Abstract
Purpose
To study the outcome of the first dose versus three monthly doses of 2 mg aflibercept in the initiation phase of neovascular age-related macular degeneration (nAMD) to inform future clinical trial design on novel durable agents. These agents may take time to act and so initial dosing with aflibercept 2 mg is required for immediate effect.
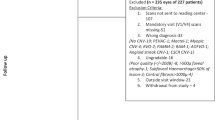
Methods
Visual acuity (VA) outcomes and associations with baseline VA and OCT characteristics were analysed using logistic regression via generalised estimating equations. In addition, VA outcomes based on different combinations of eligibility criteria were assessed.
Results
A total of 1999 eyes of 1862 patients were analysed. The mean age was 79.3 (SD 7.8) years. The mean presenting VA was 58.0 (SD 14.5) ETDRS letter score. A statistical difference in VA was found after first injection (visit 2, 61.6, SD 14.3 ETDRS letter score) and after three monthly injections (visit 4, 62.7, SD 14.9 ETDRS letter score) (P < 0.001). Lower baseline VA and OCT features suggestive of structural changes in the fovea are associated with lower VA after both first and post- initiating doses. Eyes with baseline VA > / = 54 letters alone had similar VA outcomes to eyes with both VA > / = 54 letters and central subfield thickness (CST) of <500 microns.
Conclusion
Mean VA outcomes after three monthly anti-VEGF injections are significantly better than after the first initiating dose. However, baseline OCT characteristics associated with VA in these two timepoints are not clinically different.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The anonymised PRECISE clinical database analysed during the current study is available from author SS on approval of a data sharing agreement with Moorfields Eye Hospital. Sharing of retinal images requires patient consent and sponsor approval.
References
Ferris FL III, Fine SL, Hyman L. Age-related macular degeneration and blindness due to neovascular maculopathy. Arch Ophthalmol. 1984;102:1640–2.
Heier JS, Brown DM, Chong V, Korobelnik JF, Kaiser PK, Nguyen QD, et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology. 2012;119:2537–48.
Schmidt-Erfurth U, Waldstein SM. A paradigm shift in imaging biomarkers in neovascular age-related macular degeneration. Prog Retin Eye Res. 2016;50:1–24.
Zur D, Guymer R, Korobelnik JF, Wu L, Viola F, Eter N, et al. Impact of residual retinal fluid on treatment outcomes in neovascular age-related macular degeneration. Br J Ophthalmol. 2024;bjo-2024-325640.
Chandra S, Gurudas S, Burton BJL, Menon G, Pearce I, Mckibbin M, et al. Associations of presenting visual acuity with morphological changes on OCT in neovascular age-related macular degeneration: PRECISE Study Report 2. Eye(Lond). 2024;38:757–65.
Chandra S, Gurudas S, Pearce I, Mckibbin M, Kotagiri A, Menon G, et al. Baseline characteristics of eyes with early residual fluid post loading phase of aflibercept therapy in neovascular AMD: PRECISE study report 3. Eye (Lond). 2024;38:1301–7.
Amoaku WM, Chakravarthy U, Gale R, Gavin M, Ghanchi F, Gibson J, et al. Defining response to anti-VEGF therapies in neovascular AMD. Eye. 2015;29:721–31.
Khanani AM, Aziz AA, Khan H, Gupta A, Mojumder O, Saulebayeva A, et al. The real-world efficacy and safety of faricimab in neovascular age-related macular degeneration: the TRUCKEE study - 6 month results. Eye (Lond). 2023;37:3574–81.
Bilgic A, Kodjikian L, Mathis T, Sudhalkar AA, Vasavada SA, Bhojwani DM. Single injection response to antivascular endothelial growth factor agents in patients with wet age-related macular degeneration: incidence and characteristics. Retina. 2021;41:1901–10.
Wiryasaputra S, Nguyen V, Arnold JJ, Ferrier R, Hinchcliffe P, Barthelmes D, et al. Four-week outcomes of vascular endothelial growth factor inhibitors for neovascular age-related macular degeneration. Clin Exp Ophthalmol. 2020;48:946–55.
Carlà MM, Savastano MC, Boselli F, Giannuzzi F, Rizzo S. Ranibizumab port delivery system in neovascular age-related macular degeneration: where do we stand? overview of pharmacokinetics, clinical results, and future directions. Pharmaceutics. 2024;16:314.
Khanani AM, Thomas MJ, Aziz AA, Weng CY, Danzig CJ, Yiu G, et al. Review of gene therapies for age-related macular degeneration. Eye. 2022;36:303–11.
Samanta A, Aziz AA, Jhingan M, Singh SR, Khanani AM, Chhablani J. Emerging therapies in neovascular age-related macular degeneration in 2020. Asia-Pac J Ophthalmol Philos Pa. 2020;9:250–9.
Chandra S, Tan EY, Empeslidis T, Sivaprasad S. Tyrosine kinase inhibitors and their role in treating neovascular age-related macular degeneration and diabetic macular oedema. Eye. 2023;37:3725–33.
Chorev M, Haderlein J, Chandra S, Menon G, Burton BJL, Pearce I, et al. A multi-modal ai-driven cohort selection tool to predict suboptimal non-responders to aflibercept loading-phase for neovascular age-related macular degeneration: PRECISE study report 1. J Clin Med. 2023;12:3013.
Dugel PU, Singh RP, Koh A, Ogura Y, Weissgerber G, Gedif K, et al. HAWK and HARRIER: ninety-six-week outcomes from the phase 3 trials of brolucizumab for neovascular age-related macular degeneration. Ophthalmology. 2021;128:89–99.
Heier JS, Khanani AM, Quezada Ruiz C, Basu K, Ferrone PJ, Brittain C, et al. TENAYA and LUCERNE Investigators. Efficacy, durability, and safety of intravitreal faricimab up to every 16 weeks for neovascular age-related macular degeneration (TENAYA and LUCERNE): two randomised, double-masked, phase 3, non-inferiority trials. Lancet. 2022;399:729–40.
Lydersen S, Skovlund E. Do not adjust for the baseline value in observational studies. Tidsskr Den Nor Legeforening. 2021;141. https://tidsskriftet.no/en/2021/11/medicine-and-numbers/do-not-adjust-baseline-value-observational-studies.
Yamashiro K, Oishi A, Hata M, Takahashi A, Tsujikawa A. Visual acuity outcomes of anti-VEGF treatment for neovascular age-related macular degeneration in clinical trials. Jpn J Ophthalmol. 2021;65:741–60.
Ying GS, Maguire MG, Daniel E, Ferris FL, Jaffe GJ, Grunwald JE, et al. Association of baseline characteristics and early vision response with two-year vision outcomes in the comparison of AMD treatments trials (CATT). Ophthalmology. 2015;122:2523–2531.e1.
Ying GS, Huang J, Maguire MG, Jaffe GJ, Grunwald JE, Toth C, et al. Baseline predictors for one year visual outcomes with ranibizumab or bevacizumab for neovascular age-related macular degeneration. Ophthalmology. 2013;120:122–9.
Writing Committee for the UK Age-Related Macular Degeneration EMR Users Group. The Neovascular Age-Related Macular Degeneration Database: Multicenter Study of 92 976 Ranibizumab Injections. Ophthalmology. 2014;121:1092–101.
Talks JS, Lotery AJ, Ghanchi F, Sivaprasad S, Johnston RL, Patel N, et al. First-year visual acuity outcomes of providing aflibercept according to the VIEW study protocol for age-related macular degeneration. Ophthalmology. 2016;123:337–43.
Mehta H, Kim LN, Mathis T, Zalmay P, Ghanchi F, Amoaku WM, et al. Trends in real-world neovascular AMD treatment outcomes in the UK. Clin Ophthalmol Auckl NZ. 2020;14:3331–42.
Lanzetta P, Korobelnik JF, Heier JS, Leal S, Holz FG, Clark WL, et al. Intravitreal aflibercept 8 mg in neovascular age-related macular degeneration (PULSAR): 48-week results from a randomised, double-masked, non-inferiority, phase 3 trial. Lancet. 2024;403:1141–52.
Patel S, Storey PP, Barakat MR, Hershberger V, Bridges WZ, Eichenbaum DA, et al. Phase I DAVIO Trial: EYP-1901 bioerodible, sustained-delivery vorolanib insert in patients with wet age-related macular degeneration. Ophthalmol Sci. 2024;4:100527.
Fasler K, Moraes G, Wagner S, Kortuem KU, Chopra R, Faes L, et al. One- and two-year visual outcomes from the Moorfields age-related macular degeneration database: a retrospective cohort study and an open science resource. BMJ Open. 2019;9:e027441.
Spaide RF, Jaffe GJ, Sarraf D, Freund KB, Sadda SR, Staurenghi G, et al. Consensus nomenclature for reporting neovascular age-related macular degeneration data: consensus on neovascular age-related macular degeneration nomenclature study group. Ophthalmology. 2020;127:616–36.
Funding
The investigator-initiated study was funded by Boehringer Ingelheim International GmbH (Grant number: SIVS1045). This study was also supported by the NIHR Biomedical Research Centre and Clinical Research Facility at the Moorfields Eye Hospital National Health Service Foundation Trust and the University College London Institute of Ophthalmology. Role of the Funder/Sponsor: Boehringer Ingelheim was involved in the review and approval of the manuscript. Sobha Sivaprasad reported receiving financial support from AbbVie, Alimera Science, Amgen, Apellis, Astellas, Bayer, Biogen, Boehringer Ingelheim, Clearside Biomedical, Eyebiotech, Eyepoint Phamaceuticals, Iveric Bio, Janssen Pharmaceuticals, Nova Nordisk, Optos, Ocular Therapeutix, Kriya Therapeutics, OcuTerra, Ripple Therapeutics, Roche, Stealth Biotherapeutics and Sanofi. Sobha Sivaprasad is the Editor-in- Chief of EYE. Faruque Ghanchi has received honorarium for consultancy-advisory boards from Alimera, Allergan, Bayer, Novartis, Oxford BioElectronics, Roche; educational travel grants from Allergan, Bayer, Novartis; James Talks is a consultant for Bayer and Novartis, received grant support from Bayer, Novartis and Heidelberg Engineering, is involved in research for Allergan, Roche, Bayer, Novartis and Boehringer-Ingelheim, and is the Editor in Chief of Eye; Ian Pearce has received lecture fees from Allergan, Bayer, Heidelberg and Novartis, consultancy fees from Allergan, Alimera, Bayer and Novartis and travel fees from Allergan, Bayer and Novartis; Martin McKibbin has received lecture and advisory board honoraria from Bayer and Novartis and an educational travel grant from Bayer; Ajay Kotagiri received travel support from Novartis, Bayer, and Allergan, and speaker fees from Allergan and Bayer; Geeta Menon has conducted consultancy-advisory boards for Novartis, Bayer and Allergan, received educational travel grants from Novartis, Bayer, Allergan; Benjamin Burton is in the advisory board and received international conference attendance sponsored by Novartis and Bayer; Richard Gale has conducted consultancy-advisory boards for Novartis, Bayer and Allergan, Alimera, Santen, received educational travel grants from Novartis, Bayer, Allergan, Heidelberg Engineering.
Author information
Authors and Affiliations
Contributions
Conceptualization: SS; Data curation: AK, ST, RMP, SC, SG; Formal analysis: SG and SS; Funding acquisition: SS; Methodology: SC, SG, AK, ST and SS Project administration: SS; Resources: GM, BJB, IP, MM, ST, SC, RPM, AK, AKo, JT, FG, RG, AG, and SS; Supervision: SS; Visualization: SG and SC; Writing—original draft: SC, SG and SS; Writing—review & editing: SC, SG, SS. Review and approval of final manuscript: SC, SG, AK, SS, GM, BJB, IP, MM, ST, RPM, AKo, JT, AG, FG, RG.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chandak, S., Gurudas, S., Pakeer Muhammed, R. et al. Visual outcome following initiation of first injection versus after three monthly doses of aflibercept 2 mg for treatment naïve age-related macular degeneration to inform clinical trial designs: PRECISE Report No. 6. Eye 39, 2194–2203 (2025). https://doi.org/10.1038/s41433-025-03797-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-03797-z