Abstract
Objectives
To investigate the biomechanical changes and associated factors of SMILE-derived lenticules under various preservation conditions.
Methods
A total of 520 corneal stromal lenticules of 260 patients (male: female 98:162, age 28.54 ± 5.98 years, mean spherical error –4.47 ± 1.63 D) were derived during small incision lenticule extraction (SMILE) surgeries, and were stored in glycerol, silicone oil, Optisol and cryopreservation for 1 day, 1 week or 1 month. Spherical error, cylindrical error as well as other main parameters were evaluated. A nanoindenter system was used to measure the effective Young’s modulus of each lenticule. Changes in effective Young’s modulus were evaluated in each group among all time points.
Results
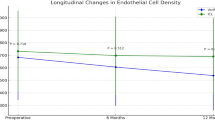
There was no statistical significance in effective Young’s moduli of lenticules in the glycerol group among all preservation times, while the lowest effective Young’s modulus appeared when preserved for 1 month, 1 week, and 1 day in the silicone oil, Optisol, and cryopreservation group. Among all factors observed, the spherical error of SMILE-derived lenticules was a positive influencing factor on their biomechanics (P = 0.04*).
Conclusions
It is feasible to maintain biomechanical stability of SMILE-derived lenticules in glycerol in the short term. Thickness is a positive influencing factor on the biomechanics of SMILE-derived lenticules.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Han T, Zhao F, Chen X, Miao H, Chen Z, Zhou X. Evaluation of disk halo size after small incision lenticule extraction (SMILE). Graefes Arch Clin Exp Ophthalmol. 2019;257:2789–93.
Han T, Zheng K, Chen Y, Gao Y, He L, Zhou X. Four-year observation of predictability and stability of small incision lenticule extraction. BMC Ophthalmol. 2016;16:149.
Miao H, Tian M, Xu Y, Chen Y, Zhou X. Visual outcomes and optical quality after femtosecond laser small incision lenticule extraction: an 18-month prospective study. J Refract Surg. 2015;31:726–31.
Liu YC, Williams GP, George BL, Soh YQ, Seah XY, Peh GSL, et al. Corneal lenticule storage before reimplantation. Mol Vis. 2017;23:753–64.
Abd Elaziz MS, Zaky AG, El SaebaySarhan AR. Stromal lenticule transplantation for management of corneal perforations; one year results. Graefes Arch Clin Exp Ophthalmol. 2017;255:1179–84.
Yin H, Qiu P, Wu F, Zhang W, Teng W, Qin Z, et al. Construction of a corneal stromal equivalent with SMILE-derived lenticules and fibrin glue. Sci Rep. 2016;6:33848.
Liu S, Zhang X, Zhou X. Toric lenticule implantation for correction of hyperopia and astigmatism following small incision lenticule intrastromal keratoplasty with the triple marking method. J Refract Surg. 2022;38:82–8.
Lazaridis A, Reinstein DZ, Archer TJ, Schulze S, Sekundo W. Refractive lenticule transplantation for correction of iatrogenic hyperopia and high astigmatism after LASIK. J Refract Surg. 2016;32:780–6.
Liang G, Wang L, Pan Z, Zhang F. Comparison of the different preservative methods for refractive lenticules following SMILE. Curr Eye Res. 2019;44:832–9.
Xia F, Zhao J, Fu D, Xu Y, Yao P, Li M, et al. Optical transmittance and ultrastructure of SMILE-derived lenticules subjected to three different preservative methods. Exp Eye Res. 2020;201:108357.
Shang Y, Li Y, Wang Z, Sun X, Zhang F. Risk evaluation of human corneal stromal lenticules from SMILE for reuse. J Refract Surg. 2021;37:32–40.
Xia F, Zhao J, Fu D, Qin B, Chen Z, Zhao Y, et al. Comparison of the effects of temperature and dehydration mode on glycerin-based approaches to SMILE-derived lenticule preservation. Cornea. 2022;41:470–7.
Xue C, Xiang Y, Shen M, Wu D, Wang Y. Preliminary investigation of the mechanical anisotropy of the normal human corneal stroma. J Ophthalmol. 2018;2018:5392041.
Xiang Y, Shen M, Xue C, Wu D, Wang Y. Tensile biomechanical properties and constitutive parameters of human corneal stroma extracted by SMILE procedure. J Mech Behav Biomed Mater. 2018;85:102–8.
Miao H, He L, Shen Y, Li M, Yu Y, Zhou X. Optical quality and intraocular scattering after femtosecond laser small incision lenticule extraction. J Refract Surg. 2014;30:296–302.
Xu P, Londregan A, Rich C, Trinkaus-Randall V. Changes in epithelial and stromal corneal stiffness occur with age and obesity. Bioengineering. 2020;7:14–24.
Zhang H, Deng Y, Li Z, Tang J. Update of research progress on small incision lenticule extraction (SMILE) lenticule reuse. Clin Ophthalmol. 2023;17:1423–31.
Nohava J, Swain M, Lang SJ, Maier P, Heinzelmann S, Reinhard T, et al. Instrumented indentation for determination of mechanical properties of human cornea after ultraviolet-A crosslinking. J Biomed Mater Res A. 2018;106:1413–20.
Wang C, Shen M, Song Y, Chang L, Yang Y, Li Y, et al. Biaxial hyperelastic and anisotropic behaviors of the corneal anterior central stroma along the preferential fibril orientations. Part II: quantitative computational analysis of mechanical response of stromal components. J Mech Behav Biomed Mater. 2023;142:105802.
Polachova M, Netukova M, Benada O, Kucera T, Kolin V, Baxant AD, et al. The new future perspective in corneal tissue utilisation - methods of preparation and preservation. BMC Ophthalmol. 2023;23:294.
Nemcokova M, Dite J, Klimesova YM, Netukova M, Studeny P. Preservation of corneal stromal lenticule: review. Cell Tissue Bank. 2022;23:627–39.
Mohamed-Noriega K, Toh KP, Poh R, Balehosur D, Riau A, Htoon HM, et al. Cornea lenticule viability and structural integrity after refractive lenticule extraction (ReLEx) and cryopreservation. Mol Vis. 2011;17:3437–49.
Romano V, Levis HJ, Gallon P, Lace R, Borroni D, Ponzin D, et al. Biobanking of dehydrated human donor corneal stroma to increase the supply of anterior lamellar grafts. Cornea. 2019;38:480–4.
Seiler TG, Shao P, Frueh BE, Yun SH, Seiler T. The influence of hydration on different mechanical moduli of the cornea. Graefes Arch Clin Exp Ophthalmol. 2018;256:1653–60.
Hatami-Marbini H, Etebu E. Hydration dependent biomechanical properties of the corneal stroma. Exp Eye Res. 2013;116:47–54.
Germann JA, Martinez-Enriquez E, Marcos S. Quantization of collagen organization in the stroma with a new order coefficient. Biomed Opt Express. 2018;9:173–89.
Zhao J, Zhang Z, Xia F, Li G, Saiding Q, Xiang L, et al. Nutrient capsules maintain tear film homeostasis for human corneal lenticule transplantation. Chem Eng J. 2022;450;138078.
Acknowledgements
The authors appreciate the contributions of all patients, as well as the support from all stuff in Eye and ENT Hospital of Fudan University.
Funding
National Key Research and Development Program of China (2023YFA0915000 (04)). National Natural Science Foundation of China (82371096). Project of Shanghai Science and Technology (20410710100). Shanghai Engineering Research Center of Laser and Autostereoscopic 3D for Vision Care (20DZ22550005) Sailing Program of Shanghai Science and Technology Commission (22YF1405900).
Author information
Authors and Affiliations
Contributions
XH collected the data with BS and drafted the manuscript. XZ contributed to design of methodology. JZ analysed the data. ML and HX supervised and revised the manuscript for critical review. XZ and ML contributed to the conceptualisation.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Han, X., Sun, B., Zhang, X. et al. Biomechanical changes and associated factors of preserved SMILE-derived corneal stromal lenticules. Eye 40, 201–206 (2026). https://doi.org/10.1038/s41433-025-04115-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-04115-3