Abstract
Background
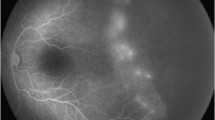
Retinopathy of prematurity (ROP) is one of the leading causes of preventable childhood blindness worldwide. There has been a rapid increase in neonatal units in Tanzania leading to increased survival of preterm babies, which lead to increasing number of babies at risk of ROP. ROP screening started in Tanzania for the first time in Muhimbili National Hospital in Dar es Salaam in late 2019. This study determines the prevalence and factors associated with ROP in Muhimbili hospital from June 2020 to February 2021.
Methods
A prospective cohort study was conducted among 193 preterm newborns with ≤34 weeks gestational age and ≤2000 g birth weight. ROP screening was performed using an indirect ophthalmoscope and 20D Volk lens on dilated fundus. Prevalence was determined as the proportion of babies with ROP. Cox regression model was used to assess the contribution of risk factors to the occurrence of ROP.
Results
The prevalence of ROP was 29% (56/193), and of type 1 ROP was 8.8%. Majority had zone two (73.2%) and 41.1% had stage two disease. Aggressive ROP constituted 8.9%. Significant factors for ROP development were gestational age <32 weeks (hazard ratio 6.8, p value 0.00), birth weight <1500 g (hazard ratio 2.1, p value 0.02), Apgar score <7 (hazard ratio 1.9, p value 0.03), RDS (hazard ratio 3.3, p value 0.01) and oxygen supplementation for >1 week (hazard ratio 0.74, p value 0.03). Surfactant use had a protective effect (hazard ratio 0.2, p value 0.03).
Conclusion
Prevalence of ROP is fairly high in our setting. Screening is essential to prevent visual morbidity and blindness resulting from ROP in the country.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data supporting the results reported in this article can be accessed by communicating with the corresponding author.
References
Hu Q, Bai Y, Chen X, Huang L, Chen Y, Li X. Recurrence of Retinopathy of Prematurity in Zone II Stage 3+ after Ranibizumab Treatment: A Retrospective Study. J Ophthalmol. 2017;3:1–5.
Shah PK, Prabhu V, Karandikar SS, Ranjan R, Narendran V, Kalpana N. Retinopathy of prematurity: Past, present and future. World J Clin Pediatr. 2016;5:35–46.
Tanzania : Profile of preterm and low birth weight prevention and care. 2024. Available from: http://reliefweb.int/report/united-republic-tanzania/tanzania-profile-preterm-and-low-birth-weight-prevention-and-care.
Blencowe H, Lawn JE, Vazquez T, Fielder A, Gilbert C. Preterm-associated visual impairment and estimates of retinopathy of prematurity at regional and global levels for 2010. Pediatr Res. 2013;74:35–49.
Smith BT, Tasman WS. Retinopathy of prematurity: late complications in the baby boomer generation (1946-1964). Trans Am Ophthalmol Soc. 2005;103:225–36.
Heidary F, Gharebaghi R. Outcomes of Retinopathy of Prematurity. Med Hypothesis Discov Innov Ophthalmol. 2016;5:112–4.
Bas AY, Demirel N, Koc E, Ulubas Isik D, Hirfanoglu İM, Tunc T, et al. Incidence, risk factors and severity of retinopathy of prematurity in Turkey (TR-ROP study): a prospective, multicentre study in 69 neonatal intensive care units. Br J Ophthalmol. 2018;102:1711–6.
Owen LA, Morrison MA, Hoffman RO, Yoder BA, DeAngelis MM. Retinopathy of prematurity: A comprehensive risk analysis for prevention and prediction of disease. PLoS One. 2017;12:1–14.
Sonksen PM, Dale N. Visual impairment in infancy: impact on neurodevelopmental and neurobiological processes. Dev Med Child Neurol. 2002;44:782–91.
Senjam SS, Chandra P. Retinopathy of prematurity: Addressing the emerging burden in developing countries. J Family Med Prim Care. 2020;9:2600–5.
International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol. 2005;123:991–9.
Zarei M, Bazvand F, Ebrahimiadib N, Roohipoor R, Karkhaneh R, Farahani Dastjani A, et al. Prevalence and Risk Factors of Retinopathy of Prematurity in Iran. J Ophthalmic Vis Res. 2019;14:291–8.
Hakeem AHAA, Mohamed GB, Othman MF. Retinopathy of prematurity: a study of prevalence and risk factors. Middle East Afr J Ophthalmol. 2012;19:289–94.
Van der Merwe SK, Freeman N, Bekker A, Harvey J, Smith J. Prevalence of and risk factors for retinopathy of prematurity in a cohort of preterm infants treated exclusively with non-invasive ventilation in the first week after birth. S Afr Med J. 2013;103:96–100.
Onyango O, Sitati S, Amolo L, Murila F, Wariua S, Nyamu G, et al. Retinopathy of prematurity in Kenya: prevalence and risk factors in a hospital with advanced neonatal care. Pan Afr Med J. 2018;29:152.
Abbasi N, Ramezani M, Shoeibi N, Vashani HB. Astudy of the prevalence and severity of retinopathy of prematurity in East of Iran during 2015–2017: A descriptive cross-sectional study. J Neonatal Nurs. 2022;28:244–8.
Akkawi MT, Shehadeh MM, Shams ANA, Al-Hardan DM, Omar LJ, Almahmoud OH, et al. Incidence and risk factors of retinopathy of prematurity in three neonatal intensive care units in Palestine. BMC Ophthalmol. 2019;19:189.
Khorshidifar M, Nikkhah H, Ramezani A, Entezari M, Daftarian N, Norouzi H, et al. Incidence and risk factors of retinopathy of prematurity and utility of the national screening criteria in a tertiary center in Iran. Int J Ophthalmol. 2019;12:1330–6.
Bassiouny RR, Ellakkany R, Aboelkhair S, Mohsen T, Othman I. Incidence and risk factors of retinopathy of prematurity in neonatal intensive care units: Mansoura, Egypt. J Egypt Ophthalmol Soc. 2017;110:71–6.
Adio AO, Ugwu RO, Nwokocha CG, Eneh AU Retinopathy of prematurity in port harcourt, Nigeria. ISRN Ophthalmol. 2014:481527. https://doi.org/10.1155/2014/481527.
Rasoulinejad SA, Montazeri M. Retinopathy of Prematurity in Neonates and its Risk Factors: A Seven Year Study in Northern Iran. Open Ophthalmol J. 2016;10:17–21.
Celebi ARC, Petricli IS, Hekimoglu E, Demirel N, Bas AY. The incidence and risk factors of severe retinopathy of prematurity in extremely low birth weight infants in Turkey. Med Sci Monit. 2014;20:1647–53.
Fajolu IB, Rotimi-Samuel A, Aribaba OT, Musa KO, Akinsola FB, Ezeaka VC, et al. Retinopathy of prematurity and associated factors in Lagos, Nigeria. Paediatr Int Child Health. 2015;35:324–8.
Braimah IZ, Enweronu-Laryea C, Sackey AH, Kenu E, Agyabeng K, Ofori-Adjei IODB, et al. Incidence and risk factors of retinopathy of prematurity in Korle-Bu Teaching Hospital: a baseline prospective study. BMJ Open. 2020;10:e035341.
Holmström G, Thomassen P, Broberger U. Maternal risk factors for retinopathy of prematurity-a population-based study. Acta Obstet Gynecol Scand. 1996;75:628–35.
Kubrey SS, Maravi P, Kushwaha N, Sharma P, Dubey A, Kumar K. Influence of maternal factors on retinopathy of prematurity: A cross-sectional Study from a tertiary care centre. Indian J Clin Exp Ophthalmol. 2023;9:359–64.
Author information
Authors and Affiliations
Contributions
YM was responsible for designing and conducting the research, extracting and analysing data, interpreting results and writing report. CM was responsible for designing the research, extracting and analysing data, interpreting results and writing report. MM was responsible for designing the research and providing feedback on the report. AS was responsible for designing the research and providing feedback on the report. NSM was responsible for designing the research and providing feedback on the report. AM designed the study, analysed the data, interpreted the results and edited the report.
Corresponding author
Ethics declarations
Competing interests
There are no competing interests to declare.
Ethical approval and consent to participate
This study was approved by the Institutional Review Board (IRB) of Muhimbili University of Health and Allied Sciences (MUHAS-REC-06-2020-292). The principles of the Declaration of Helsinki were followed. Written informed consent was obtained from the parents of all the participants enroled in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mhina, C., Mtogo, Y., Mafwiri, M. et al. Prevalence and associated factors for retinopathy of prematurity at a tertiary hospital in Dar es Salaam, Tanzania. Eye 39, 1476–1480 (2025). https://doi.org/10.1038/s41433-025-03651-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-03651-2
This article is cited by
-
Prevalence and associated factors of retinopathy of prematurity in sub‑Saharan Africa: a systematic review and meta‑analysis
BMC Ophthalmology (2025)
-
Construction of a predictive model for retinopathy of prematurity using machine learning algorithms
BMC Ophthalmology (2025)
-
The aftermath of retinopathy of prematurity blindness
Eye (2025)