Abstract
Objectives
To explore the changes in eye structures over time in the Chinese population from the perspective of birth year.
Methods
We collected measurement data of intraocular lens Master from patients who underwent intraocular lens Master biometry for a routine cataract or refractive examination (ametropia and presbyopia) between April 2012 and October 2023, then screened them. Selected patients were divided into ten groups of 10 years each according to their year of birth (called birth decades). Birth-year–dependent changes in axial length and corneal curvature were compared between the groups.
Results
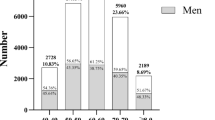
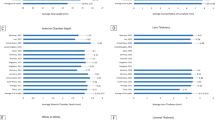
The average axial length increased from 23.52 mm to 25.95 mm, and the corneal curvature dropped from 44.20 D to 43.33 D in patients born in before-1930 and 1990s. The proportion of short average axial length and steep corneal curvature decreased, whereas the proportion of long average axial length increased with the birth decade. The proportion of patients with corneal curvature < 40 D was 4.18% in 1970s, 5.73% in 1980s, and 3.38% in 1990s, which were significantly higher than those of other age groups. The average axial length of the eyes among primary school students was 23.96 mm, and among college students, it was 25.86 mm.
Conclusions
Overall, with the birth decade, average axial length increased and corneal curvature decreased. There were generational differences in ocular biological parameters, changes in the eye might affect the incidence of eye diseases such as glaucoma and fundus diseases, which in turn might lead to changes in the spectrum of eye diseases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data supporting the findings of this study are not publicly accessible due to privacy concerns and can be available from the corresponding author upon reasonable request.
References
Nakao SY, Miyake M, Hosoda Y, Nakano E, Mori Y, Takahashi A, et al. Myopia prevalence and ocular biometry features in a general Japanese population: The Nagahama study. Ophthalmology. 2021;128:522–31.
Koch DD, Liu JF, Hyde LL, Rock RL, Emery JM. Refractive complications of cataract surgery after radial keratotomy. Am J Ophthalmol. 1989;108:676–82.
Ren Y, Castro CB, Peng Y, Glauben T. Nutrition transition with accelerating urbanization? Empirical evidence from rural China. Nutrients. 2021;13:921.
Ye X, Zhu D, Ding R, He P. The effect of China’s compulsory education reforms on physiological health in adulthood: a natural experiment. Health Policy Plan. 2022;37:376–84.
Li W, Cui Y, Gong Q, Zhu Z. Association of smartphone use duration with physical fitness among University students: focus on strength and flexibility. Int J Env Res Pub He. 2022;19:7386.
Osailan A. The relationship between smartphone usage duration (using smartphone’s ability to monitor screen time) with hand-grip and pinch-grip strength among young people: an observational study. Bmc Musculoskel Dis. 2021;22:186.
He M, Xiang F, Zeng Y, Mai J, Chen Q, Zhang J, et al. Effect of Time spent outdoors at school on the development of myopia among children in China: A randomized clinical trial. Jama-J Am Med Assoc. 2015;314:1142–8.
Bourke CM, Loughman J, Flitcroft DI, Loskutova E, O Brien C. We can’t afford to turn a blind eye to myopia. Int J Med. 2023;116:635–9.
Chen Z, Gu D, Wang B, Kang P, Watt K, Yang Z, et al. Significant myopic shift over time: Sixteen-year trends in overall refraction and age of myopia onset among Chinese children, with a focus on ages 4-6 years. J Glob Health. 2023;13:4144.
Dolgin E. The myopia boom. Nature. 2015;519:276–8.
Morgan IG, French AN, Ashby RS, Guo X, Ding X, He M, et al. The epidemics of myopia: Aetiology and prevention. Prog Retin Eye Res. 2018;62:134–49.
Kumagai K, Ogino N, Horie E, Fukami M, Furukawa M, Matsumura M, et al. Birth year-dependent increase in axial length of Japanese adult. Am J Ophthalmol. 2021;232:98–108.
Bullimore MA, Lee SS, Schmid KL, Rozema JJ, Leveziel N, Mallen E, et al. IMI-onset and progression of myopia in young adults. Invest Ophth Vis Sci. 2023;64:2.
Wolffsohn JS, Jong M, Smith ER, Resnikoff SR, Jonas JB, Logan NS, et al. IMI 2021 Reports and digest - reflections on the implications for clinical practice. Invest Ophth Vis Sci. 2021;62:1.
Myopia stabilization and associated factors among participants in the Correction of Myopia Evaluation Trial (COMET). Invest Ophth Vis Sci 2013;54:7871–84.
Brennan NA, Toubouti YM, Cheng X, Bullimore MA. Efficacy in myopia control. Prog Retin Eye Res. 2021;83:100923.
Jan C, Xu R, Luo D, Xiong X, Song Y, Ma J, et al. Association of visual impairment with economic development among Chinese schoolchildren. Jama Pediatr. 2019;173:e190914.
Benzir M, Afroze A, Zahan A, Naznin RA, Khanam A, Sumi SA, et al. A study linking axial length, corneal curvature, and eye axis with demographic characteristics in the emmetropic eyes of Bangladeshi people. Cureus J Med Sci. 2022;14:e29925.
Tideman J, Polling JR, Vingerling JR, Jaddoe V, Williams C, Guggenheim JA, et al. Axial length growth and the risk of developing myopia in European children. Acta Ophthalmol. 2018;96:301–9.
Vongphanit J, Mitchell P, Wang JJ. Prevalence and progression of myopic retinopathy in an older population. Ophthalmology. 2002;109:704–11.
Congdon N, Wang F, Tielsch JM. Issues in the epidemiology and population-based screening of primary angle-closure glaucoma. Surv Ophthalmol. 1992;36:411–23.
Wong TY, Loon SC, Saw SM. The epidemiology of age related eye diseases in Asia. Brit J Ophthalmol. 2006;90:506–11.
Neoh FP, Y A, Siti AA, Liza-Sharmini AT. Anterior segment biometry in primary angle closure glaucoma patients with visual field progression: comparison between Malays and Chinese. J Curr Glaucoma Pract. 2023;17:3–8.
Wang Z, Wiggs JL, Aung T, Khawaja AP, Khor CC. The genetic basis for adult onset glaucoma: Recent advances and future directions. Prog Retin Eye Res. 2022;90:101066.
Sun X, Dai Y, Chen Y, Yu DY, Cringle SJ, Chen J, et al. Primary angle closure glaucoma: What we know and what we don’t know. Prog Retin Eye Res. 2017;57:26–45.
Fan NW, Hwang DK, Ko YC, Tseng FC, Hung KH, Liu CJ. Risk factors for progressive visual field loss in primary angle-closure glaucoma: a retrospective cohort study. Plos One. 2013;8:e69772.
Li S, Shao M, Wan Y, Tang B, Sun X, Cao W. Relationship between ocular biometry and severity of primary angle-closure glaucoma: relevance for predictive, preventive, and personalized medicine. Epma J. 2019;10:261–71.
Yong KL, Gong T, Nongpiur ME, How AC, Lee HK, Cheng L, et al. Myopia in Asian subjects with primary angle closure: implications for glaucoma trends in East Asia. Ophthalmology. 2014;121:1566–71.
Lowe RF. Aetiology of the anatomical basis for primary angle-closure glaucoma. Biometrical comparisons between normal eyes and eyes with primary angle-closure glaucoma. Brit J Ophthalmol. 1970;54:161–9.
Xu L, Wang Y, Wang S, Wang Y, Jonas JB. High myopia and glaucoma susceptibility the Beijing Eye Study. Ophthalmology. 2007;114:216–20.
Marcus MW, de Vries MM, Junoy MF, Jansonius NM. Myopia as a risk factor for open-angle glaucoma: a systematic review and meta-analysis. Ophthalmology. 2011;118:1989–94.
Oku Y, Oku H, Park M, Hayashi K, Takahashi H, Shouji T, et al. Long axial length as risk factor for normal tension glaucoma. Graef Arch Clin Exp. 2009;247:781–7.
Haarman A, Enthoven CA, Tideman J, Tedja MS, Verhoeven V, Klaver C. The complications of myopia: a review and meta-analysis. Invest Ophth Vis Sci. 2020;61:49.
Ha A, Kim CY, Shim SR, Chang IB, Kim YK. Degree of myopia and glaucoma risk: a dose-response meta-analysis. Am J Ophthalmol. 2022;236:107–19.
Song P, Wang J, Bucan K, Theodoratou E, Rudan I, Chan KY. National and subnational prevalence and burden of glaucoma in China: A systematic analysis. J Glob Health. 2017;7:20705.
Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012;31:622–60.
Stulting RD, Carr JD, Thompson KP, Waring GR, Wiley WM, Walker JG. Complications of laser in situ keratomileusis for the correction of myopia. Ophthalmology. 1999;106:13–20.
Shojaei A, Mohammad-Rabei H, Eslani M, Elahi B, Noorizadeh F. Long-term evaluation of complications and results of photorefractive keratectomy in myopia: an 8-year follow-up. Cornea. 2009;28:304–10.
Acknowledgements
a. Funding/Support: This study was supported by Natural Science Foundation of Hubei Province of China (2023AFB053), Cultivation Fund for Science and Technology Innovation of Zhongnan Hospital of Wuhan University (ZNYYIIT20200507) of China and the 72nd batch of grant from China Postdoctoral Science Foundation (2022M722463). The funders played no role in the study design, data collection, analysis, decision to publish, or manuscript preparation. b. Financial Disclosures: None of the authors has proprietary interests in any product described in this article or any conflicts of interest.
Funding
Supported by Natural Science Foundation of Hubei Province of China (2023AFB053), Cultivation Fund for Science and Technology Innovation of Zhongnan Hospital of Wuhan University (ZNYYIIT20200507) of China and the 72nd batch of grant from China Postdoctoral Science Foundation (2022M722463).
Author information
Authors and Affiliations
Contributions
MK and Liang Liang developed the concept of the study, contributed to writing the article and supervision of the project. Lufan Li and NZ contributed the writing of the article, data collection, interpretation and analysis. XW, QW, RL collaborated in initial data collection and contribution to the first draft. RH, LY, YH, WL, YF and BJ collected the patient data and assisted in drafting the manuscript. XC, WZ, YL and FL read and revised the manuscript. All authors approved the manuscript and this submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, L., Zhang, N., Wang, X. et al. Changes in eye axis length and corneal curvature in central China from the perspective of birth year. Eye 39, 1373–1379 (2025). https://doi.org/10.1038/s41433-025-03652-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-03652-1