Abstract
Objective
We aimed to use symptom-based stratification to identify the subtype-specific pathophysiology of dry eye disease (DED) in Sjögren’s syndrome (SS).
Methods
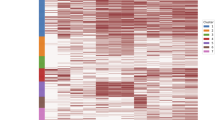
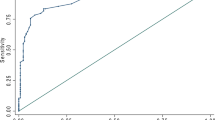
We retrospectively enrolled patients with SS who visited Juntendo University Hospital between October 2017 and July 2023 and were diagnosed with DED (2016 Asia Dry Eye Society guideline). The DED subtype and pathophysiology were classified under five distinct tear film breakup patterns: area, line, spot, dimple, and random breaks. Based on responses to the Japanese version of the Ocular Surface Disease Index (J-OSDI), spectral clustering was used to stratify participants; inter-cluster comparison of J-OSDI total scores and key DED-related objective findings was undertaken.
Results
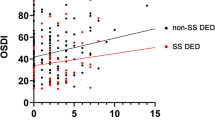
Among the 239 participants, DED prevalence was the highest in Cluster 3 (98.2%), followed by clusters 2 (83.4%) and 1 (4.1%). J-OSDI total scores were the highest in Cluster 3 (64.6 points) and lowest in Cluster 1 (2.1 points) (P < 0.001). Prevalence of line and area breaks (aqueous-deficient type) was highest in Cluster 1 (81.6%) whereas dimple and spot breaks (decreased-wettability type) were most prevalent in Cluster 2 (21.0%). Random breaks (increased evaporation) were observed most frequently in Cluster 1 (8.2%). Median MBI was shortest in Cluster 3 (7.1 s), followed by Cluster 2 (8.6 s) (P = 0.003). The median serum anti-SS-A/Ro concentration was highest in Cluster 3 (32.0 U/mL; P = 0.018). Cluster 2 showed a notable discrepancy between subjective symptoms and CFS scores.
Conclusions
Using symptom-based DED severity of SS, we successfully stratified patients into three clusters to potentially facilitate type-customised interventions to improve treatment efficacy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
All relevant data are included within the manuscript and its supplementary materials.
References
Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo CK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15:276–83.
Tsubota K, Yokoi N, Shimazaki J, Watanabe H, Dogru M, Yamada M, et al. New perspectives on dry eye definition and diagnosis: a consensus report by the Asia dry eye society. Ocul Surf. 2017;15:65–76.
Stapleton F, Alves M, Bunya VY, Jalbert I, Lekhanont K, Malet F, et al. TFOS DEWS II epidemiology report. Ocul Surf. 2017;15:334–65.
Inomata T, Nakamura M, Iwagami M, Shiang T, Yoshimura Y, Fujimoto K, et al. risk factors for severe dry eye disease: crowdsourced research using DryEyeRhythm. Ophthalmology. 2019;126:766–8.
Belmonte C, Nichols JJ, Cox SM, Brock JA, Begley CG, Bereiter DA, et al. TFOS DEWS II pain and sensation report. Ocul Surf. 2017;15:404–37.
Yamada M, Mizuno Y, Shigeyasu C. Impact of dry eye on work productivity. Clinicoecon Outcomes Res. 2012;4:307–12.
Negrini S, Emmi G, Greco M, Borro M, Sardanelli F, Murdaca G, et al. Sjögren’s syndrome: a systemic autoimmune disease. Clin Exp Med. 2022;22:9–25.
Carsons SE, Patel BC. Sjogren Syndrome. StatPearls. StatPearls Publishing Copyright © 2025, StatPearls Publishing LLC.: Treasure Island (FL) ineligible companies. Disclosure: Bhupendra Patel declares no relevant financial relationships with ineligible companies.; 2025. https://pubmed.ncbi.nlm.nih.gov/28613703/.
Lessard CJ, Li H, Adrianto I, Ice JA, Rasmussen A, Grundahl KM, et al. Variants at multiple loci implicated in both innate and adaptive immune responses are associated with Sjögren’s syndrome. Nat Genet. 2013;45:1284–92.
Bezzina OM, Gallagher P, Mitchell S, Bowman SJ, Griffiths B, Hindmarsh V, et al. Subjective and objective measures of dryness symptoms in primary Sjögren’s syndrome: capturing the discrepancy. Arthritis Care Res. 2017;69:1714–23.
Adatia FA, Michaeli-Cohen A, Naor J, Caffery B, Bookman A, Slomovic A. Correlation between corneal sensitivity, subjective dry eye symptoms and corneal staining in Sjögren’s syndrome. Can J Ophthalmol. 2004;39:767–71.
Tarn JR, Howard-Tripp N, Lendrem DW, Mariette X, Saraux A, Devauchelle-Pensec V, et al. Symptom-based stratification of patients with primary Sjögren’s syndrome: multi-dimensional characterisation of international observational cohorts and reanalyses of randomised clinical trials. Lancet Rheumatol. 2019;1:e85–94.
Inomata T, Iwagami M, Hiratsuka Y, Fujimoto K, Okumura Y, Shiang T, et al. Maximum blink interval is associated with tear film breakup time: a new simple, screening test for dry eye disease. Sci Rep. 2018;8:13443.
Fujibayashi T, Sugai S, Miyasaka N, Hayashi Y, Tsubota K. Revised Japanese criteria for Sjögren’s syndrome (1999): availability and validity. Mod Rheumatol. 2004;14:425–34.
Midorikawa-Inomata A, Inomata T, Nojiri S, Nakamura M, Iwagami M, Fujimoto K, et al. Reliability and validity of the Japanese version of the ocular surface disease Index for dry eye disease. BMJ Open. 2019;9:e033940.
Yokoi N, Georgiev GA, Kato H, Komuro A, Sonomura Y, Sotozono C, et al. Classification of fluorescein breakup patterns: a novel method of differential diagnosis for dry eye. Am J Ophthalmol. 2017;180:72–85.
Yokoi N, Georgiev GA. Tear-film-oriented diagnosis for dry eye. Jpn J Ophthalmol. 2019;63:127–36.
van Bijsterveld OP. Diagnostic tests in the Sicca syndrome. Arch Ophthalmol. 1969;82:10–14.
Senchyna M, Wax MB. Quantitative assessment of tear production: a review of methods and utility in dry eye drug discovery. J Ocul Biol Dis Info. 2008;1:1–6.
Suzuki Y, Fujii H, Nomura H, Mizushima I, Yamada K, Yamagishi M, et al. Impact of double positive for anti-centromere and anti-SS-a/Ro antibodies on clinicopathological characteristics of primary Sjögren’s syndrome: a retrospective cohort study. Mod Rheumatol. 2018;28:872–8.
Praprotnik S, Bozic B, Kveder T, Rozman B. Fluctuation of anti-Ro/SS-A antibody levels in patients with systemic lupus erythematosus and Sjögren’s syndrome: a prospective study. Clin Exp Rheumatol. 1999;17:63–68.
Inomata T, Nakamura M, Sung J, Midorikawa-Inomata A, Iwagami M, Fujio K, et al. Smartphone-based digital phenotyping for dry eye toward P4 medicine: a crowdsourced cross-sectional study. NPJ Digit Med. 2021;4:171.
von Luxburg U. A tutorial on spectral clustering. Statistics Comput. 2007;17:395–416.
McInnes L, Healy J. UMAP: Uniform Manifold Approximation and Projection for Dimension Reduction. ArXiv; https://doi.org/10.48550/arXiv.1802.03426 (2018).
Ogawa Y. Sjögren’s Syndrome, Non-Sjögren’s Syndrome, and Graft-Versus-Host Disease Related Dry Eye. Invest Ophthalmol Vis Sci. 2018;59:Des71–des79.
Foulks GN, Forstot SL, Donshik PC, Forstot JZ, Goldstein MH, Lemp MA, et al. Clinical guidelines for management of dry eye associated with Sjögren disease. Ocul Surf. 2015;13:118–32.
Pflugfelder SC, Jones D, Ji Z, Afonso A, Monroy D. Altered cytokine balance in the tear fluid and conjunctiva of patients with Sjögren’s syndrome keratoconjunctivitis sicca. Curr Eye Res. 1999;19:201–11.
Han SB, Hyon JY, Wee WR, Lee JH, Lee YJ, Yun PY. Reduced corneal sensitivity in patients with primary Sjögren’s syndrome. Acta Ophthalmol. 2010;88:e277–8.
Akpek EK, Bunya VY, Saldanha IJ. Sjögren’s syndrome: more than just dry eye. Cornea. 2019;38:658–61.
Parisis D, Chivasso C, Perret J, Soyfoo MS, Delporte C. Current state of knowledge on primary Sjögren’s syndrome, an autoimmune exocrinopathy. J Clin Med. 2020;9:2299.
Argüeso P, Balaram M, Spurr-Michaud S, Keutmann HT, Dana MR, Gipson IK. Decreased levels of the goblet cell mucin MUC5AC in tears of patients with Sjögren syndrome. Investig Ophthalmol Vis Sci. 2002;43:1004–11.
Chaudhury NM, Proctor GB, Karlsson NG, Carpenter GH, Flowers SA. Reduced Mucin-7 (Muc7) Sialylation and altered saliva rheology in Sjögren’s syndrome associated oral dryness. Mol Cell Proteom. 2016;15:1048–59.
Tsubota K, Yokoi N, Watanabe H, Dogru M, Kojima T, Yamada M, et al. A new perspective on dry eye classification: proposal by the Asia dry eye society. Eye Contact Lens. 2020;46:S2–13.
Mavragani CP, Moutsopoulos HM. The geoepidemiology of Sjögren’s syndrome. Autoimmun Rev. 2010;9:A305–310.
Tsubota K, Pflugfelder SC, Liu Z, Baudouin C, Kim HM, Messmer EM, et al. Defining dry eye from a clinical perspective. Int J Mol Sci. 2020;21:9271.
Labbé A, Wang YX, Jie Y, Baudouin C, Jonas JB, Xu L. Dry eye disease, dry eye symptoms and depression: the Beijing Eye Study. Br J Ophthalmol. 2013;97:1399–403.
Acknowledgements
The authors thank Professor Shigeki Aoki, Head of the Data Science, at Juntendo University Graduate School of Medicine, for fostering a supportive and collaborative research environment, and thank the nurses and orthoptists, of the Department of Ophthalmology, at Juntendo University Faculty of Medicine, for data collection and measurements undertaken for the DED diagnosis.
Funding
This research was funded by the Japan Agency for Medical Research and Development (24hma322004s0803 [TI]), JST FOREST program (JPMJFR234I [TI]), Japan Society for the Promotion of Science, Grants-in-Aid for Scientific Research (grant numbers: 23K16364 [AMI], 23K18406 [TI], 24K19796 [AE], 25K20553 [KN], and 25K12857 [TI]), and OTC Self-Medication Promotion Foundation 2019, 2021, and 2024 (TI), Research Grants in the Natural Sciences 2024, The Mitsubishi Foundation (TI), and Suzuken Memorial Foundation 2024 (TI). The funding sources had no role in the study design, data collection, analysis, interpretation, writing of the report, or decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
MT was responsible for methodology, data curation, visualisation, formal analysis, investigation, writing-original draft preparation, and writing- reviewing and editing. KN was responsible for methodology, data curation, validation, visualisation, formal analysis, investigation, writing-original draft preparation, and writing- reviewing and editing. JS conducted the investigation and wrote the original draft and reviewed and edited the manuscript. AMI performed validation, investigation, funding, writing-original draft preparation, and writing- reviewing and editing. AE performed validation, funding, writing-original draft preparation, and writing- reviewing and editing. TH performed data curation, writing-original draft preparation, and writing- reviewing and editing. SN performed supervision, writing-original draft preparation, and writing- reviewing and editing. TI was responsible for conceptualisation, methodology, data curation, validation, visualisation, formal analysis, investigation, funding, writing-original draft preparation, and writing- reviewing and editing.
Corresponding author
Ethics declarations
Competing interests
KN and AMI received personal fees from InnoJin, Inc., outside of the submitted work. SN reports grants from Kowa Company. Ltd., Mitsubishi Tanabe Pharma Corporation, Alcon Japan, Ltd., Santen Pharmaceutical Co., Ltd., Machida Endoscope Co., Ltd., Wakamoto Pharmaceutical Co., Ltd., Bayer Yakuhin, Ltd., Senju Pharmaceutical Co., Ltd., Nippon Boehringer Ingelheim Co., Ltd., Chugai Pharmaceutical Co., Ltd., Hoya Corporation, and Novartis Pharma KK, outside the submitted work. TI reports non-financial support from Lion Corporation and Sony Network Communications Inc., grants from Johnson & Johnson Vision Care, Inc., Yuimedi, Inc., ROHTO Pharmaceutical Co., Ltd., Kobayashi Pharmaceutical Co., Ltd., Kandenko Co., Ltd., and Fukoku Co., Ltd., personal fees from Santen Pharmaceutical Co., Ltd., InnoJin, Inc., and Ono Pharmaceutical Co., Ltd., outside the submitted work. The remaining authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tamagawa, M., Nagino, K., Sung, J. et al. Symptom-based stratification of heterogeneous symptoms of dry eye disease in patients with Sjögren’s syndrome. Eye 39, 2415–2422 (2025). https://doi.org/10.1038/s41433-025-03880-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-03880-5