Abstract
Background
The early detection of conjunctival fornix shortening is essential for the effective management of progressive cicatrising conjunctival diseases. Establishing a baseline reference for conjunctival scarring by determining the normative conjunctival fornix depths (FDs) allows for the measurement and monitoring of changes in the conjunctiva. This study explored anatomical variations in conjunctival FDs amongst an Asian Chinese population, providing valuable information for conjunctival fibrosis assessment.
Methods
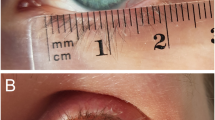
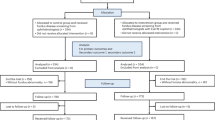
This retrospective study conducted at a single centre included 295 Chinese individuals (590 eyes) with normal conjunctiva who visited the eye clinic between 2019 and 2023. The lower and upper FDs were assessed using a validated FD measurer (FDM). Mean lower and upper FDs were calculated and stratified by age and gender.
Results
The mean upper and lower conjunctival FDs for the Chinese population in Singapore were 16.1 mm ± 1.6 (95% CI, 15.9–16.2) and 10.1 mm ± 1.7 (95% CI, 10.0–10.3), respectively. Females exhibited shorter FDs (upper 15.7 mm ± 1.5; lower 9.8 mm ± 1.5) compared to males (upper 16.5 mm ± 1.5; lower 10.5 mm ± 1.9) (p < 0.001). Linear regression analysis demonstrated a significant inverse correlation between age and FDs, indicating that FDs decreases with advancing age (R² = 0.1469 for upper and 0.3195 for lower fornices; p < 0.001). Specifically, the mean upper FD ranged from 17.4 mm (95% CI, 17.2–17.7) in the 20–29 age group to 15.2 mm (95% CI, 14.9–15.5) in the 80-89 age group. Similarly, the mean lower FD ranged from 12.0 mm (95% CI, 11.6–12.4) in the 20-29 age group to 8.7 mm (95% CI, 8.5–9.0) in the 80-89 age group. Analysis of the 95% CIs revealed no statistical difference in FD measurements when compared to published Caucasians, South Asians, and Turkish populations.
Conclusions
This study adds to the available literature a set of normative data for upper and lower FD in a Chinese population, highlighting gender-related variations and age-related progressive conjunctival shrinkage. The established dataset serves as a valuable resource for clinicians, enabling them to better manage and monitor patients with conjunctival diseases. These normative values in forniceal depths adds to available data obtained from Caucasian, South Asian, and Turkish eyes. Existing clinical assessment tools incorporating FD measurements, but validated in other ethnic populations, can be used in Chinese populations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request. These data are not publicly available due to ethical restrictions and the potential risk of compromising participant confidentiality. All relevant summary data have been presented within the manuscript and supplementary materials, in accordance with Eye’s Data Policy Type 3.
References
Dart JK. The 2016 Bowman Lecture Conjunctival curses: scarring conjunctivitis 30 years on. Eye. 2017;31:301–32.
Foster CS. Cicatricial pemphigoid. Trans Am Ophthalmol Soc. 1986;84:527–663.
Vazirani J, Donthineni PR, Goel S, Sane SS, Mahuvakar S, Narang P, et al. Chronic cicatrizing conjunctivitis: A review of the differential diagnosis and an algorithmic approach to management. Indian J Ophthalmol. 2020;68:2349–55.
Chang JH, McCluskey PJ. Ocular cicatricial pemphigoid: manifestations and management. Curr Allergy Asthma Rep. 2005;5:333–8.
Hossain P. The evil curse of ocular pemphigoid. Eye. 2011;25:1107–8.
Kohanim S, Palioura S, Saeed HN, Akpek EK, Amescua G, Basu S, et al. Acute and chronic ophthalmic involvement in Stevens-Johnson Syndrome/Toxic epidermal necrolysis - a comprehensive review and guide to Therapy. II. Ophthalmic disease. Ocul Surf. 2016;14:168–88.
Williams GP, Radford C, Nightingale P, Dart JK, Rauz S. Evaluation of early and late presentation of patients with ocular mucous membrane pemphigoid to two major tertiary referral hospitals in the United Kingdom. Eye. 2011;25:1207–18.
Radford CF, Rauz S, Williams GP, Saw VP, Dart JK. Incidence, presenting features, and diagnosis of cicatrising conjunctivitis in the United Kingdom. Eye. 2012;26:1199–208.
Chan LS, Ahmed AR, Anhalt GJ, Bernauer W, Cooper KD, Elder MJ, et al. The first international consensus on mucous membrane pemphigoid: definition, diagnostic criteria, pathogenic factors, medical treatment, and prognostic indicators. Arch Dermatol. 2002;138:370–9.
Saw VP, Dart JK. Ocular mucous membrane pemphigoid: diagnosis and management strategies. Ocul Surf. 2008;6:128–42.
Zillikens D, Wever S, Roth A, Weidenthaler-Barth B, Hashimoto T, Brocker EB. Incidence of autoimmune subepidermal blistering dermatoses in a region of central Germany. Arch Dermatol. 1995;131:957–8.
Bobba S, Devlin C, Di Girolamo N, Wakefield D, McCluskey P, Chan E, et al. Incidence, clinical features and diagnosis of cicatrising conjunctivitis in Australia and New Zealand. Eye. 2018;32:1636–43.
Vazirani J, Nair D, Shanbhag S, Wurity S, Ranjan A, Sangwan V. Limbal stem cell deficiency-demography and underlying causes. Am J Ophthalmol. 2018;188:99–103.
Singh S, Donthineni PR, Shanbhag SS, Senthil S, Ong HS, Dart JK, et al. Drug induced cicatrizing conjunctivitis: A case series with review of etiopathogenesis, diagnosis and management. Ocul Surf. 2022;24:83–92.
Solomon AW, Burton MJ, Gower EW, Harding-Esch EM, Oldenburg CE, Taylor HR, et al. Trachoma. Nat Rev Dis Primers. 2022;8:32.
Kasi PM, Gilani AI, Ahmad K, Janjua NZ. Blinding trachoma: a disease of poverty. PLoS Med. 2004;1:e44.
Ong HS, Dart JK. Managing ocular surface disease: a common-sense approach. Community Eye Health. 2016;29:44–6.
Saw VP, Dart JK, Rauz S, Ramsay A, Bunce C, Xing W, et al. Immunosuppressive therapy for ocular mucous membrane pemphigoid strategies and outcomes. Ophthalmology. 2008;115:253–61.e1.
Saw VP, Offiah I, Dart RJ, Galatowicz G, Dart JK, Daniels JT, et al. Conjunctival interleukin-13 expression in mucous membrane pemphigoid and functional effects of interleukin-13 on conjunctival fibroblasts in vitro. Am J Pathol. 2009;175:2406–15.
Mondino BJ, Brown SI. Ocular cicatricial pemphigoid. Ophthalmology. 1981;88:95–100.
Tauber J, Jabbur N, Foster CS. Improved detection of disease progression in ocular cicatricial pemphigoid. Cornea. 1992;11:446–51.
Schwab IR, Linberg JV, Gioia VM, Benson WH, Chao GM. Foreshortening of the inferior conjunctival fornix associated with chronic glaucoma medications. Ophthalmology. 1992;99:197–202.
Jutley G, Carpenter D, Hau S, Booth D, Jasim HA, Tay E, et al. Upper and lower conjunctival fornix depth in healthy white caucasian eyes: a method of objective assessment. Eye. 2016;30:1351–8.
Kawakita T, Kawashima M, Murat D, Tsubota K, Shimazaki J. Measurement of fornix depth and area: a novel method of determining the severity of fornix shortening. Eye. 2009;23:1115–9.
Khan IJ, Ghauri AJ, Hodson J, Edmunds MR, Cottrell P, Evans S, et al. Defining the limits of normal conjunctival fornix anatomy in a healthy South Asian population. Ophthalmology. 2014;121:492–7.
Bulut O, Kaplan A, Furundaoturan O, Kose T, Barut Selver O. Identification of Normal Fornix Depth Dataset Generated with a Validated Fornix Meter in Healthy Turkish Population. Ocul Immunol Inflamm. 2023:1–5.
Ong HS, Minassian D, Rauz S, Mehta JS, Dart JK. Validation of a clinical assessment tool for cicatrising conjunctivitis. Ocul Surf. 2020;18:121–9.
Hong M, Tong L, Mehta JS, Ong HS. Impact of Exposomes on Ocular Surface Diseases. Int J Mol Sci. 2023;24.
Ong HS, Dart JK, Mehta JS. A review of clinical disease scoring systems for cicatricial diseases of the conjunctiva. Front Med. 2021;8:664572.
McCabe MC, Hill RC, Calderone K, Cui Y, Yan Y, Quan T, et al. Alterations in extracellular matrix composition during aging and photoaging of the skin. Matrix Biol Plus. 2020;8:100041.
Phan H, Chotprasert N, Janebodin K, Charoonpatrapong K, Srithavaj T. OSC20: Factors affecting dimensions of the 3D Ocular prosthesis in patients rehabilitated at Mahidol University. J Indian Prosthodont Soc. 2018;18:S15.
Williams GP, Saw VP, Saeed T, Evans ST, Cottrell P, Curnow SJ, et al. Validation of a fornix depth measurer: a putative tool for the assessment of progressive cicatrising conjunctivitis. Br J Ophthalmol. 2011;95:842–7.
Acknowledgements
We would like to extend sincere gratitude to Professor John Dart for his invaluable time, expertise, and constructive feedback on this study.
Funding
This work was supported by the following grants held by Hon Shing Ong: SingHealth Foundation Grant, Singapore (Ref: SHF/FG707S/2017), SingHealth Duke-NUS Ophthalmology & Visual Sciences Academic Clinical Programme Award (Ref: 05/FY2019/P1/18-A33), and the National Medical Research Council (NMRC) Transition Award (Ref: MOH-001776). None of the funders had any role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
Conceptualisation and supervision: HSO, SR, JKD, JSM. Data curation: HSO, MD. Formal analysis, investigation & methodology: STT, HSO, JKD. Funding acquisition: HSO, JSM. Writing draft, review & editing: HSO, STT, SR, JKD, JSM. All authors approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
Saaeha Rauz is a member of the Eye editorial board. The authors declare that they have no competing interests related to the content of this manuscript. All authors have disclosed any potential conflicts of interest and have adhered to ethical guidelines to ensure the integrity of the research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tan, S.T., Htoon, H.M., Davidson, M. et al. Defining the limits of upper and lower conjunctival fornix depths in a healthy Asian Chinese population. Eye 39, 2289–2297 (2025). https://doi.org/10.1038/s41433-025-03828-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-03828-9