Abstract
Objectives
To investigates the associations between various sleep patterns and DR prevalence and incidence.
Methods
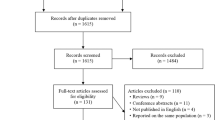
We conducted a multi-stage analysis combining cross-sectional and longitudinal data from UK Biobank (UKB) and Shanghai Cohort of Diabetic Eye Disease (SCODE), alongside two-sample Mendelian randomisation (MR) using genome-wide association study (GWAS) summary statistics. Sleep traits included daytime napping, sleep duration, chronotype, snoring, insomnia, dozing and sleep apnoea. Associations with DR prevalence and incidence were evaluated using logistic and Cox regression models, adjusting for key covariates. Daytime sleepiness was further assessed using the Epworth Sleepiness Scale (ESS). MR analysis employed inverse variance weighting and sensitivity tests to assess causality, heterogeneity, and pleiotropy.
Results
UKB cross-sectional data showed that frequent daytime napping was associated with higher DR prevalence (Usually vs. Never/rarely, adjusted odds ratio [OR] = 1.847, P < 0.001), while SCODE data linked more frequent napping (P = 0.013), longer daytime sleep duration (P = 0.023), and higher Epworth Sleepiness Scale scores (P = 0.046) to higher DR prevalence. Longitudinal analysis found that frequent daytime napping (Usually vs. Never/rarely, hazard ratio [HR] = 2.317, P < 0.001) was associated with DR incidence. Mendelian randomisation analysis suggested a possible link between daytime napping and DR (IVW OR = 1.46, P = 0.04), though this did not withstand multiple testing correction.
Conclusions
Excessive daytime sleepiness may be associated with an increased risk of DR.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
This study utilised data from the UK Biobank (UKB), the Shanghai Cohort for Diabetic Eye Disease (SCODE), and publicly available genome-wide association studies (GWAS). Access to the UK Biobank data is available to bona fide researchers through application via access@ukbiobank.ac.uk and subject to the UKB’s institutional access procedures. Data from the SCODE study are not publicly available but can be obtained from the corresponding author (YM) upon reasonable request and under a formal data use agreement. The SCODE dataset can only be shared for non-commercial academic purposes, and data sharing must comply with relevant Chinese laws and regulations. Summary statistics from GWAS used in this study are publicly accessible and their sources are detailed in the Supplementary Materials.
References
Cheung N, Mitchell P, Wong TY. Diabetic retinopathy. Lancet. 2010;376:124–36.
Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pr. 2014;103:137–49.
Teo ZL, Tham YC, Yu M, Chee ML, Rim TH, Cheung N, et al. Global prevalence of diabetic retinopathy and projection of burden through 2045: systematic review and meta-analysis. Ophthalmology. 2021;128:1580–91.
Jalily PH, Eldstrom J, Miller SC, Kwan DC, Tai SS, Chou D, et al. Mechanisms of action of novel influenza A/M2 viroporin inhibitors derived from hexamethylene amiloride. Mol Pharm. 2016;90:80–95.
Yang S, Zhang J, Chen L. The cells involved in the pathological process of diabetic retinopathy. Biomed Pharmacother. 2020;132:110818.
Duh EJ, Sun JK, Stitt AW. Diabetic retinopathy: current understanding, mechanisms, and treatment strategies. JCI Insight. 2017;2:e93751.
Lim LS, Wong TY. Lipids and diabetic retinopathy. Expert Opin Biol Ther. 2012;12:93–105.
Honasoge A, Nudleman E, Smith M, Rajagopal R. Emerging insights and interventions for diabetic retinopathy. Curr Diab Rep. 2019;19:100.
Lin KY, Hsih WH, Lin YB, Wen CY, Chang TJ. Update in the epidemiology, risk factors, screening, and treatment of diabetic retinopathy. J Diabetes Investig. 2021;12:1322–5.
Wang W, Lo ACY. Diabetic retinopathy: pathophysiology and treatments. Int J Mol Sci. 2018;19:1816.
Yau JWY, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–64.
Microvascular Complications and Foot Care. Standards of medical care in diabetes—2021. Diabetes Care. 2021;44:S151–S67.
Simonson M, Li Y, Zhu B, McAnany JJ, Chirakalwasan N, Sutabutr Vajaranant T, et al. Multidimensional sleep health and diabetic retinopathy: Systematic review and meta-analysis. Sleep Med Rev. 2024;74:101891.
Wei DYW, Chew M, Sabanayagam C. Obstructive sleep apnoea, other sleep parameters and diabetic retinopathy. Curr Diabetes Rep. 2021;21:58.
Zheng Z, Wang C, Li C, Wu Q, Chen X, Chen H, et al. Meta-analysis of relationship of sleep quality and duration with risk of diabetic retinopathy. Front Endocrinol. 2022;13:922886.
Chew M, Tan NYQ, Lamoureux E, Cheng CY, Wong TY, Sabanayagam C. The associations of objectively measured sleep duration and sleep disturbances with diabetic retinopathy. Diabetes Res Clin Pr. 2020;159:107967.
Garcia-Sanchez A, Villalain I, Asencio M, Garcia J, Garcia-Rio F. Sleep apnea and eye diseases: evidence of association and potential pathogenic mechanisms. J Clin Sleep Med. 2022;18:265–78.
Lavie L. Oxidative stress in obstructive sleep apnea and intermittent hypoxia-revisited-the bad ugly and good: implications to the heart and brain. Sleep Med Rev. 2015;20:27–45.
Storti F, Pulley J, Kuner P, Abt M, Luhmann UFO. Circulating biomarkers of inflammation and endothelial activation in diabetic retinopathy. Transl Vis Sci Technol. 2021;10:8.
Irwin MR, Olmstead R, Carroll JE. Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry. 2016;80:40–52.
Catrina SB, Zheng X. Hypoxia and hypoxia-inducible factors in diabetes and its complications. Diabetologia. 2021;64:709–16.
Irwin MR. Sleep and inflammation: partners in sickness and in health. Nat Rev Immunol. 2019;19:702–15.
Irwin MR, Opp MR. Sleep health: reciprocal regulation of sleep and innate immunity. Neuropsychopharmacology. 2017;42:129–55.
García-Sánchez A, Villalaín-Rodes I, Jaureguizar A, Zamarrón E, Martínez-Cerón E, Casitas R, et al. Continuous positive airway pressure effect on progression of retinal disease in patients with sleep apnea and nonproliferative diabetic retinopathy a randomized clinical trial. Ann Am Thoracic Soc. 2024;21:102–13.
Richmond RC, Anderson EL, Dashti HS, Jones SE, Lane JM, Strand LB, et al. Investigating causal relations between sleep traits and risk of breast cancer in women: mendelian randomisation study. BMJ. 2019;365:l2327.
Fan M, Sun D, Zhou T, Heianza Y, Lv J, Li L, et al. Sleep patterns, genetic susceptibility, and incident cardiovascular disease: a prospective study of 385 292 UK biobank participants. Eur Heart J. 2020;41:1182–9.
Liu H, Li L, Zan X, Wei J. No bidirectional relationship between sleep phenotypes and risk of proliferative diabetic retinopathy: a two-sample Mendelian randomization study. Sci Rep. 2024;14:9585.
Jee D, Keum N, Kang S, Arroyo JG. Sleep and diabetic retinopathy. Acta Ophthalmol. 2017;95:41–7.
Zhou M, Li DL, Kai JY, Zhang XF, Pan CW. Sleep duration and the risk of major eye disorders: a systematic review and meta-analysis. Eye. 2023;37:2707–15.
Bycroft C, Freeman C, Petkova D, Band G, Elliott LT, Sharp K, et al. The UK Biobank resource with deep phenotyping and genomic data. Nature. 2018;562:203–9.
Tan NYQ, Chew M, Tham YC, Nguyen QD, Yasuda M, Cheng CY, et al. Associations between sleep duration, sleep quality and diabetic retinopathy. PLoS One. 2018;13:e0196399.
Raman R, Gupta A, Venkatesh K, Kulothungan V, Sharma T. Abnormal sleep patterns in subjects with type II diabetes mellitus and its effect on diabetic microangiopathies: Sankara Nethralaya Diabetic Retinopathy Epidemiology and Molecular Genetic Study (SN-DREAMS, report 20). Acta Diabetol. 2012;49:255–61.
Ba-Ali S, Brondsted AE, Andersen HU, Sander B, Jennum PJ, Lund-Andersen H. Assessment of diurnal melatonin, cortisol, activity, and sleep-wake cycle in patients with and without diabetic retinopathy. Sleep Med. 2019;54:35–42.
Singh R, Undevia NS, Schuman C, Attarian H. Excessive daytime sleepiness among attending physicians: a pilot survey study at an academic institution. Sleep Med. 2011;12:808–10.
Yong Liu AGW, Chapman DP, Cunningham TJ, Lu H, Croft BJ. Prevalence of healthy sleep duration among adults-United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65:137–41.
Wang H, Guo Z, Xu Y. Association of monocyte-lymphocyte ratio and proliferative diabetic retinopathy in the U.S. population with type 2 diabetes. J Transl Med. 2022;20:219.
Huang W, Ma X, Liang H, Li H, Chen J, Fang L, et al. Dietary magnesium intake affects the association between serum vitamin D and type 2 diabetes: a cross-sectional study. Front Nutr. 2021;8:763076.
Altaf QA, Dodson P, Ali A, Raymond NT, Wharton H, Fellows H, et al. Obstructive sleep apnea and retinopathy in patients with type 2 diabetes. A longitudinal study. Am J Respir Crit Care Med. 2017;196:892–900.
Baba A, Zbiba W, Bouayed E, Korbi M, Ghrairi H. Obstructive sleep apnea syndrome. Is it a risk factor for diabetic retinopathy?. J Fr Ophtalmol. 2016;39:139–42.
Banghoej AM, Nerild HH, Kristensen PL, Pedersen-Bjergaard U, Fleischer J, Jensen AE, et al. Obstructive sleep apnoea is frequent in patients with type 1 diabetes. J Diabetes Complications. 2017;31:156–61.
Du C, He C, Dong L, Zheng S, Wang W, Zheng C, et al. Associations of apnea hypopnea index and educational attainments with microvascular complications in patients with T2DM. Endocrine. 2020;67:363–73.
Kaswan R, Bansal R, Katoch D, Dogra M, Singh R, Gupta V, et al. Screening for obstructive sleep apnea in a diabetic retinopathy clinic in a tertiary care center. Indian J Ophthalmol. 2021;69:3349–57.
Grauslund J, Stokholm L, Thykjaer AS, Moller S, Laugesen CS, Andresen J, et al. Inverse cross-sectional and longitudinal relationships between diabetic retinopathy and obstructive sleep apnea in type 2 diabetes: results from a National Screening Program. Ophthalmol Sci. 2021;1:100011.
El Ouardighi H, Poppe KG, Kleynen P, Grabzcan L, Veltri F, Bruyneel AV, et al. Obstructive sleep apnea is not associated with diabetic retinopathy in diabetes: a prospective case-control study. Sleep Breath. 2023;27:121–8.
Jordan AS, McSharry DG, Malhotra A. Adult obstructive sleep apnoea. Lancet. 2014;383:736–47.
Vazir A, Kapelios CJ. Sleep-disordered breathing and cardiovascular disease: who and why to test and how to intervene?. Heart. 2023;109:1864–70.
Liguori C, Maestri M, Spanetta M, Placidi F, Bonanni E, Mercuri NB, et al. Sleep-disordered breathing and the risk of Alzheimer’s disease. Sleep Med Rev. 2021;55:101375.
Cortese R, Adams TS, Cataldo KH, Hummel J, Kaminski N, Kheirandish-Gozal L, et al. Single-cell RNA-seq uncovers cellular heterogeneity and provides a signature for paediatric sleep apnoea. Eur Respir J. 2023;61:2201465.
Meliante PG, Zoccali F, Cascone F, Di Stefano V, Greco A, de Vincentiis M, et al. Molecular pathology, oxidative stress, and biomarkers in obstructive sleep apnea. Int J Mol Sci. 2023;24:5478.
Sivaprasad S, Sen S, Cunha-Vaz J. Perspectives of diabetic retinopathy-challenges and opportunities. Eye. 2023;37:2183–91.
Chang AC, Fox TP, Wang S, Wu AY. Relationship between obstructive sleep apnea and the presence and severity of diabetic retinopathy. Retina. 2018;38:2197–206.
Meng LL, Liu Y, Geng RN, Tang YZ, Li DQ. Association of diabetic vascular complications with poor sleep complaints. Diabetol Metab Syndr. 2016;8:80.
Cudney LE, Frey BN, McCabe RE, Green SM. Investigating the relationship between objective measures of sleep and self-report sleep quality in healthy adults: a review. J Clin Sleep Med. 2022;18:927–36.
Miner B, Stone KL, Zeitzer JM, Han L, Doyle M, Blackwell T, et al. Self-reported and actigraphic short sleep duration in older adults. J Clin Sleep Med. 2022;18:403–13.
Egan KJ, Knutson KL, Pereira AC, von Schantz M. The role of race and ethnicity in sleep, circadian rhythms and cardiovascular health. Sleep Med Rev. 2017;33:70–8.
Wang K, Hu L, Wang L, Shu HN, Wang YT, Yuan Y, et al. Midday napping, nighttime sleep, and mortality: prospective cohort evidence in China. Biomed Environ Sci. 2023;36:702–14.
Dharmastuti DP, Agni AN, Widyaputri F, Pawiroranu S, Sofro ZM, Wardhana FS, et al. Associations of physical activity and sedentary behaviour with vision-threatening diabetic retinopathy in indonesian population with type 2 diabetes mellitus: Jogjakarta Eye Diabetic Study in the Community (JOGED.COM). Ophthalmic Epidemiol. 2018;25:113–9.
Birney E. Mendelian Randomization. Cold Spring Harb Perspect Med. 2022;12:a041302.
Xu F, Li Z, Yang X, Gao Y, Li Z, Li G, et al. Assessment of choroidal structural changes in patients with pre- and early-stage clinical diabetic retinopathy using wide-field SS-OCTA. Front Endocrinol. 2022;13:1036625.
Wong TY, Cheung CM, Larsen M, Sharma S, Simo R. Diabetic retinopathy. Nat Rev Dis Prim. 2016;2:16012.
Um YH, Kim TW, Jeong JH, Hong SC, Seo HJ, Han KD. Association between diabetic retinopathy and insomnia risk: a nationwide population-based study. Front Endocrinol. 2022;13:939251.
Reutrakul S, Park JC, McAnany JJ, Chau FY, Danielson KK, Prasad B, et al. Dysregulated 24 h melatonin secretion associated with intrinsically photosensitive retinal ganglion cell function in diabetic retinopathy: a cross-sectional study. Diabetologia. 2024;67:1114–21.
Okada R, Teramoto M, Muraki I, Tamakoshi A, Iso H. Sleep duration and daytime napping and risk of type 2 diabetes among Japanese men and women: the Japan Collaborative Cohort Study for Evaluation of Cancer Risk. J Epidemiol. 2023;33:562–8.
Sun J, Ma C, Zhao M, Magnussen CG, Xi B. Daytime napping and cardiovascular risk factors, cardiovascular disease, and mortality: a systematic review. Sleep Med Rev. 2022;65:101682.
Guo VY, Cao B, Wong CKH, Yu EYT. The association between daytime napping and risk of diabetes: a systematic review and meta-analysis of observational studies. Sleep Med. 2017;37:105–12.
Yamada T, Shojima N, Yamauchi T, Kadowaki T. J-curve relation between daytime nap duration and type 2 diabetes or metabolic syndrome: a dose-response meta-analysis. Sci Rep. 2016;6:38075.
Xu YX, Pu SD, Zhang YT, Tong XW, Sun XT, Shan YY, et al. Insulin resistance is associated with the presence and severity of retinopathy in patients with type 2 diabetes. Clin Exp Ophthalmol. 2024;52:63–77.
Garcia-Llorca A, Kararigas G. Sex-related effects of gut microbiota in metabolic syndrome-related diabetic retinopathy. Microorganisms. 2023;11:447.
Alomar SY, Barakat BM, Eldosoky M, Atef H, Mohamed AS, Elhawary R, et al. Protective effect of metformin on rat diabetic retinopathy involves suppression of toll-like receptor 4/nuclear factor-k B expression and glutamate excitotoxicity. Int Immunopharmacol. 2021;90:107193.
Chen B, Shen C, Sun B. Current landscape and comprehensive management of glycemic variability in diabetic retinopathy. J Transl Med. 2024;22:700.
Forrester JV, Kuffova L, Delibegovic M. The role of inflammation in diabetic retinopathy. Front Immunol. 2020;11:583687.
Jakubowski KP, Hall MH, Marsland AL, Matthews KA. Is daytime napping associated with inflammation in adolescents?. Health Psychol. 2016;35:1298–306.
Devine JK, Wolf JM. Integrating nap and night-time sleep into sleep patterns reveals differential links to health-relevant outcomes. J Sleep Res. 2016;25:225–33.
Basta M, Koutentaki E, Vgontzas A, Zaganas I, Vogiatzi E, Gouna G, et al. Objective daytime napping is associated with disease severity and inflammation in patients with mild to moderate dementia1. J Alzheimers Dis. 2020;74:803–15.
Mantua J, Spencer RMC. The interactive effects of nocturnal sleep and daytime naps in relation to serum C-reactive protein. Sleep Med. 2015;16:1213–6.
Deantoni M, Reyt M, Baillet M, Dourte M, De Haan S, Lesoinne A, et al. Napping and circadian sleep-wake regulation during healthy aging. Sleep. 2024;47:zsad287.
Mesas AE, Sanchez-Lopez M, Pozuelo-Carrascosa DP, Sequi-Dominguez I, Jimenez-Lopez E, Martinez-Vizcaino V. The role of daytime napping on salivary cortisol in children aged 0-5 years: a systematic review and meta-analysis. Eur J Pediatr. 2022;181:1437–48.
Leong RLF, Tian L, Yu N, Teo TB, Ong JL, Chee MWL. Bidirectional associations between the duration and timing of nocturnal sleep and daytime naps in adolescents differ from weekdays to weekends. Sleep. 2024;47:zsae147.
Do MTH. Melanopsin and the intrinsically photosensitive retinal ganglion cells: biophysics to behavior. Neuron. 2019;104:205–26.
Ko GY. Circadian regulation in the retina: from molecules to network. Eur J Neurosci. 2020;51:194–216.
Liu WJ, Chen JY, Niu SR, Zheng YS, Lin S, Hong Y. Recent advances in the study of circadian rhythm disorders that induce diabetic retinopathy. Biomed Pharmacother. 2023;166:115368.
Ling F, Zhang C, Zhao X, Xin X, Zhao S. Identification of key genes modules linking diabetic retinopathy and circadian rhythm. Front Immunol. 2023;14:1260350.
Stenvers DJ, Scheer F, Schrauwen P, la Fleur SE, Kalsbeek A. Circadian clocks and insulin resistance. Nat Rev Endocrinol. 2019;15:75–89.
Fagiani F, Di Marino D, Romagnoli A, Travelli C, Voltan D, Di Cesare Mannelli L, et al. Molecular regulations of circadian rhythm and implications for physiology and diseases. Sig Transduct Target Ther. 2022;7:41.
Thorarinsdottir EH, Pack AI, Gislason T, Kuna ST, Penzel T, Yun Li Q, et al. Polysomnographic characteristics of excessive daytime sleepiness phenotypes in obstructive sleep apnea: results from the international sleep apnea global interdisciplinary consortium. Sleep. 2024;47:zsae035.
Dai W, Tham YC, Cheung N, Yasuda M, Tan NYQ, Cheung CY, et al. Macular thickness profile and diabetic retinopathy: the Singapore Epidemiology of Eye Diseases Study. Br J Ophthalmol. 2018;102:1072–6.
Bhaskaran A, Babu M, Sudhakar NA, Kudlu KP, Shashidhara BC. Study of retinal nerve fiber layer thickness in diabetic patients using optical coherence tomography. Indian J Ophthalmol. 2023;71:920–6.
Gong X, Wang W, Xiong K, Wang L, Li W, Li Y, et al. Associations between peripapillary retinal nerve fiber layer and choroidal thickness with the development and progression of diabetic retinopathy. Invest Ophthalmol Vis Sci. 2022;63:7.
Yusuf FLA, Tang TS, Karim ME. The association between diabetes and excessive daytime sleepiness among American adults aged 20-79 years: findings from the 2015-2018 National Health and Nutrition Examination Surveys. Ann Epidemiol. 2022;68:54–63.
Griggs S, Hickman RL, Strohl KP, Redeker NS, Crawford SL, Grey M. Sleep-wake characteristics, daytime sleepiness, and glycemia in young adults with type 1 diabetes. J Clin Sleep Med. 2021;17:1865–74.
Funding
This work was supported by the National Key Research and Development Program of China (2021YFC2702100), the Key Disciplinary Projects of the 3-year Action Plan to Strengthen the Construction of the Public Health System in Shanghai (GWVI-11.1-30), the Science and Technology Commission of Shanghai Municipality (23ZR1481000), the Shanghai Municipal Health Commission (2022YQ051), Shanghai Engineering Research Centre of Precise Diagnosis and Treatment of Eye Diseases (19DZ2250100), and Shanghai “Rising Stars of Medical Talent” Youth Development Program.
Author information
Authors and Affiliations
Contributions
Conceptualisation, XZ, SL, LL, YX, HZ and YM; Methodology, SL, LL, YX, HZ and YM; Formal Analysis, XZ, SL, and YM; Investigation, SL, LL, YX, HZ and YM; Resources, SL, LL, YX, HZ and YM; Data Curation, SL, LL, YX, HZ and YM; Writing – Original Draft, XZ, SL, and YM; Writing – Review & Editing, all authors; Visualisation, LL, YX, HZ and YM; Supervision, SL, LL, YX, HZ and YM; Project Administration, SL, LL, YX, HZ and YM; Funding Acquisition, HZ.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41433_2025_4066_MOESM1_ESM.docx
Supplementary materials of "Associations between Sleep Patterns and Diabetic Retinopathy: Insights from Cross-Sectional and Longitudinal Evidence"
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhao, X., Lin, S., Lu, L. et al. Associations between sleep patterns and diabetic retinopathy: insights from cross-sectional and longitudinal evidence. Eye 39, 3314–3323 (2025). https://doi.org/10.1038/s41433-025-04066-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-04066-9