectrum of choroidal nevi based on age at presentation in 3422 consecutive eyes. Ophthalmology. 2008;115:546–52.
Singh AD, Kalyani P, Topham A. Estimating the risk of malignant transformation of choroidal nevus. Ophthalmology. 2005;112:1784–9.
Shields CL, Furuta M, Berman EL, Zahler JD, Hoberman DM, Dinh DH, et al. Choroidal nevus transformation into melanoma: analysis of 2514 consecutive cases. Arch Ophthalmol. 2009;127:981–7.
Shields CL, Shields JA, Kiratli H, De Potter P, Cater JR. Risk factors for growth and metastasis of small choroidal melanocytic lesions. Ophthalmology. 1995;102:1351–61.
Shields CL, Dalvin LA, Ancona-Lezama D, Yu MD, Di Nicola M, Williams BK Jr., et al. Choroidal nevus imaging features in 3,806 cases and risk factors for transformation into melanoma in 2,355 cases: The 2020 Taylor R. Smith and Victor T. Curtin Lecture. Retina. 2019;39:1840–51.
Damato EM, Damato BE. Detection and time to treatment of uveal melanoma in the United Kingdom: an evaluation of 2,384 patients. Ophthalmology. 2012;119:1582–9.
Mehrotra A, Forrest CB, Lin CY. Dropping the baton: specialty referrals in the United States. Milbank Q. 2011;89:39–68.
Law C, Krema H, Simpson ER. Referral patterns of intraocular tumour patients to a dedicated Canadian ocular oncology department. Can J Ophthalmol. 2012;47:254–61.
Eiger-Moscovich M, Eagle RC Jr, Shields CL, Racher H, Lally SE, Silkiss RZ, et al. Muir-Torre Syndrome associated periocular sebaceous neoplasms: screening patterns in the literature and in clinical practice. Ocul Oncol Pathol. 2020;6:226–37.
Shah SN, Kogachi K, Correa ZM, Schefler AC, Aronow ME, Callejo SA, et al. Trends in radiation practices for female ocular oncologists in North America: a collaborative study of the international society of ocular oncology. Ocul Oncol Pathol. 2019;5:54–59.
Funding
Support provided in part by the Eye Tumor Research Foundation, Philadelphia, PA (CLS). The funders had no role in the design and conduct of the study, in the collection, analysis and interpretation of the data, and in the preparation, review or approval of the manuscript.
Author information
Authors and Affiliations
Contributions
CLS had full access to the data and takes responsibility for the integrity of the data and data analysis. Concept and design: JDD, CLS. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: JDD. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: JDD, PWD. Obtained funding: CLS. Supervision: CLS, RRS.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The Wills Eye Hospital Institutional Review Board deemed that this study was exempted from IRB approval. This study adhered to the tenets of the declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
DeSimone, J.D., Dockery, P.W., Kreinces, J.B. et al. Survey of ophthalmic imaging use to assess risk of progression of choroidal nevus to melanoma. Eye 37, 953–958 (2023). https://doi.org/10.1038/s41433-022-02110-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-022-02110-6
This article is cited by
-
Peroxisome proliferator-activated receptor gamma coactivator-1 (PGC-1) family in physiological and pathophysiological process and diseases
Signal Transduction and Targeted Therapy (2024)
-
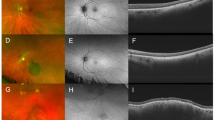
Multimodal imaging risk factors predictive of small choroidal melanocytic lesion growth to melanoma: An educational study and pictorial guide
Eye (2024)
-
Ocular oncology demystified
Eye (2023)