Abstract
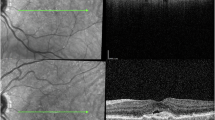
In this narrative review we describe the main optical coherence tomography biomarkers appearing in eyes with neovascular age-related macular degeneration (AMD) that do not directly correspond to exudation. We highlight those signs that may mimic exudation and therefore do not require active treatment, such as outer retinal tubulations, pseudocysts, lipid globules, or hyporeflective wedges. Other signs may indicate impending exudation such as hyperreflective foci or shallow irregular retinal pigment epithelium elevation, and therefore should be carefully monitored. We also review and summarize the different origins of subretinal hyperreflective material and describe the main signs of degeneration seen in eyes with AMD, such as outer retinal tubulation, thinning of the retinal layers, outer retinal atrophy, and choroidal changes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Keenan T, Cukras C, Chew E. Age-related macular degeneration: epidemiology and clinical aspects. Adv Exp Med Biol. 2021;1256:1–31.
Ferris FL, Wilkinson CP, Bird A, Chakravarthy U, Chew E, Csaky K, et al. Clinical classification of age-related macular degeneration. Ophthalmology. 2013;120:844–51.
Vidal-Oliver L, Montolío-Marzo E, Gallego-Pinazo R, Dolz-Marco R. Optical coherence tomography biomarkers in early and intermediate age-related macular degeneration: a clinical guide. Clin Exp Ophthalmol. 2024;52:207–19.
Borrelli E, Barresi C, Lari G, Berni A, Battista M, Reibaldi M et al. Capturing the transition from intermediate to neovascular AMD: longitudinal inner retinal thinning and factors associated with neuronal loss. Invest Ophthalmol Vis Sci. 2023;64:21.
Rudas A, Chiang JN, Corradetti G, Rakocz N, Avram O, Halperin E, et al. Automated large-scale prediction of exudative AMD progression using machine-read OCT biomarkers. PLoS Digit Heal. 2023;2:e0000106. https://doi.org/10.1371/journal.pdig.0000106.
Wakatsuki Y, Hirabayashi K, Yu HJ, Marion KM, Corradetti G, Wykoff CC, et al. Optical coherence tomography biomarkers for conversion to exudative neovascular age-related macular degeneration. Am J Ophthalmol. 2023;247:137–44.
Xu L, Mrejen S, Jung JJ, Gallego-Pinazo R, Thompson D, Marsiglia M, et al. Geographic atrophy in patients receiving anti-vascular endothelial growth factor for neovascular age-related macular degeneration. Retina. 2015;35:176–86.
Mrejen S, Jung JJ, Chen C, Patel SN, Gallego-Pinazo R, Yannuzzi N, et al. Long-term visual outcomes for a treat and extend anti-vascular endothelial growth factor regimen in eyes with neovascular age-related macular degeneration. J Clin Med. 2015;4:1380–402.
Kar SS, Cetin H, Lunasco L, Le TK, Zahid R, Meng X, et al. OCT-derived radiomic features predict anti–VEGF response and durability in neovascular age-related macular degeneration. Ophthalmol Sci. 2022;2:100171. https://doi.org/10.1016/j.xops.2022.100171.
Pugazhendhi A, Hubbell M, Jairam P, Ambati B. Neovascular macular degeneration: a review of etiology, risk factors, and recent advances in research and therapy. Int J Mol Sci. 2021;22:1–25.
Monje-Fernández L, Gallego-Pinazo R, Cordero-Coma M, Donate-López J, Coco-Martín RM, Dolz-Marco R. Evaluation of non-exudative tomographic signs in cases of exudative age-related macular degeneration. Arch Soc Esp Oftalmol. 2023;98:276–80.
Zatreanu L, Freund K, Leong B, Yu H, Teke M, Yzer S, et al. Serous macular detachment in Best disease: a Masquerade Syndrome. Retina. 2020;40:1456–70.
Sacconi R, Fragiotta S, Sarraf D, Sadda SVR, Freund KB, Parravano M, et al. Towards a better understanding of non-exudative choroidal and macular neovascularization. Prog Retin Eye Res. 2023;92:101113. https://doi.org/10.1016/j.preteyeres.2022.101113.
Hirabayashi K, Yu H, Wakatsuki Y, Marion K, Wykoff CC, Sadda S. OCT risk factors for development of atrophy in eyes with intermediate age-related macular degeneration. Ophthalmol Retin. 2023;7:253–60.
Ricardi F, Borrelli E, Boscia G, Gelormini F, Marica V, Conte F, et al. Relationship of topographic distribution of macular atrophy secondary to neovascular AMD and reading performance. Invest Ophthalmol Vis Sci. 2024;65:44.
Querques G, Coscas F, Forte R, Massamba N, Sterkers M, Souied EH. Cystoid macular degeneration in exudative age-related macular degeneration. Am J Ophthalmol. 2011;152:100–7.
Cohen SY, Dubois L, Nghiem-Buffet S, Ayrault S, Fajnkuchen F, Guiberteau B, et al. Retinal pseudocysts in age-related geographic atrophy. Am J Ophthalmol. 2010;150:211–7.
Servillo A, Kesim C, Sacconi R, Battist M, Capuano V, Fragiotta S, et al. Non-exudative intraretinal fluid in intermediate age-related macular degeneration. Retina. 2024. https://doi.org/10.1097/IAE.0000000000004054.
Berlin A, Messinger JD, Balaratnasingam C, Mendis R, Ferrara D, Freund KB, et al. Imaging histology correlations of intraretinal fluid in neovascular age-related macular degeneration. Transl Vis Sci Technol. 2023;12:1–15.
Fragiotta S, Abdolrahimzadeh S, Dolz-Marco R, Sakurada Y, Gal-Or O, Scuderi G. Significance of hyperreflective foci as an optical coherence tomography biomarker in retinal diseases: characterization and clinical implications. J Ophthalmol. 2021;2021:6096017.
Cao D, Leong B, Messinger JD, Kar D, Ach T, Yannuzzi LA, et al. Hyperreflective foci, optical coherence tomography progression indicators in age-related macular degeneration, include transdifferentiated retinal pigment epithelium. Invest Ophthalmol Vis Sci. 2021;62:34.
Goh KL, Wintergerst MWM, Abbott CJ, Hadoux X, Jannaud M, Kumar H, et al. Hyperreflective foci not seen as hyperpigmentary abnormalities on color fundus photographs in age-related macular degeneration. Retina. 2024;44:214–21.
Duic C, Pfau K, Keenan T, Wiley H, Thavikulwat A, Chew E, et al. Hyperreflective foci in age-related macular degeneration are associated with disease severity and functional impairment. Ophthalmol Retin. 2023;7:307–17.
Balaratnasingam C, Messinger JD, Sloan KR, Yannuzzi LA, Freund KB, Curcio CA. Histologic and optical coherence tomographic correlates in drusenoid pigment epithelium detachment in age-related macular degeneration. Ophthalmology. 2017;124:644–56.
Bousquet E, Santina A, Corradetti G, Sacconi R, Ramtohul P, Bijon J, et al. From drusen to type 3 macular neovascularization. Retina. 2024;44:189–96.
Sacconi R, Sarraf D, Garrity S, Freund K, Yanuzzi L, Gal-Or O, et al. Nascent type 3 neovascularization in age-related macular degeneration. Ophthalmol Retina. 2018;2:1097–106.
Segal O, Barayev E, Nemet AY, Geffen N, Vainer I, Mimouni M. Prognostic value of hyperreflective foci in neovascular age-related macular degeneration treated with Bevacizumab. Retina. 2016;36:2175–82.
Moraes G, Fu DJ, Wilson M, Khalid H, Wagner SK, Korot E, et al. Quantitative analysis of OCT for neovascular age-related macular degeneration using deep learning. Ophthalmology. 2021;128:693–705.
Goldberg NR, Greenberg JP, Laud K, Tsang S, Freund KB. Outer retinal tubulation in degenerative retinal disorders. Retina. 2013;33:1871–6.
Arrigo A, Aragona E, Battaglia O, Saladino A, Amato A, Borghesan F, et al. Outer retinal tubulation formation and clinical course of advanced age-related macular degeneration. Sci Rep. 2021;11:1–12.
Janse Van Rensburg E, Ryu CL, Rampakakis E, Vila N, Chan EW, Chen JC. Outer retinal tubulation may result from fibrosed type 2 neovascularization: clinical observations and model of pathogenesis. Retina. 2021;41:1930–9.
Zweifel S, Engelbert M, Laud K, Margolis R, Spaide R, Freund KB. Outer retinal tubulation: a novel optical coherence tomography finding. Arch Opthalmol. 2009;127:1596–602.
Schaal KB, Freund KB, Litts KM, Zhang Y, Messinger JD, Curcio CA. Outer retinal tubulation in advanced age-related macular degeneration optical coherence tomographic findings correspond to histology. Retina. 2015;35:1339–50.
Litts KM, Ach T, Hammack KM, Sloan KR, Zhang Y, Freund KB, et al. Quantitative analysis of outer retinal tubulation in age-related macular degeneration from spectral-domain optical coherence tomography and histology. Invest Ophthalmol Vis Sci. 2016;57:2647–56.
Wolff B, Matet A, Vasseur V, Sahel JA, Mauget-Faÿsse M. En face OCT imaging for the diagnosis of outer retinal tubulations in age-related macular degeneration. J Ophthalmol. 2012;2012:542417. https://doi.org/10.1155/2012/542417.
Dolz-Marco R, Litts KM, Tan ACS, Freund KB, Curcio CA. The evolution of outer retinal tubulation, a neurodegeneration and gliosis prominent in macular diseases. Ophthalmology. 2017;124:1353–67.
Iaculli C, Barone A, Scudieri M, Palumbo MG, Noci ND. Outer retinal tubulation: characteristics in patients with neovascular age-related macular degeneration. Retina. 2015;35:1979–84.
Kovacs A, Kiss T, Rarosi F, Somfai GM, Facsko A, Degi R. The effect of ranibizumab and aflibercept treatment on the prevalence of outer retinal tubulation and its influence on retreatment in neovascular age-related macular degeneration. BMC Ophthalmol. 2018;18:1–6.
Shah VP, Shah SA, Mrejen S, Freund KB. Subretinal hyperreflective exudation associated with neovascular age-related macular degeneration. Retina. 2014;34:1281–8.
Montolío-Marzo S, Gallego-Pinazo R, Palacios-Pozo E, Dolz-Marco R. Advantages of optical coherence tomography as a high dynamic range imaging modality in subretinal hyperreflective material. Retina. 2023;43:641–8.
Kumar JB, Stinnett S, Han JIL, Jaffe GJ. Correlation of subretinal hyperreflective material morphology and visual acuity in neovascular age-related macular degeneration. Retina. 2020;40:845–56.
Kawashima Y, Hata M, Oishi A, Ooto S, Yamashiro K, Tamura H, et al. Association of vascular versus avascular subretinal hyperreflective material with aflibercept response in age-related macular degeneration. Am J Ophthalmol. 2017;181:61–70.
Dansingani KK, Tan ACS, Gilani F, Phasukkijwatana N, Novais E, Querques L, et al. Subretinal hyperreflective material imaged with optical coherence tomography angiography. Am J Ophthalmol. 2016;169:235–48.
Willoughby AS, Ying GS, Toth CA, Maguire MG, Burns RE, Grunwald JE, et al. Subretinal hyperreflective material in the comparison of age-related macular degeneration treatments trials. Ophthalmology. 2015;122:1846–53.
Dolz-Marco R, Phasukkijwatana N, Sarraf D, Freund KB. Regression of type 2 neovascularization into a type 1 pattern after intravitreal anti-vascular endothelial growth factor therapy for neovascular age-related macular degeneration. Retina. 2017;37:222–33.
Sacconi R, Mullins RF, Lutty GA, Borrelli E, Bandello F, Querques G. Subretinal pseudocyst: a novel optical coherence tomography finding in age-related macular degeneration. Eur J Ophthalmol. 2020;30:NP24–6.
Menean M, Sacconi R, Vujosevic S, Kesim C, Quarta A, Ribarich N, et al. Subretinal pseudocysts: a comprehensive analysis of this novel OCT finding. Ophthalmol Ther. 2023;12:2035–48.
Fernández-Avellaneda P, Freund KB, Wang RK, He Q, Zhang Q, Fragiotta S, et al. Multimodal imaging features and clinical relevance of subretinal lipid globules. Am J Ophthalmol. 2021;222:112–25.
Monés J, Biarnés M, Trindade F. Hyporeflective wedge-shaped band in geographic atrophy secondary to age-related macular degeneration: an underreported finding. Ophthalmology. 2012;119:1412–9.
Sacconi R, Sarraf D, Sadda S, Freund K, Servillo A, Fogel Levin M, et al. Nascent geographic atrophy as a predictor of type 3 macular neovascularization development. Ophthalmol Retin. 2023;7:586–92.
Li M, Dolz-Marco R, Huisingh C, Messinger JD, Feist RM, Ferrara D, et al. Clinicopathologic correlation of geographic atrophy secondary to age-related macular degeneration. Retina. 2019;39:802–16.
Capuano GQ, Frascio V, Zweifel P, Georges S, Souied A. E. Wedge-shaped subretinal hyporeflectivity in geographic atrophy. Retina. 2015;35:1735–42.
Fragiotta S, Parravano M, Sacconi R, Costanzo E, Viggiano P, Prascina F, et al. A common finding in foveal-sparing extensive macular atrophy with pseudodrusen implicated basal laminar deposits. Retina. 2022;42:1319–29.
Tan ACS, Astroz P, Dansingani KK, Slakter JS, Yannuzzi LA, Curcio CA, et al. The evolution of the plateau, an optical coherence tomography signature seen in geographic atrophy. Invest Ophthalmol Vis Sci. 2017;58:2349–58.
Querques G, Costanzo E, Miere A, Capuano V, Souied EH. Choroidal caverns: a novel optical coherence tomography finding in geographic atrophy. Invest Ophthalmol Vis Sci. 2016;57:2578–82.
Dolz-Marco R, Glover JP, Gal-Or O, Litts KM, Messinger JD, Zhang Y, et al. Choroidal and sub-retinal pigment epithelium caverns: multimodal imaging and correspondence with friedman lipid globules. Ophthalmology. 2018;125:1287–301.
Fragiotta S, Parravano M, Costanzo E, De Geronimo D, Varano M, Fernandez-Avellaneda P, et al. Subretinal lipid globules an early biomarker of macular neovascularization in eyes with intermediate age-related macular degeneration. Retina. 2023;44:913–22.
Querques G, Srour M, Massamba N, Georges A, Ben Moussa N, Rafaeli O, et al. Functional characterization and multimodal imaging of treatment-naive “quiescent” choroidal neovascularization. Invest Ophthalmol Vis Sci. 2013;54:6886–92.
Narita C, Wu Z, Rosenfeld PJ, Yang J, Lyu C, Caruso E, et al. Structural OCT signs suggestive of subclinical nonexudative macular neovascularization in eyes with large drusen. Ophthalmology. 2020;127:637–47.
de Oliveira Dias JR, Zhang Q, Garcia JMB, Zheng F, Motulsky EH, Roisman L, et al. Natural history of subclinical neovascularization in nonexudative age-related macular degeneration using swept-source OCT angiography. Ophthalmology. 2018;125:255–66.
Csincsik L, Muldrew KA, Bettiol A, Wright DM, Rosenfeld PJ, Waheed NK, et al. The double layer sign is highly predictive of progression to exudation in age-related macular degeneration. Ophthalmol Retina. 2024;8:234–45.
Wang Y, Sun J, Wu J, Jia H, Feng J, Chen J, et al. Growth of nonexudative macular neovascularization in age-related macular degeneration: an indicator of biological lesion activity. Eye. 2023;37:2048–54.
Carnevali A, Cicinelli MV, Capuano V, Corvi F, Mazzaferro A, Querques L, et al. Optical coherence tomography angiography: a useful tool for diagnosis of treatment-naïve quiescent choroidal neovascularization. Am J Ophthalmol. 2016;169:189–98.
Rahimy E, Freund KB, Larsen M, Spaide RF, Costa RA, Hoang Q, et al. Multilayered pigment epithelial detachment in neovascular age-related macular degeneration. Retina. 2014;34:1289–95.
Soman M, Sheth JU, Indurkar A, Meleth P, Nair U. De-novo multilayering in fibrovascular pigment epithelial detachment. Sci Rep. 2021;11:1–10.
Mukai R, Sato T, Kishi S A. hyporeflective space between hyperreflective materials in pigment epithelial detachment and Bruch’s membrane in neovascular age-related macular degeneration. BMC Ophthalmol. 2014;14:159.
Kredi G, Iglicki M, Gomel N, Hilely A, Loewenstein A, Habot-Wilner Z, et al. Risk factors and clinical significance of prechoroidal cleft in eyes with neovascular age-related macular degeneration in Caucasian patients. Acta Ophthalmol. 2023;101:e338–45.
Pece A, Borrelli E, Sacconi R, Maione G, Bandello F, Querques G. Choroidal cleft simulating choroidal caverns in neovascular age-related macular degeneration. Eur J Ophthalmol. 2019;29:471–3.
Kim J, Kang S, Son D, Bae K. Risk factors and clinical significance of prechoroidal cleft in neovascular age-related macular degeneration. Retina. 2017;37:2047–55.
Kim J, Kim J, Kim C, Lee D. Long-term course and visual outcomes of prechoroidal cleft in neovascular age-related macular degeneration and polypoidal choroidal vasculopathy. Retina. 2021;41:2436–45.
Lee S, Kim KT, Kim DY, Chae JB, Seo EJ. Outer nuclear layer recovery as a predictor of visual prognosis in type 1 choroidal neovascularization of neovascular age-related macular degeneration. Sci Rep. 2023;13:1–10.
Pfau M, von der Emde L, de Sisternes L, Hallak J, Leng T, Schmitz-Valckenberg S, et al. Progression of photoreceptor degeneration in geographic atrophy secondary to age-related macular degeneration. JAMA Ophthalmol. 2020;138:1–9.
Cheong KX, Li H, Tham YC, Teo KYC, Tan ACS, Schmetterer L, et al. Relationship between retinal layer thickness and genetic susceptibility to age-related macular degeneration in Asian populations. Ophthalmol Sci. 2023;3:100396.
Zekavat SM, Sekimitsu S, Ye Y, Raghu V, Zhao H, Elze T, et al. Photoreceptor layer thinning is an early biomarker for age-related macular degeneration: epidemiologic and genetic evidence from UK Biobank OCT Data. Ophthalmology. 2022;129:694–707.
Farinha C, Silva AL, Coimbra R, Nunes S, Cachulo ML, Marques JP, et al. Retinal layer thicknesses and neurodegeneration in early age-related macular degeneration: insights from the Coimbra Eye Study. Graefes Arch Clin Exp Ophthalmol. 2021;259:2545–57.
Brandl C, Brücklmayer C, Günther F, Zimmermann ME, Küchenhoff H, Helbig H, et al. Retinal layer thicknesses in early age-related macular degeneration: results from the German AugUR study. Invest Ophthalmol Vis Sci. 2019;60:1581–94.
Zucchiatti I, Parodi MB, Pierro L, Cicinelli MV, Gagliardi M, Castellino N, et al. Macular ganglion cell complex and retinal nerve fiber layer comparison in different stages of age-related macular degeneration. Am J Ophthalmol. 2015;160:602–7.
Lee SW, Sim HE, Park JY, Kim JS, Chang IB, Park YS, et al. Changes in inner retinal layer thickness in patients with exudative age-related macular degeneration during treatment with anti-vascular endothelial growth factor. Medicine. 2020;99:E19955.
Sadda SR, Guymer R, Holz FG, Schmitz-Valckenberg S, Curcio CA, Bird AC, et al. Consensus definition for atrophy associated with age-related macular degeneration on OCT: classification of atrophy report 3. Ophthalmology. 2018;125:537–48.
Mitamura Y, Mitamura-Aizawa S, Katome T, Naito T, Hagiwara A, Kumagai K, et al. Photoreceptor impairment and restoration on optical coherence tomographic image. J Ophthalmol. 2013;2013:518170.
Sadda SVR, Abdelfattah NS, Lei J, Shi Y, Marion KM, Morgenthien E, et al. Spectral-domain OCT analysis of risk factors for macular atrophy development in the HARBOR study for neovascular age-related macular degeneration. Ophthalmology. 2020;127:1360–70.
Lindner M, Bezatis A, Czauderna J, Becker E, Brinkmann CK, Schmitz-Valckenberg S, et al. Choroidal thickness in geographic atrophy secondary to age-related macular degeneration. Invest Ophthalmol Vis Sci. 2015;56:875–82.
Foss A, Rotsos T, Empeslidis T, Chong V. Development of macular atrophy in patients with wet age-related macular degeneration receiving anti-VEGF treatment. Ophthalmologica. 2022;245:204–17.
Siedlecki J, Fischer C, Schworm B, Kreutzer TC, Luft N, Kortuem KU, et al. Impact of sub-retinal fluid on the long-term incidence of macular atrophy in neovascular age-related macular degeneration under treat & extend anti-vascular endothelial growth factor inhibitors. Sci Rep. 2020;10:1–8.
Toth CA, Tai V, Pistilli M, Chiu SJ, Winter KP, Daniel E, et al. Distribution of OCT features within areas of macular atrophy or scar after 2 years of anti-VEGF treatment for neovascular AMD in CATT. Ophthalmol Retin. 2019;3:316–25.
Eshtiaghi A, Issa M, Popovic M, Muni R, Kertes P. Geographic atrophy incidence and progression after intravitreal injections of anti-vascular endothelial growth factor agents for age-related macular degeneration: a meta-analysis. Retina. 2021;41:2424–35.
Christakis PG, Agrón E, Klein ML, Clemons TE, Campbell JP, Ferris FL, et al. Incidence of macular atrophy after untreated neovascular age-related macular degeneration: age-related eye disease study report 40. Ophthalmology. 2020;127:784–92.
Bhisitkul RB, Mendes TS, Rofagha S, Enanoria W, Boyer DS, Sadda SVR, et al. Macular atrophy progression and 7-year vision outcomes in subjects from the ANCHOR, MARINA, and HORIZON studies: The SEVEN-UP study. Am J Ophthalmol. 2015;159:915–24.e2.
Martin DF, Maguire MG, Fine SL, Ying GS, Jaffe GJ, Grunwald JE, et al. Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: two-year results. Ophthalmology. 2012;119:1388–98.
Gune S, Abdelfattah NS, Karamat A, Balasubramanian S, Marion KM, Morgenthien E, et al. Spectral-domain OCT–based prevalence and progression of macular atrophy in the HARBOR study for neovascular age-related macular degeneration. Ophthalmology. 2020;127:523–32.
Querques G, Capuano V, Costanzo E, Corvi F, Querques L, Introini U, et al. Retinal pigment epithelium aperture: A previously unreported finding in the evolution of avascular pigment epithelium detachment. Retina. 2016;36:S65–72.
Giannakaki-Zimmermann H, Querques G, Munch IC, Shroff D, Sarraf D, Chen X, et al. Atypical retinal pigment epithelial defects with retained photoreceptor layers: a so far disregarded finding in age related macular degeneration. BMC Ophthalmol. 2017;17:1–8.
Molina-Pallete R, Andreu-Fenoll M, Gallego-Pinazo R, Dolz-Marco R. Atypical healing in a case with retinal pigment epithelium apertures. Retin Cases Brief Rep. 2021;15:294–8.
Girgis J, Liu Y, Liang M, Baumal C, Duker J, Waheed N. Retinal pigment epithelium aperture preceding collapse of vascular and avascular pigment epithelial detachments secondary to AMD. Retin Cases Brief Rep. 2023. https://doi.org/10.1097/ICB.0000000000001435.
Ersoz MG, Karacorlu M, Arf S, Sayman Muslubas I, Hocaoglu M. Retinal pigment epithelium tears: classification, pathogenesis, predictors, and management. Surv Ophthalmol. 2017;62:493–505.
Iovino C, Chhablani J, Parameswarappa DC, Pellegrini M, Giannaccare G, Peiretti E. Retinal pigment epithelium apertures as a late complication of longstanding serous pigment epithelium detachments in chronic central serous chorioretinopathy. Eye. 2019;33:1871–6.
Clemens CR, Alten F, Eter N. Reading the signs: microrips as a prognostic sign for impending RPE tear development. Acta Ophthalmol. 2015;93:e600–2.
Fragiotta S, Scuderi L, Iodice CM, Rullo D, Di Pippo M, Maugliani E, et al. Choroidal vasculature changes in age-related macular degeneration: from a molecular to a clinical perspective. Int J Mol Sci. 2022;23:12010.
Invernizzi A, Benatti E, Cozzi M, Erba S, Vaishnavi S, Vupparaboina KK, et al. Choroidal structural changes correlate with neovascular activity in neovascular age related macular degeneration. Invest Ophthalmol Vis Sci. 2018;59:3836–41.
Borrelli E, Souied EH, Bailey Freund K, Querques G, Miere A, Gal-Or O, et al. Reduced choriocapillaris flow in eyes with type 3 neovascularization and age-related macular degeneration. Retina. 2018;38:1968–76.
Salehi MA, Mohammadi S, Gouravani M, Rezagholi F, Arevalo JF. Retinal and choroidal changes in AMD: a systematic review and meta-analysis of spectral-domain optical coherence tomography studies. Surv Ophthalmol. 2023;68:54–66.
Ting DSW, Ng WY, Ng SR, Tan SP, Yeo IYS, Mathur R, et al. Choroidal thickness changes in age-related macular degeneration and polypoidal choroidal vasculopathy: a 12-month prospective study. Am J Ophthalmol. 2016;164:128–36.e1.
Boscia G, Pozharitskiy N, Grassi MO, Borrelli E, D’Addario M, Alessio G, et al. Choroidal remodeling following different anti-VEGF therapies in neovascular AMD. Sci Rep. 2024;14:1–7.
Scharf JM, Corradetti G, Alagorie AR, Grondin C, Hilely A, Wang D, et al. Choriocapillaris flow deficits and treatment-naïve macular neovascularization secondary to age-related macular degeneration. Invest Ophthalmol Vis Sci. 2020;61:1–10.
Author information
Authors and Affiliations
Contributions
LVO was responsible for conducting the literature search, extracting, and analysing data, updating reference lists. PFA, SF, GC, and EB provided feedback on the report, adding new references, and creating figures. RDM was responsible for designing the review content, organizing the manuscript and list of features, creating figures and captions, and reviewing the manuscript.
Corresponding author
Ethics declarations
Competing interests
LVO reports travel expenses from Bayer; PFA is a consultant for Bayer and Roche; SF reports personal fees from Bayer (Advisor) outside the submitted work; GC none; EB is consultant to Abbvie, Bayer, Hofmann La Roche, Zeiss; RDM is consultant to Heidelberg Engineering and receives research funding from Roche, and Abbvie. The current manuscript received no funding.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vidal-Oliver, L., Fernández-Avellaneda, P., Fragiotta, S. et al. Non-exudative OCT findings in neovascular AMD. Eye 39, 516–526 (2025). https://doi.org/10.1038/s41433-024-03461-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-024-03461-y