Abstract
Objectives
To report the clinical outcomes of surgical management versus medical management alone in cases of endogenous fungal endophthalmitis. Additionally, we explore the role of routine ophthalmic screening.
Methods
Retrospective observational multicentre study. We examined the databases of five UK centres and a tertiary centre in the United States for patients with Candida septicaemia (candidemia) and/or clinically established endogenous fungal endophthalmitis. Clinical data including visual acuity and other outcomes were reviewed and analysed with statistics.
Results
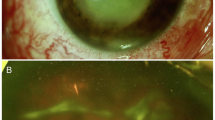
A total of 404 patients were included from all centres. Forty-six eyes were diagnosed clinically as presumed EFE - of which 25 were later confirmed with positive vitreous biopsies. 18/46 received systemic medical treatment with or without intravitreal injection of antifungal agents and without a significant logMAR vision improvement from 1.15 ± 0.29 at baseline to 0.74 ± 0.21 at last follow up. The remaining 28/46 eyes received both systemic medical treatment and vitrectomy, and visual acuity improved from 1.56 ± 0.19 to 1.14 ± 0.21 after surgery (p = 0.04). At the last follow up, 18/28 eyes (64.3%) had an attached retina with no tamponade, three attached under oil and two ending up with detached retina. Silicone oil was retained in three eyes due to either patient comorbidities precluding further surgery or due to surgeon preference to ensure long-term anatomical stability. Two cases resulted in macular and/or fibrovascular scarring and one in enucleation. Out of 359 patients with candidemia, 95 (26.4%) had ophthalmological examination and only 9 (9.47% of those examined and 2.5% of the total) had endogenous fungal endophthalmitis (7 confirmed with vitreous sample cultures and 2 presumed).
Conclusion
Although our findings suggest that vitrectomy may improve outcomes in select cases of EFE, the retrospective nature of our study and the potential for bias mandate cautious interpretation. Therefore, further prospective studies are necessary to shed more light with novel insights. A more targeted, case-by-case screening paradigm for patients with candidemia is advocated for optimum outcomes and efficient use of resources.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The raw data (excel sheet) that support the findings of this study are available upon request from the corresponding author (A.W.).
Change history
12 November 2025
In this article the acknowledgement section has been modified. The following sentence is added: The authors gratefully acknowledge Dr. Kashika Singh, BMBS, BMedSci (Hons), and Dr. Haytham Rezq, who were affiliated with University Hospital Southampton NHS Foundation Trust at the time of data collection, for their valuable contribution to the acquisition of data supporting this work. Dr. Singh is currently affiliated with Worcestershire Acute Hospitals Trust, and Dr. Rezq is currently affiliated with Magrabi Health Hospitals and Centres.
References
Lingappan A, Wykoff CC, Albini TA, Miller D, Pathengay A, Davis JL, et al. Endogenous fungal endophthalmitis: causative organisms, management strategies, and visual acuity outcomes. Am J Ophthalmol. 2012;153:162–6.
Schiedler V, Scott IU, Flynn Jr HW, Davis JL, Benz MS, Miller D. Culture-proven endogenous endophthalmitis: clinical features and visual acuity outcomes. Am J Ophthalmol. 2004;137:725–31.
Horn DL, Neofytos D, Anaissie EJ, Fishman JA, Steinbach WJ, Olyaei AJ, et al. Epidemiology and outcomes of candidemia in 2019 patients: data from the prospective antifungal therapy alliance registry. Clin Infect Dis. 2009;48:1695–703.
Menezes AV, Sigesmund DA, Demajo WA, Devenyi RG. Mortality of hospitalized patients with Candida endophthalmitis. Arch Intern Med. 1994;154:2093–7.
Breazzano MP, Tooley AA, Godfrey KJ, Iacob CE, Yannuzzi NA, Flynn HW. Candida auris and endogenous panophthalmitis: clinical and histopathological features. Am J Ophthalmol Case Rep. 2020;19. https://pubmed.ncbi.nlm.nih.gov/32462100/ [Accessed October 18, 2024].
Kostick DA. Endogenous endophthalmitis caused by Candida albicans in a healthy woman. Am J Ophthalmol. 1992;113:593–5.
Sridhar J, Flynn HW, Kuriyan AE, Miller D, Albini T. Endogenous fungal endophthalmitis: risk factors, clinical features, and treatment outcomes in mold and yeast infections. J Ophthalmic Inflamm Infect. 2013;3:1–6.
Thangamathesvaran L, Canner JK, Scott AW, Woreta FA, Breazzano MP. National emergency department trends for endogenous endophthalmitis: an increasing public health challenge. Eye. 2023;37:1123–9.
Dutta Majumder P. Endogenous fungal endophthalmitis in COVID-19 patients: an unexplored possibility. Indian J Ophthalmol. 2022;70:1083–5.
Kim DY, Moon HI, Joe SG, Kim JG, Yoon YH, Lee JY. Recent clinical manifestation and prognosis of fungal endophthalmitis: a 7-year experience at a tertiary referral center in Korea. J Korean Med Sci. 2015;30:960–4.
Chakrabarti A, shivaprakash MR, Singh R, Tarai B, George VK, Fomda BA, et al. Fungal endophthalmitis: fourteen years’ experience from a center in India. Retina. 2008;28:1400–7.
Edwards JE Jr, Foos RY, Montgomerie JZ, Guze LB. Ocular manifestations of Candida septicemia: review of seventy-six cases of hematogenous Candida endophthalmitis. Medicine. 1974;53:47–75.
Parke DW II, Jones DB, Gentry LO. Endogenous endophthalmitis among patients with candidemia. Ophthalmology. 1982;89:789–96.
Krishna R, Amuh D, Lowder CY, Gordon S, Hall G, Adal K. Should all patients with candidemia have an ophthalmologic examination to rule out ocular candidiasis? Clinical Infect Dis. 1997;25:439.
Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA, Ostrosky-Zeichner L, et al. Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin infect Dis. 2015;62:e1–e50. https://academic.oup.com/cid/article-abstract/62/4/e1/2462830 [Accessed April 22, 2024].
Royal College of Ophthalmologists. Eye care in the intensive care unit (ICU). The Royal College of Ophthalmologists, Ophthalmic services guidance; April 2020. https://www.rcophth.ac.uk/wp-content/uploads/2021/01/Eye-Care-in-the-Intensive-Care-Unit-2020.pdf.
Priluck A, Huang P, Breazzano MP. Outcomes and clinical features predictive of fungal endophthalmitis. Am J Ophthalmol. 2023. https://www.sciencedirect.com/science/article/pii/S0002939423000685 [Accessed October 18, 2024].
Day HR, Bond JB, Gupta B, Saeed K, Breazzano MP. Should routine eye examinations be included in treatment bundles for patients with candidemia? J Infect Dis. 2021, https://academic.oup.com/jid/article-abstract/224/9/1626/6209464 [Accessed September 14, 2024].
Breazzano MP, Bond JB, Bearelly S, Kim DH, Donahue SP, Lum F, et al. American Academy of Ophthalmology recommendations on screening for endogenous Candida endophthalmitis. Ophthalmology. 2022;129:73–76.
Sallam A, Taylor SRJ, Khan A, McCluskey P, Lynn WA, Manku K, et al. Factors determining visual outcome in endogenous Candida endophthalmitis. Retina. 2012;32:1129–34.
Chen KJ, Sun MH, Chen YP, Chen YH, Wang NK, Liu L, et al. Endogenous fungal endophthalmitis: causative organisms, treatments, and visual outcomes. J Fungi. 2022;8:641.
Moussa G, Bassilious K, Mathews N. A novel excel sheet conversion tool from Snellen fraction to LogMAR including ‘counting fingers’, ‘hand movement’, ‘light perception’ and ‘no light perception’ and focused review of literature of low visual acuity reference values. Acta Ophthalmol. 2021; 99: e963–e965. https://onlinelibrary.wiley.com/doi/full/10.1111/aos.14659 [Accessed October 18, 2024].
Tabatabaei SA, Aminzade S, Ahmadraji A, Soleimani M, Sefidan BB, Kasaee A, et al. Early and complete vitrectomy versus tap and inject in acute post cataract surgery endophthalmitis presenting with hand motion vision; a quasi-experimental study. BMC Ophthalmol. 2022;22:16.
Dib B, Morris RE, Oltmanns MH, Sapp MR, Glover JP, Kuhn F. Complete and early vitrectomy for endophthalmitis after cataract surgery: an alternative treatment paradigm. Clin Ophthalmol. 2020;14:1945–54. https://www.tandfonline.com/doi/abs/10.2147/OPTH.S253228 [Accessed April 22, 2024].
Grzybowski A, Turczynowska M, Kuhn F. The treatment of postoperative endophthalmitis: should we still follow the endophthalmitis vitrectomy study more than two decades after its publication? Acta Ophthalmol. 2018;96:e651–e654.
Priluck AZ, Huang P, Breazzano MP. Outcomes and clinical features predictive of fungal endophthalmitis. Am J Ophthalmol. 2023;251:104–14.
Payne JF, Keenum DG, Sternberg P, Thliveris A, Kala A, Olsen TW. Concentrated intravitreal amphotericin B in fungal endophthalmitis. Arch Ophthalmol. 2010;128:1546–50.
Haseeb AA, Elhusseiny AM, Siddiqui MZ, Ahmad KT, Sallam AB. Fungal endophthalmitis: a comprehensive review. J Fungi. 2021;7:996.
Lupia T, Corcione S, Fea AM, Reibaldi M, Fallico M, Petrillo F, et al. Exogenous fungal endophthalmitis: clues to Aspergillus aetiology with a pharmacological perspective. Microorganisms. 2020;9:74.
Schimel AM, Miller D, Flynn HW Jr. Endophthalmitis isolates and antibiotic susceptibilities: a 10-year review of culture-proven cases. Am J Ophthalmol. 2013;156:50–52.
Spadea L, Giannico MI. Diagnostic and management strategies of aspergillus endophthalmitis: current insights. Clinical Ophthalmol. 2019;13:2573–82.
Das T, Agarwal M, Anand AR, Behera UC, Bhende M, Das AV, et al. Fungal endophthalmitis: analysis of 730 consecutive eyes from 7 tertiary eye care centers in India. Ophthalmol Retin. 2022;6:243–51.
Danielescu C, Anton N, Stanca HT, Munteanu M. Endogenous endophthalmitis: a review of case series published between 2011 and 2020. J Ophthalmol. 2020, https://onlinelibrary.wiley.com/doi/abs/10.1155/2020/8869590 [Accessed October 20, 2024].
Nguyen N-H, Nguyen M-P, Nguyen HPT, Mai HK, Do ST, Ho HX, et al. Endogenous endophthalmitis in children: a 5-year retrospective study in Vietnam. J Pediatr Ophthalmol Strabismus. 2025. https://journals.healio.com/doi/abs/10.3928/01913913-20250404-04 [Accessed June 29, 2025].
El-Abiary M, Jones B, Williams G, Lockington D. Fundoscopy screening for intraocular candida in patients with positive blood cultures—is it justified? Eye. 2018. https://www.nature.com/articles/s41433-018-0160-x [Accessed May 5, 2024].
Breazzano MP, Day HR, Bloch KC, Tanaka S, Cherney EF, Sternberg P, et al. Utility of ophthalmologic screening for patients with candida bloodstream infections: a systematic review. JAMA Ophthalmol. 2019;137:698–710.
Ueda T, Takesue Y, Tokimatsu I, Miyazaki T, Nakada-Motokawa N, Nagao M, et al. The incidence of endophthalmitis or macular involvement and the necessity of a routine ophthalmic examination in patients with candidemia. PLoS One. 2019;14:e0216956.
Vena A, Muñoz P, Padilla B, Valerio M, Sanchez MI, Puig-Asensio M, et al. Is routine ophthalmoscopy really necessary in candidemic patients? PLoS One. 2017;12:e0183485.
Danielescu C, Stanca HT, Iorga RE, Darabus DM, Potop V. The diagnosis and treatment of fungal endophthalmitis: an update. Diagnostics. 2022;12:679.
Patel TP, Zacks DN, Dedania VS. Antimicrobial guide to posterior segment infections. Graefe’s Arch Clin Exp Ophthalmol. 2021;259:2473–501.
Patterson TF, Thompson Iii GR, Denning DW, Fishman JA, Hadley S, Herbrecht R, et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016; 63: e1–e60. https://academic.oup.com/cid/article-abstract/63/4/e1/2595039 [Accessed April 22, 2024].
Yoshida M, Kiyota N, Maruyama K, Kunikata H, Toyokawa M, Hagiwara S, et al. Endogenous fusarium endophthalmitis during treatment for acute myeloid leukemia, successfully treated with 25-gauge vitrectomy and antifungal medications. Mycopathologia. 2018;183:451–7.
Rizzello I, Castagnetti F, Toschi PG, Bertaccini P, Primavera L, Paolucci M, et al. Successful treatment of bilateral endogenous Fusarium solani endophthalmitis in a patient with acute lymphocytic leukaemia. Mycoses. 2018;61:53–60.
Acknowledgements
The authors gratefully acknowledge Dr. Kashika Singh, BMBS, BMedSci (Hons), and Dr. Haytham Rezq, who were affiliated with University Hospital Southampton NHS Foundation Trust at the time of data collection, for their valuable contribution to the acquisition of data supporting this work. Dr. Singh is currently affiliated with Worcestershire Acute Hospitals Trust, and Dr. Rezq is currently affiliated with Magrabi Health Hospitals and Centres.
Author information
Authors and Affiliations
Contributions
AW: Organising data, data analysis and statistics, writing the manuscript. DK: Writing the manuscript. BG: Study idea and design. Communication with other centres. Supervising the whole process. Review. MB, KS, DS, AC, RH: Review and revision of manuscript. Southampton data collection team: BG, KS. Newcastle data collection team: RH, KN, IM, MN. St. Thomas’ data collection team: TW, NK. Sunderland data collection team: DS. SUNY, New York data collection team: MB, NG, JH.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Wassef, A., Breazzano, M.P., Saeed, K. et al. Endogenous fungal endophthalmitis: international, multicentre, retrospective analysis of clinical outcomes following surgical and medical management, and screening. Eye 39, 3249–3256 (2025). https://doi.org/10.1038/s41433-025-04061-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-04061-0