Abstract
Purpose
To evaluate the clinical efficacy and safety of asynchronous virtual post-operative assessments following vitreoretinal surgery and procedures compared to traditional face-to-face assessments in a high-volume tertiary eye centre.
Methods
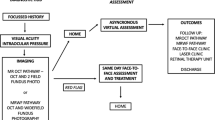
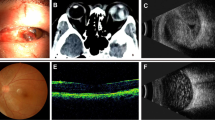
Prospective comparative clinical series study of patients who had undergone vitreoretinal surgery or post-laser retinopexy. Patients received both virtual and face-to-face assessments. The virtual assessment included clinical questions, visual acuity measurement, and virtual retinal imaging using ultra-wide field (UWF) imaging and macular optical coherence tomography (OCT). Face-to-face assessments involved standard clinical examinations.
Results
We included 142 patients undergoing a variety of vitreoretinal procedures. We showed comparable results between virtual and face-to-face assessments in both, post-operative and post-laser treatments. UWF imaging with macular OCT demonstrated potential for effective virtual post-operative assessment. The virtual assessment has a sensitivity of 91% and specificity of 100% for detecting retinal detachments with 100% specificity and 100% sensitivity for detecting new retinal tears or insufficient laser treatment.
Conclusions
The implementation of asynchronous virtual post-operative assessments following a variety of vitreoretinal procedures is a promising alternative to traditional face-to-face assessments. Virtual assessments using UWF imaging and macular OCT showed high sensitivity and specificity. Virtual post-operative clinics offer the potential to improve patient access and decrease the clinical burden, especially with the continuing evolution of telemedicine technologies and imaging modalities.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
References
Hanumunthadu D, Adan K, Tinkler K, Balaskas K, Hamilton R, Nicholson L. Moorfields Medical Retina Virtual Assessment Study Group. Outcomes following implementation of a high-volume medical retina virtual clinic utilising a diagnostic hub during COVID-19. Eye. 2022;36:627–33. https://doi.org/10.1038/s41433-021-01510-4.
Jayaram H, Strouthidis NG, Gazzard G. The COVID-19 pandemic will redefine the future delivery of glaucoma care. Eye. 2020;34:1203–5. https://doi.org/10.1038/s41433-020-0958-1.
Kilduff CL, Thomas AA, Dugdill J, Casswell EJ, Dabrowski M, Lovegrove C, et al. Creating the Moorfields’ virtual eye casualty: video consultations to provide emergency teleophthalmology care during and beyond the COVID-19 pandemic. BMJ Health Care Inf. 2020;27:e100179. https://doi.org/10.1136/bmjhci-2020-100179.
Al Harby L, Ali Z, Rajai A, Roberts SA, Peto T, Leung I, et al. Prospective validation of a virtual clinic pathway in the management of choroidal naevi: the NAEVUS study report no. 1: safety assessment. Br J Ophthalmol. 2022;106:128–34. https://doi.org/10.1136/bjophthalmol-2020-317371.
Kern C, Kortuem K, Hamilton R, Fasolo S, Cai Y, Balaskas K, et al. Clinical outcomes of a hospital-based teleophthalmology service: what happens to patients in a virtual clinic? Ophthalmol Retin. 2019;3:422–8. https://doi.org/10.1016/j.oret.2019.01.011.
Kumar V, Surve A, Kumawat D, Takkar B, Azad S, Chawla R, et al. Ultra-wide field retinal imaging: a wider clinical perspective. Indian J Ophthalmol. 2021;69:824–35. https://doi.org/10.4103/ijo.IJO_1403_20.
Fogliato G, Borrelli E, Iuliano L, Ramoni A, Querques L, Rabiolo A, et al. Comparison between ultra-widefield pseudocolor imaging and indirect ophthalmoscopy in the detection of peripheral retinal lesions. Ophthalmic Surg Lasers Imaging Retin. 2019;50:544–9. https://doi.org/10.3928/23258160-20190905-02.
Kornberg DL, Klufas MA, Yannuzzi NA, Orlin A, D’Amico DJ, Kiss S. Clinical utility of ultra-widefield imaging with the Optos Optomap compared with indirect ophthalmoscopy in the setting of non-traumatic rhegmatogenous retinal detachment. Semin Ophthalmol. 2016;31:505–12. https://doi.org/10.3109/08820538.2014.981551.
Inoue M, Koto T, Hirota K, Hirakata A. Ultra-widefield fundus imaging in gas-filled eyes after vitrectomy. BMC Ophthalmol. 2017;17:114 https://doi.org/10.1186/s12886-017-0510-7.
Chen QY, Tang YX, He YQ, Lin HM, Gao RL, Li MY, et al. Air tamponade in retinal detachment surgery followed by ultra-widefield fundus imaging system. Int J Ophthalmol. 2018;11:1198–203. https://doi.org/10.18240/ijo.2018.07.20.
Witmer MT, Cho M, Favarone G, Chan RV, D’Amico DJ, Kiss S. Ultra-wide-field autofluorescence imaging in non-traumatic rhegmatogenous retinal detachment. Eye. 2012;26:1209–16. https://doi.org/10.1038/eye.2012.122.
Lin AC, Kalaw FGP, Schönbach EM, Song D, Koretz Z, Walker E, et al. The sensitivity of ultra-widefield fundus photography versus scleral depressed examination for detection of retinal horseshoe tears. Am J Ophthalmol. 2023;255:155–60. https://doi.org/10.1016/j.ajo.2023.07.010.
NHS. Chapter 5: Digitally-Enabled Care Will Go Mainstream Across The NHS. Online version of the NHS Long Term Plan. 2020. https://www.longtermplan.nhs.uk/online-version/chapter-5-digitally-enabled-care-will-go-mainstream-across-the-nhs/.
Kovai V, Rao GN, Holden B. Key factors determining success of primary eye care through vision centres in rural India: patients’ perspectives. Indian J Ophthalmol. 2012;60:487–91. https://doi.org/10.4103/0301-4738.100558.
Shahid SM, Anguita R, daCruz L. Telemedicine for postoperative consultations following vitrectomy for retinal detachment repair during the COVID-19 crisis: a patient satisfaction survey. Can J Ophthalmol. 2021;56:e46–e48. https://doi.org/10.1016/j.jcjo.2020.11.011.
Anguita R, Makuloluwa A, Hind J, Wickham L. Large language models in vitreoretinal surgery. Eye. 2024;38:809–10. https://doi.org/10.1038/s41433-023-02751-1.
Ferro Desideri L, Roth J, Zinkernagel M, Anguita R. Application and accuracy of artificial intelligence-derived large language models in patients with age related macular degeneration. Int J Retin Vitr. 2023;9:71. https://doi.org/10.1186/s40942-023-00511-7.
Author information
Authors and Affiliations
Contributions
RA and LW conceived and designed the research. SA, AM and JH collected the data. RA and JR analysed the data. RA, JR and LW analysed and interpreted the literature. RA, SA, AM, JH, JR and LW draughted the manuscript and made critical revisions of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Anguita, R., Ahmed, S., Makuloluwa, A. et al. Prospective validation of a virtual post-operative clinic in vitreoretinal surgery. Eye 38, 3258–3262 (2024). https://doi.org/10.1038/s41433-024-03272-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-024-03272-1
This article is cited by
-
Virtual vitreoretinal clinics: a service delivery pathway of the future
International Journal of Retina and Vitreous (2025)
-
Sensitivity and utility of ultra-wide field imaging for the detection of peripheral retinal breaks in a large Irish tertiary referral centre
Eye (2025)