Abstract
Background
Intraocular metastases from cutaneous melanoma are rare. Diagnosis can be challenging and there is currently no consensus on treatment. However, with the increasing incidence of this cancer and improved survival of patients treated with targeted BRAF-MEK inhibitors and checkpoint inhibitors, it is likely that more cases will be referred to ocular oncology clinics.
Subjects
Single-centre retrospective study. We included all the patients diagnosed with intraocular metastases from cutaneous melanoma seen between 2017 and 2022.
Results
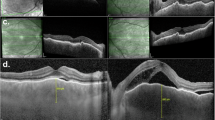
The first patient had bilateral choroidal metastases and unilateral vitreous cells (treated with external beam radiotherapy and immunotherapy), the second had unilateral amelanotic vitreous metastasis (treated with vitrectomy and BRAF-MEK inhibitors) and the third had bilateral multifocal choroidal metastases (treated with BRAK-MEK inhibitors followed by immunotherapy). The fourth patient (previously reported) had unilateral anterior segment and vitreous metastases (treated with immunotherapy and enucleation). Interestingly, two patients had a history of uveitis in the affected eye, unrelated to the ocular metastases. All four patients had synchronous systemic metastases.
Conclusions
The diagnosis of intraocular metastases from cutaneous melanoma is generally clinical but it is sometimes challenging because of possible masquerade syndromes. The presence of other extraocular metastatic sites is an indicator of the diagnosis. Cytopathologic proof combined with genetic analysis is sometimes necessary for diagnosis, especially with amelanotic vitreous debris or in rare cases where systemic screening is negative. New treatments with targeted BRAF-MEK inhibitors and checkpoint inhibition may avoid external beam radiotherapy and enucleation in some patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others

Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request. Data are located in controlled access data storage at Moorfields Eye Hospital.
References
Eisemann N, Schumann L, Baltus H, Labohm L, Kraywinkel K, Katalinic A. Longer survival from melanoma in Germany. Dtsch Arztebl Int. 2024;121:45–51.
Dummer R, Rozati S, Eggmann N, Rinderknecht J, Goldinger SM. From chemotherapy to targeted treatment. Ann Oncol. 2012;23:x101–3.
Robert C, Grob JJ, Stroyakovskiy D, Karaszewska B, Hauschild A, Levchenko E, et al. Five-year outcomes with dabrafenib plus trametinib in metastatic melanoma. N Engl J Med. 2019;381:626–36.
Larkin J, Chiarion-Sileni V, Gonzalez R, Grob J-J, Rutkowski P, Lao CD, et al. Five-year survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med. 2019;381:1535–46.
Fernandez-Diaz AB, García-Medina A, Ferrer-Guillen B, Berrocal A. Eye immune privilege? Nivolumab plus ipilimumab: successful treatment in a patient with cutaneous melanoma and ocular metastases. Melanoma Res. 2019;29:345–7.
Szalai E, Csutak A, Lengyel Z. Complete resolution of bilateral choroidal metastases of cutaneous melanoma with combined targeted therapy. Retina. 2021;41:e30–1.
Venkat A, Binkley EM, Srivastava S, Karthik N, Singh AD. Immunotherapy-resistant vitreoretinal metastatic melanoma. Ocul Oncol Pathol. 2021;7:62–5.
Sia DIT, Thaung C, O’Hanlon-Brown C, Cohen VML, Sagoo MS. Immune privilege: failure of immunotherapy in controlling metastatic cutaneous melanoma to the eye. Melanoma Res. 2018;28:359–62.
Grajewski RS, Schuler-Thurner B, Mauch C, Kreuzberg N, Koch KR, Bergua A, et al. Ocular diseases in metastatic cutaneous melanoma: review of 108 consecutive patients in two German tertiary centers. Graefes Arch Clin Exp Ophthalmol. 2014;252:679–85.
Thrift AP, Gudenkauf FJ. Melanoma incidence among non-Hispanic Whites in all 50 US states from 2001 through 2015. J Natl Cancer Inst. 2020;112:533–9.
Pampena R, Michelini S, Lai M, Chester J, Pellacani G, Longo C. New systemic therapies for cutaneous melanoma: why, who and what. Ital J Dermatol Venerol. 2021;156:344–55.
Antoun J, Titah C, Cochereau I. Ocular and orbital side-effects of checkpoint inhibitors: a review article. Curr Opin Oncol. 2016;28:288–94.
Méndez-Martínez S, Calvo P, Ruiz-Moreno O, Pardiñas Barón N, Leciñena Bueno J, Gil Ruiz MDR, et al. Ocular adverse events associated with MEK inhibitors. Retina. 2019;39:1435–50.
Fauviaux E, Promelle V, Boucenna V, Jany B, Errera MH, Delbarre M, et al. [Ocular toxicity of targeted therapies with MEK inhibitors and BRAF inhibitors in the treatment of metastatic cutaneous melanoma]. J Fr Ophtalmol. 2022;45:612–8.
Arepalli S, Kaliki S, Shields CL. Choroidal metastases: origin, features, and therapy. Indian J Ophthalmol. 2015;63:122–7.
Rosenberg C, Finger PT. Cutaneous malignant melanoma metastatic to the eye, lids, and orbit. Surv Ophthalmol. 2008;53:187–202.
Adler NR, Haydon A, McLean CA, Kelly JW, Mar VJ. Metastatic pathways in patients with cutaneous melanoma. Pigment Cell Melanoma Res. 2017;30:13–27.
Francis JH, Berry D, Abramson DH, Barker CA, Bergstrom C, Demirci H, et al. Intravitreous cutaneous metastatic melanoma in the era of checkpoint inhibition: unmasking and masquerading. Ophthalmology. 2020;127:240–8.
Everett L, Damato BE, Bloomer MM, Palmer JD, Kao AA, Stewart JM, et al. Metastatic cutaneous melanoma presenting with choroidal metastasis simulating primary uveal melanoma. Ocul Oncol Pathol. 2019;5:135–8.
Rieth JM, Bowen RC, Milhem MM, Boldt HC, Binkley EM. Presumed Melanoma of unknown primary origin metastatic to the choroid mimics primary uveal melanoma. Case Rep. Ophthalmol. 2021;12:987–93.
Iorgulescu JB, Harary M, Zogg CK, Ligon KL, Reardon DA, Hodi FS, et al. Improved risk-adjusted survival for melanoma brain metastases in the era of checkpoint blockade immunotherapies: results from a national cohort. Cancer Immunol Res. 2018;6:1039–45.
McDonald MA, Sanghvi P, Bykowski J, Daniels GA. Unmasking of intracranial metastatic melanoma during ipilimumab/nivolumab therapy: case report and literature review. BMC Cancer. 2018;18:549.
Gündüz K, Shields JA, Shields CL, Eagle RC. Cutaneous melanoma metastatic to the vitreous cavity. Ophthalmology. 1998;105:600–5.
Francis JH, Canestraro J, Abramson DH, Barker CA, Shoushtari AN. Combination intravitreous melphalan and bevacizumb for cutaneous metastatic melanoma to the vitreous and retina. Am J Ophthalmol Case Rep. 2022;26:101519.
Acknowledgements
The authors would like to thank Lamis Al Harby for her contribution to this work.
Author information
Authors and Affiliations
Contributions
SL—study conception and design, data collection, analysis and interpretation of results, manuscript preparation. AKA—data collection, analysis and interpretation of results. GRH—data collection, analysis and interpretation of results. MSS—study conception and design, analysis and interpretation of results, manuscript preparation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lemaître, S., Arora, A.K., Hay, G.R. et al. Spectrum of presentation of intraocular metastases from cutaneous melanoma in the era of immunotherapy and targeted therapies. Eye 39, 1825–1830 (2025). https://doi.org/10.1038/s41433-025-03753-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-03753-x