Abstract
Objectives
To evaluate the differences in surgical outcomes between scleral buckling (SB) with noncryopexy and cryopexy methods.
Methods
We systematically searched the Embase, Medline, Cochrane Library, and Scopus databases for randomized controlled trials (RCTs) published from their inception until January 1, 2024. A random-effects model was applied, and outcomes are presented as risk ratios (RRs) or standardized mean differences with 95% confidence intervals (CIs). The certainty of evidence was assessed using the Grading of Recommendations Assessment, Development and Evaluation criteria.
Results
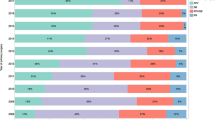
We included seven RCTs involving a total of 1103 patients. The meta-analysis revealed comparable retinal reattachment rates between noncryopexy and cryopexy methods (RR: 1.00; 95% CI: 0.96–1.05). Our subgroup analysis revealed similar results between nonretinopexy and laser retinopexy subgroups. Moreover, postoperative visual acuity (VA) and complication rates were comparable between noncryopexy and cryopexy methods (proportion of eyes with postoperative VA of 20/40 or better: RR: 1.24, 95% CI: 0.83–1.85; macular pucker: RR: 1.08, 95% CI: 0.53–2.21; cystoid macular oedema: RR: 1.01, 95% CI: 0.79–1.30; and subretinal pigmentary migration: RR: 0.34, 95% CI: 0.08–1.38). However, the certainty of evidence for these outcomes was low to very low, indicating the need for cautious interpretation of these findings.
Conclusions
Similar surgical outcomes were noted between noncryopexy and cryopexy methods in SB, suggesting that both methods are effective in repairing rhegmatogenous retinal detachment. However, future studies on a larger scale and with longer follow-ups may be necessary to detect late redetachment and complications.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The original contributions presented in this study are included in the article and its Supplementary Materials. Any additional inquiries or requests for data can be directed to the corresponding author.
References
Sultan ZN, Agorogiannis EI, Iannetta D, Steel D, Sandinha T. Rhegmatogenous retinal detachment: a review of current practice in diagnosis and management. BMJ Open Ophthalmol. 2020;5:e000474.
Ghazi NG, Green WR. Pathology and pathogenesis of retinal detachment. Eye (Lond). 2002;16:411–21.
Ge JY, Teo ZL, Chee ML, Tham YC, Rim TH, Cheng CY, et al. International incidence and temporal trends for rhegmatogenous retinal detachment: A systematic review and meta-analysis. Surv Ophthalmol. 2024;69:330–6.
Ryan EH, Ryan CM, Forbes NJ, Yonekawa Y, Wagley S, Mittra RA, et al. Primary Retinal Detachment Outcomes Study Report Number 2: Phakic Retinal Detachment Outcomes. Ophthalmology. 2020;127:1077–85.
Fallico M, Alosi P, Reibaldi M, Longo A, Bonfiglio V, Avitabile T, et al. Scleral Buckling: A Review of Clinical Aspects and Current Concepts. J Clin Med. 2022;11:314.
Figueroa MS, Corte MD, Sbordone S, Romano A, Alvarez MT, Villalba SJ, et al. Scleral buckling technique without retinopexy for treatment of rhegmatogeneous: a pilot study. Retin (Phila, Pa). 2002;22:288–93.
Mahdizadeh M, Masoumpour M, Ashraf H. Anatomical retinal reattachment after scleral buckling with and without retinopexy: a pilot study. Acta ophthalmologica. 2008;86:297–301.
Jaccoma EH, Conway BP, Campochiaro PA. Cryotherapy causes extensive breakdown of the blood-retinal barrier. A comparison with argon laser photocoagulation. Arch Ophthalmol. 1985;103:1728–30.
Campochiaro PA, Kaden IH, Vidaurri-Leal J, Glaser BM. Cryotherapy enhances intravitreal dispersion of viable retinal pigment epithelial cells. Arch Ophthalmol. 1985;103:434–6.
Singh AK, Michels RG, Glaser BM. Scleral indentation following cryotherapy and repeat cryotherapy enhance release of viable retinal pigment epithelial cells. Retina. 1986;6:176–8.
Cowley M, Conway BP, Campochiaro PA, Kaiser D, Gaskin H. Clinical risk factors for proliferative vitreoretinopathy. Arch Ophthalmol. 1989;107:1147–51.
Bonnet M, Guenoun S. Surgical risk factors for severe postoperative proliferative vitreoretinopathy (PVR) in retinal detachment with grade B PVR. Graefes Arch Clin Exp Ophthalmol. 1995;233:789–91.
Dunker S, Faulborn J, Haller EM, Reich ME. The effect of retinal cryoapplication on the vitreous. Retina. 1997;17:338–43.
Uemura A, Ideta H, Nagasaki H, Morita H, Ito K. Macular pucker after retinal detachment surgery. Ophthalmic Surg. 1992;23:116–9.
Avitabile T, Bartolotta G, Torrisi B, Reibaldi A. A randomized prospective study of rhegmatogenous retinal detachment cases treated with cryopexy versus frequency-doubled Nd:YAG laser-retinopexy during episcleral surgery. Retin (Phila, Pa). 2004;24:878–82.
Lira RPC, Takasaka I, Arieta CEL, Nascimento MA, Caldato R, Panetta H. Cryotherapy vs laser photocoagulation in scleral buckle surgery: A randomized clinical trial. Arch Ophthalmol (Chic, Ill: 1960). 2010;128:1519–22.
Mafi M, Mirghorbani M, Ghahvehchian H, Mohammadi SS, Riazi-Esfahani H, Khalili Pour E, et al. Modified Encircling Scleral Buckle Technique Without Subretinal Fluid Drainage or Retinopexy. Ophthalmol Ther. 2020;9:641–51.
Steel DH, West J, Campbell WG. A randomized controlled study of the use of transscleral diode laser and cryotherapy in the management of rhegmatogenous retinal detachment. Retin (Phila, Pa). 2000;20:346–57.
Veckeneer M, Van Overdam K, Bouwens D, Feron E, Mertens D, Peperkamp E, et al. Randomized clinical trial of cryotherapy versus laser photocoagulation for retinopexy in conventional retinal detachment surgery. Am J Ophthalmol. 2001;132:343–7.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Cheng J, Pullenayegum E, Marshall JK, Iorio A, Thabane L. Impact of including or excluding both-armed zero-event studies on using standard meta-analysis methods for rare event outcome: a simulation study. BMJ Open. 2016;6:e010983.
Catalá-López F, Tobías A. Meta-analysis of randomized trials, heterogeneity and prediction intervals. Med Clin (Barc). 2014;142:270–4.
Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Comparison of two methods to detect publication bias in meta-analysis. Jama. 2006;295:676–80.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
Axer-Siegel R, Yassur Y, Ben-Sira I. Surgical management of retinal detachment without cryopexy. Am J Ophthalmol. 1981;91:474–9.
Gao XX, Kang CY, Wang RF. Laser photocoagulation versus cryopexy in the treatment of rhegmatogenous retinal detachment. Int J Ophthalmol. 2010;10:1552–3.
Campochiaro PA, Jerdan JA, Glaser BM. Serum contains chemoattractants for human retinal pigment epithelial cells. Arch Ophthalmol. 1984;102:1830–3.
Campochiaro PA, Glaser BM. Platelet-derived growth factor is chemotactic for human retinal pigment epithelial cells. Arch Ophthalmol. 1985;103:576–9.
Acknowledgements
This manuscript was edited by Wallace Academic Editing.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
SMH was responsible for conceptualizing the study, supervising the research activities, and overseeing project administration. KYC and YCS contributed to the development of the methodology, carried out the investigation, and performed the statistical analyses. KYC drafted the initial version of the manuscript. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, KY., Su, YC. & Hsu, SM. Noncryopexy versus cryopexy treatment during scleral buckling: a systematic review and meta-analysis. Eye 39, 1292–1300 (2025). https://doi.org/10.1038/s41433-025-03614-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-03614-7