Abstract
Background/Objectives
Retinopathy of prematurity (ROP) is a leading cause of childhood blindness. This systematic review and meta-analysis assess the association between eight serum biomarkers and the presence of ROP in premature neonates. These biomarkers are neutrophil-to-lymphocyte ratio (NLR), C-reactive protein (CRP), red cell distribution width (RDW), lymphocyte-to-monocyte ratio (LMR), platelet-to-lymphocyte ratio (PLR), platelet mass index (PMI), systemic immune-inflammation index (SII), and vitamin D.
Subjects/Methods
A comprehensive literature search was conducted across PubMed, Embase, Scopus, and Cochrane Library for studies published up to February 2025. Eligible studies included quantitative data on serum biomarker levels in premature neonates with and without ROP. A random-effects meta-analysis estimated standardised mean differences (SMDs) and 95% confidence intervals (CIs). Risk of bias was assessed using the Newcastle-Ottawa Scale.
Results
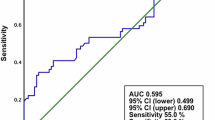
Twenty-one studies comprising 3965 participants were included. Significant associations were found for NLR (SMD = 0.43, 95% CI: 0.16–0.71, P = 0.002), RDW (SMD = 0.41, 95% CI: 0.15–0.67, P = 0.002), and vitamin D (SMD = −1.18, 95% CI: -1.47–-0.90, P < 0.00001). CRP, LMR, PLR, PMI, and SII did not show significant associations with ROP presence.
Conclusions
NLR, RDW, and vitamin D levels are potential biomarkers associated with ROP presence in premature neonates, likely reflecting systemic inflammation and vascular pathology. Further large-scale prospective studies are warranted to establish standardised cutoff values for clinical implementation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
References
Good WV, Hardy RJ, Dobson V, Palmer EA, Phelps DL, Quintos M, et al. The incidence and course of retinopathy of prematurity: findings from the early treatment for retinopathy of prematurity study. Pediatrics. 2005;116:15–23.
Solebo AL, Teoh L, Rahi J. Epidemiology of blindness in children. Arch Dis Child. 2017;102:853–7.
Blencowe H, Lawn JE, Vazquez T, Fielder A, Gilbert C. Preterm-associated visual impairment and estimates of retinopathy of prematurity at regional and global levels for 2010. Pediatr Res. 2013;74:35–49.
Hartnett ME, Penn JS. Mechanisms and management of retinopathy of prematurity. N Engl J Med. 2012;367:2515–26.
Ramshekar A, Hartnett ME. Vascular endothelial growth factor signaling in models of oxygen-induced retinopathy: insights into mechanisms of pathology in retinopathy of prematurity. Front Pediatr. 2021;9:796143.
Poets CF, Roberts RS, Schmidt B, Whyte RK, Asztalos EV, Bader D, et al. Association between intermittent Hypoxemia or Bradycardia and late death or disability in extremely preterm infants. Jama. 2015;314:595–603.
Darlow BA, Hutchinson JL, Henderson-Smart DJ, Donoghue DA, Simpson JM, Evans NJ. Prenatal risk factors for severe retinopathy of prematurity among very preterm infants of the Australian and New Zealand Neonatal Network. Pediatrics. 2005;115:990–6.
Sabri K, Ells AL, Lee EY, Dutta S, Vinekar A. Retinopathy of Prematurity: A Global Perspective and Recent Developments. Pediatrics. 2022;150.
Chuang SH, Chang CH. Platelet-to-lymphocyte ratio and lymphocyte-to-monocyte ratio in glaucoma: a meta-analysis. Biomark Med. 2024;18:39–49.
Shirvani M, Soufi F, Nouralishahi A, Vakili K, Salimi A, Lucke-Wold B, et al. The diagnostic value of neutrophil to lymphocyte ratio as an effective biomarker for eye disorders: a meta-analysis. Biomed Res Int. 2022;2022:5744008.
Song J, Chen S, Liu X, Duan H, Kong J, Li Z. Relationship between C-reactive protein level and diabetic retinopathy: a systematic review and meta-analysis. PLoS One. 2015;10:e0144406.
Mu Y, Wang H. Association of neutrophil to lymphocyte ratio with preterm necrotizing enterocolitis: a retrospective case-control study. BMC Gastroenterol. 2022;22:248.
Akdogan M, Ustundag Y, Cevik SG, Dogan P, Dogan N. Correlation between systemic immune-inflammation index and routine hemogram-related inflammatory markers in the prognosis of retinopathy of prematurity. Indian J Ophthalmol. 2021;69:2182–7.
Bakry HESK, Shahin EMT, Mohamed SA, Eldmery AM, Elgazzar AMF, Elkhrsawy AM, et al. Retinopathy of prematurity and the changes of the red cells distribution width in neonates: a retrospective study. NeuroQuantology. 2022;20:753–60.
Borțea CI, Stoica F, Boia M, Iacob ER, Dinu M, Iacob R, et al. Risk factors associated with retinopathy of prematurity in very and extremely preterm infants. Medicina. 2021;57.
Boskabadi H, Abrishami M, Shoeibi N, Sanei Z, Moradi A, Zakerihamidi M. Comparison of Vitamin D levels in premature infants with and without retinopathy of prematurity. Arch Iran Med. 2022;25:209–13.
Celik K, Ekinci D, Asena M, Matur NO. Can hematological parameters be a indicator risk factor in the development of retinopathy of prematurity?. Klin Padiatr. 2021;233:216–20.
Çömez A, Yurttutan S, Seringec Akkececi N, Bozkaya A, Köküsarı G, Evgin İ, et al. Red cell distribution width and its association with retinopathy of prematurity. Int Ophthalmol. 2021;41:699–706.
Deger I, Ertuğrul S, Kaya IK, Yılmaz ST, Yolbaş I. Can platelet count, Platelet Mass Index and mean platelet volume be parameters in retinopathy of prematurity?. East J Med. 2022;27:513–8.
Ekinci DY, Bezirganoglu H, Okur N, Tas M. A novel marker for predicting type 1 retinopathy of prematurity: C-reactive protein/albumin ratio. Int Ophthalmol. 2023;43:3345–53.
Fevereiro-Martins M, Santos AC, Marques-Neves C, Guimarães H, Bicho M. Complete blood count parameters as biomarkers of retinopathy of prematurity: a Portuguese multicenter study. Graefes Arch Clin Exp Ophthalmol. 2023;261:2997–3006.
Hu YX, Xu XX, Shao Y, Yuan GL, Mei F, Zhou Q, et al. The prognostic value of lymphocyte-to-monocyte ratio in retinopathy of prematurity. Int J Ophthalmol. 2017;10:1716–21.
Kabataş EU, Dinlen NF, Zenciroğlu A, Dilli D, Beken S, Okumuş N. Relationship between serum 25-hydroxy vitamin D levels and retinopathy of prematurity. Scott Med J. 2017;62:129–35.
Kıran Yenice E, Kara C, Karsli Türkoglu T, Ulubaş Işık D, Çelik İH. Predictive value of serum inflammatory markers in retinopathy of prematurity. Eye. 2024;38:2822–6.
Kurtul BE, Kabatas EU, Zenciroglu A, Ozer PA, Ertugrul GT, Beken S, et al. Serum neutrophil-to-lymphocyte ratio in retinopathy of prematurity. J AAPOS. 2015;19:327–31.
Maeda H, Go H, Iwasa H, Hiruta S, Ichikawa H, Sugano Y, et al. Red blood cell parameters as biomarkers of retinopathy of prematurity in preterm infants born before 30 weeks of gestation. Sci Rep. 2025;15:264.
Modrzejewska M, Bosy-Gąsior W, Grzesiak W Association of Positive Bacterial Cultures Obtained from the Throat, Anus, Ear, Bronchi and Blood in Very-Low-Birth-Weight Premature Infants with Severe Retinopathy of Prematurity—Own Observations. J Clin Med. 2023;12.
Obata S, Matsumoto R, Kakinoki M, Sawada O, Sawada T, Saishin Y, et al. Blood neutrophil-to-lymphocyte ratio as a risk factor in treatment for retinopathy of prematurity. Graefes Arch Clin Exp Ophthalmol. 2023;261:951–7.
Okur N, Buyuktiryaki M, Uras N, Oncel MY, Ertekin O, Canpolat FE, et al. Platelet mass index in very preterm infants: can it be used as a parameter for neonatal morbidities?. J Matern Fetal Neonatal Med. 2016;29:3218–22.
Oruz O, Dervişoğulları MS, Öktem ME, İncekaş C. Predictive role of systemic immune-inflammation index and neutrophil/lymphocyte ratio values in infants with retinopathy of prematurity. Graefes Arch Clin Exp Ophthalmol. 2024;262:3125–34.
Ozturk T, Durmaz Engin C, Kaya M, Yaman A. Complete blood count parameters to predict retinopathy of prematurity: when to evaluate and what do they tell us?. Int Ophthalmol. 2021;41:2009–18.
Ugurlu A, Icel E. Are the neutrophil-to-lymphocyte, platelet-to-lymphocyte and monocyte-to-lymphocyte ratios predictive factors for the retinopathy of prematurity?. Hong Kong J Paediatr. 2022;27:107–12.
Zonda GI, Mogos R, Melinte-Popescu AS, Adam AM, Harabor V, Nemescu D, et al. Hematologic Risk Factors for the Development of Retinopathy of Prematurity—A Retrospective Study. Children. 2023;10.
Ikeda H, Kuriyama S. Risk factors for retinopathy of prematurity requiring photocoagulation. Jpn J Ophthalmol. 2004;48:68–71.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle–Ottawa Scale (NOS) for Assessing the Quality of Non-Randomized Studies in Meta-Analysis. 2000.
Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. 2018;27:1785–805.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135.
Altman D, Machin D, Bryant T, Gardner M eds 2000: Statistics with confidence, 2nd edn. London: BMJ Books. 240 pp+ diskette,£ 19.95 (PB). Citeseer; 2001.
Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1:97–111.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–63.
Chiang MF, Quinn GE, Fielder AR, Ostmo SR, Paul Chan RV, Berrocal A, et al. International Classification of Retinopathy of Prematurity, Third Edition. Ophthalmology. 2021;128:e51–e68.
Hellstrom A, Smith LE, Dammann O. Retinopathy of prematurity. Lancet. 2013;382:1445–57.
Hellgren G, Lundgren P, Pivodic A, Lofqvist C, Nilsson AK, Ley D, et al. Decreased platelet counts and serum levels of VEGF-A, PDGF-BB, and BDNF in extremely preterm infants developing severe ROP. Neonatology. 2021;118:18–27.
Sood BG, Madan A, Saha S, Schendel D, Thorsen P, Skogstrand K, et al. Perinatal systemic inflammatory response syndrome and retinopathy of prematurity. Pediatr Res. 2010;67:394–400.
Woo SJ, Park KH, Lee SY, Ahn SJ, Ahn J, Park KH, et al. The relationship between cord blood cytokine levels and perinatal factors and retinopathy of prematurity: a gestational age-matched case-control study. Invest Ophthalmol Vis Sci. 2013;54:3434–9.
Tremblay S, Miloudi K, Chaychi S, Favret S, Binet F, Polosa A, et al. Systemic inflammation perturbs developmental retinal angiogenesis and neuroretinal function. Invest Ophthalmol Vis Sci. 2013;54:8125–39.
Ozgonul C, Sertoglu E, Gokce G. Accurate use of neutrophil/lymphocyte ratio in patients with keratoconus. Cornea. 2015;34:e4–5.
Howard R, Kanetsky PA, Egan KM. Exploring the prognostic value of the neutrophil-to-lymphocyte ratio in cancer. Sci Rep. 2019;9:19673.
Orkin SH, David EF, Nathan DG, Look, AT, Lux SE & Ginsburg D. Nathan and Oski’s hematology of infancy and childhood. 6th, editor: 2003 pp. 2752.
Yektaei-Karin E, Moshfegh A, Lundahl J, Berggren V, Hansson LO, Marchini G. The stress of birth enhances in vitro spontaneous and IL-8-induced neutrophil chemotaxis in the human newborn. Pediatr Allergy Immunol. 2007;18:643–51.
Acknowledgements
None.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Conceptualisation: Shu-Han Chuang, Yen Thi Thao Le, Cheng-Hsien Chang. Data curation: Shu-Han Chuang, Yen Thi Thao Le, Yan-Han Li, Yu Zhi Lian. Formal analysis: Shu-Han Chuang, Yen Thi Thao Le, Yan-Han Li, Yu Zhi Lian. Investigation: Shu-Han Chuang, Yen Thi Thao Le, Yan-Han Li, Cheng-Hsien Chang. Methodology: Cheng-Hsien Chang, Yi-Jie Kuo, Yu-Pin Chen. Software: Yi-Jie Kuo, Yu-Pin Chen. Resources: Cheng-Hsien Chang, Yi-Jie Kuo, Yu-Pin Chen. Supervision: Cheng-Hsien Chang, Yi-Jie Kuo, Yu-Pin Chen. Validation: Shu-Han Chuang, Yen Thi Thao Le, Yan-Han Li, Yu Zhi Lian. Visualisation: Shu-Han Chuang, Yen Thi Thao Le, Yan-Han Li, Yu Zhi Lian. Writing – original draft: Shu-Han Chuang, Yen Thi Thao Le, Yan-Han Li, Yu Zhi Lian. Writing – review & editing: Cheng-Hsien Chang, Yi-Jie Kuo, Yu-Pin Chen.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
The Institutional Review Board Committee of Changhua Christian Hospital in Taiwan granted ethical approval for the execution of this study (IRB number: 240607).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chuang, SH., Le, Y.T.T., Li, YH. et al. Significance of serum biomarkers in preterm infants screened for retinopathy of prematurity: a systematic review and meta-analysis. Eye 39, 3167–3175 (2025). https://doi.org/10.1038/s41433-025-04051-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-04051-2